Tubulointerstitial nephritis
advertisement
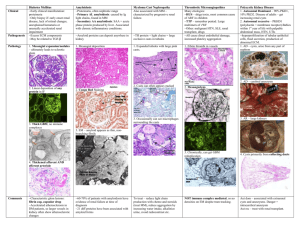
Tubulointerstitial nephritis Lívia Jánoskuti Definition • Kidney diseases that involve structures in the kidney outside the glomerulus • Tubules and/ or the interstitium • Tubules are responsible for concentrating the urine(osmolality, sodium and water reabsorption) • Reduction of tubular or interstitial function both result in: impaired resorptive capacity • Isosthenuria:urin osm. the same as blood < 350 mosmol/kg Characteristics of tubulointerstitial and glomerural diseases Tubular Glomerular Urine osmolality Low <350mos/kg High/norm Urine sodium >40mM/L <40 U. sediment hematuria Muddy brown Red cell casts casts(ATN) Eosinophils(AAIN) rare common proteinuria rare common Causes Concom.illness Drugs common Autoimmun or congen. Therapy Supportive/dialysis Steroids,immunmo Eosinophils and eo.in casts in urine sediment (Hansel’s stain) Muddy brown casts pigmented granular casts Pathophysiology • Lethal, sublethal injuri to renal cells lead to expression of new local antigens, inflammatory cell infiltration and activation of proinflammatory cells and cytokines • Acute- renal tubular dysfunction with or without renal failure ( If the tubular basement mebrane is preserved- reversibile) • Chronic- interstitial scarring fibrosis, tubule atrophy- resulting progressive renal failure Clinical presentation Acute • Abruptly, within days of exposure to the offending agent • Uremic symptoms: oliguria Acute tubulointerstitial diseases • • • • • • • • • Acute tubular necrosis(ATN) Contrast nephropathy Acute allergic tubulointerstitial nephritis(AAIN) Atheroembolic renal insuff. Pigment mediated renal insuff. Crystal mediated renal insuff. Myeloma related renal insuff. Toxin mediated renal insuff. Papillary necrosis. Acute tubular necrosis • Cause:hypotension or sepsis • Sy: azotemia as incidental findings • Dg: U osm-L,UNa –H,FENa-H BUN/cr –L muddy brown casts • Th:supportive observation electrolytes, mental status, fluid overload, -dialysis Lab. Findings distinguishing ATN from prerenal azotemia prenrenal ATN U Na mM/L <20 >40 FE Na <1% >1% U osm mM/kg >500 <350 BUN/creat >20:1 10-15:1 U sediment Hyalin casts Brown casts Contrast nephropathy • Progressive rise in Se creat 24-48 h after radiocontrast is given • Risk factors: older age, DM, HF,MM. preexisting chr.kidney disease,liver failure • Th:supportive • Prevention:avoiding contrast(when possible), low dose low osmolality contrast agent use, isotonic fluid infusion 1ml/kg/h 6-12h before and after the contrast,600mgacetylcystein pos before the day and the day of contrast Acute Allergic Interstitial Nephritis(AAIN) Causes(many): drugs(allopurinol,penicillin, quinolons, sulfas, rifampicin) infection,autoimmune disease Sy:shortly after the first dose;fever,rash Dg:eosinophilia, eosinophils in u.sediment.IgE elev Th:stop offending agent, renal f. control, • no sign of improvement within few days- 1mg/kg prednisolon for 4-6 weeks with rapid tapering of the dose Atheroembolic kidney disease • Cause:multiple small infarctions of renal parenchyma secondary to recent vascular procedure ( angio, PTCA) • (cholesterol crystals lodge in small/medium sized arteries) • Sy: bluish skin discolor., livedo reticularis • uremic sy.Hollenhorst plaques in optic fundi • Dg.retrospective • Th: no therapy Livedo reticularis Blue toe syndrome Hollenhorst plaques ( bright plaques in the retinal arterioles Pigment mediated RI. Cause: -rhabdomyolysis(traumatic crush injury, muscle ischaemia,seizures, statins,NSAID, cocaine overdose), -intravasc. hemolysis ( blood transfusion reaction) Sy: very dark urin, uremic sy. Dg: Hbg, myoglobin in urine, CPK,Se K Th:ICU- hyperK-Ca gluconate iv, osmotic diuresis(mannitol), alkalization( sodium bicarb)can reduce liklehood of renal insuff. Gross hemoglobinemia and hemoglobinuria Crystal mediated RI. Cause: 1.Oxalate crystals (ethylen glycol toxicity,methoxyflurane anaesthesia, Crohn s disease) 2.urate crystals –tumor lysis syndr., primary, sec. hyperuricaemia if the urine concentrated Dg:history 1.envelope shaped crystals , anion gap metabol.acidosis(Na)-(Cl+HCO3)>11mEq/L 2.Hyperuricaemia, diamond shaped crystals Th: 1.aggressive hydration+10% ethanol 7,5mg/kg iv for ADH enzime competition 2.aggressive hydration + allopurinol Myeloma-related RI. Cause:overproduction of monoclonal Ig light chain( Bence Jones protein) by pathologic B cell clonal population Sy: MM and uremic Dg. 24h urin protein ELFO Th: MM therapy. Toxin mediated RI Cause : drugs, but not occure after the first dose (NSAID,aminoglycoside, amphotericinB, cisplatin, cephalopsorins, cyclosporin) Sy: uremic, following longer term th.