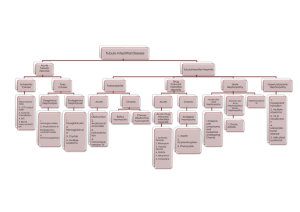
Tubulointerstitial Diseases: Types, Mechanisms, Clinical Aspects
advertisement

TUBULOINTERSTITIAL DISEASES Al-Absi, M.D. TUBULOINTERSTITIAL DISEASES • Tubulointerstitial nephritis: – Primary - Inflammation limited to tubules & with uninvolved – – – – or minimally involved glomeruli/vessels. • Acute - Sudden onset & rapid decline in renal function associated with interstitial edema • Chronic - Protracted onset and slow decline in renal function associated with interstitial fibrosis Secondary - Tubulointerstitial inflammation associated with primary glomerular/vascular diseases Infectious – Tubulointerstitial inflammation associated with presence of live microorganism Idiopathic – Tubulointerstitial nephritis where etiological agents or causes are not known Reactive – Tubulointerstitial inflammation from the effects of systemic inflammation. Kidney is sterile. TUBULOINTERSTITIAL DISEASES • Urinary tract infection – colonization of excretory system by live microorganism – Pyelonephritis: tubulointerstitial nephritis with pelvis and calyceal involvement • Acute - usually suppurative inflammation involving pelvi-calyceal system and parenchyma • Chronic - involvement of pelvi-calyceal system and parenchyma with prominent scarring Tubulointerstitial Nephropathy • Two distinct clinical presentations and course of development: (1) acute (2) chronic • Immunologic mechanisms often involved in pathogenesis regardless of underlying cause • Histologic changes evident on microscopy are not specific for a given etiology Immunologic Mechanisms in Tubulointerstitial Nephropathy • Drug acting as hapten binding to tubulointerstitial parenchyma, making the latter immunogenic • Drug-induced damage through toxic mechanisms, producing nephritogenic neoantigens • Molecular mimicry by infectious agents inducing cross-reactive immune response Acute Tubulointerstitial Nephropathy • Drug-induced acute renal failure allergic tubulointerstitial nephritis nephrotoxic tubular injury • Acute bacterial pyelonephritis • Metabolic disorders hypercalcemia hyperuricosuria • Environmental factors Morphologic Features of DrugInduced ATIN • Increased interstitial volume due to: mononuclear cell infiltration lymphocytes, plasma cells, macrophages, granulomatous reaction, eosinophiles interstitial edema • Tubular injury characterized by: disruption of tubular basement membranes epithelial cell necrosis Chronic Tubulointerstitial Nephropathy • Drug-induced analgesics, cyclosporine, antineoplastic agents • Infection-related chronic bacterial pyelonephritis vesicoureteral reflux obstructive uropathy • Autoimmunity SLE, Sjogren’s Disease Morphologic Features of Chronic TIN • Interstitial fibrosis with less prominence of cellular infiltrates • Decreased vascularity due to reduced volume of capillaries • Tubular atrophy • Secondary glomerulosclerosis Clinical Evidence of Tubular Dysfunction in TIN • Renal glucosuria and amino aciduria • Hypophosphatemia • Hyperchloremic acidosis Hypokalemia Hyperkalemia • Reduced urine concentrating ability • Sodium wasting • Pyuria and urine epithelial cells UTI and Pyelonephritis •Acute versus Chronic •Ascending versus Hematogenous •Bacterial Adhesion • Vesicoureteral reflux UTI and Pyelonephritis • Asymptomatic & symptomatic • Pathology: Interstitial edema, and inflammation • Chronic Pyelonephritis and Reflux Clinical Aspects of TIN Related to Specific Drugs or Other Causes • Drugs beta lactam derivative antibiotics NSAIDS analgesics aminoglycosides • Environmental agents • Alternative medications • Bacteria Acute Tubulointerstitial Nephritis Induced by Beta-Lactam Derivatives • Duration of drug administration may vary from few days to several weeks; not dose-dependent • Clinical manifestations: fever, rash, eosinophilia, oliguric or non-oliguric renal failure • Urinary findings: hematuria (microscopic or gross), pyuria, proteinuria, eosinophiluria Acute Tubulointerstitial Nephritis Induced by BetaLactam Derivatives • Pathogenesis: possible immunemedicated • Pathology: Enlarged kidney, IS inflammation • Clinical Course Tubulointerstitial Nephritis Induced by Non-steroidal Antiinflammatory Drugs Usually occurs after prolonged drug administration and may present as: • Acute impairment of renal function with nonnephrotic range proteinuria, hyperkalemia and other evidence of tubular dysfunction • Clinical manifestations similar to those above, but with nephrotic range proteinuria • Nephrotic syndrome without other evidence of renal impairment Analgesic Abuse Nephropathy • Initial occurrence reported in association with phenacetin abuse • Has been associated with long term use of analgesic mixtures containing phenacetin (?acetaminophen) and aspirin or other non