(daysweeks) No fever, no rash Th:dependent on drug. Prevention: ensure widest spacing of dose, estimation of drug plasma levels Papillary necrosis Cause: NSAID, acetaminophen ingestion in patients with DM, liver cirrhosis, sickle cell disease Sy: fever,flank pain( appears like UTI) Dg: no WBC or elevated nitrits in urin. Elevated serum WBC Confirm with spiral CT. Th: stop offending drug. Prevention: avoid excessive use of NSAID Principal mechanism in acute tubulointerstitial nephritis • Hypersensitive reaction to drugs (penicillin, NSAID, sulfa drugs) • Infection (viral, bacterial, parasitic) often associated with obstruction or reflux • Autoimmun mechanism • Vasomotor nephropathy (afferent arteriola constriction) • Intratubular obstruction (pigment, crystal, protein) • Direct toxic effect on tubular epithelium Clinical presentation 2.Chronic • • • • • • • • • Drugs (analgetics, lithium, cylosporin, tacrolimus) Heavy metals ( lead, cadmium, mercury) Obstructive uropathy, nephrolithiasis, reflux disease Immunologíc diseases( lupus, Sjögren,sarcoidosis, vasculitis, chr. transplant rejection Neoplasia ( myeloma, amyloidosis, leukemia) Atherosclerotic kidney diseases Metabolic ( hyperCa,potassium depletion, cystinosis) Genetics( Alport sy, medullary cystic diseases Miscellaneous ( Balkan endemic nephropathy) Epidemiology • 10-15% of all kidney diseases • Analgesic nephropathy is 5-6 times more common in women • All toxic nephropathies are observed more frequently with adavancing age (cummulative effects) Clinical presentation Chronic • Insidious nature • Often diagnosed incidentally on routine laboratory screening, or evaluation of hypertension • Modest proteinuria, sterile pyuria, anemia, renal insuff ( NSAID) • Polyuria concentration defect (lithium) • Modest proteinuria, hyperK renal tub. acidosis in chr. obstruction • Arterioscler. kidney: modest proteinuria, kreatinin and BUN elevation, hypertension Laboratory • BUN , kreatinin- renal failure • Low bicarbonate < 24 mEq L- acidosisph<7,35 With hypoK – proximal tub. disorder With hyperK- distal tub disoreder • Urinalysis: hematuria and pyuria with-or without bacteria, casts, eosinophils, crystals • Urine protein usually less >1-2 gr/24h • Protein ELFO- low mol. weight (beta-2 microglob,alfa-1 microglob., light chains) Imaging US/ and flat plate kidney- hydronephrosis, renal calculi • Normal kidney size favours acute • Small kidneys with increased echogenicity- chr . disease Iv pyelography usually not indicated- contrast damage CT(high resolutional) scan show microcalcifications in renal papillary tipsdiagnosing analgesic nephropathy Nephrosclerosis CT Hydronephrosis US Analgesic nephropathy CT microcalcifications Management of chr. Tubulointerstitial disease • Depends on the etiology- generally stop of the offending drug and supportive measures-blood pressure and anemia control • Analgesic- increased uroepitheal cc • Lead- chelation th. with EDTA • Atheroscler.- no specific th.-smoking cessation, cholesterol diet and statins • Reflux nephropathy, urinary tract obstruction:surgical treatment, antibiotics Lead nephroptahy diagnosis • Bone lead content by radiographic fluorescensce • EDTA lead mobilizatiion test: after iv/im 2 g EDTA( calcium disonium versenate) 24h urine lead exretion->0,6 g- abnormal • Basophil puncture in RBC Prognosis • Most patients with allergic inerstitial nephritis recover upon cessation of the offending agent • Cholesterol microembolic diseases have some spontaneous improvement, complete resolution is rare • Chr. Tubulointerstitial d. progresses to ESRD.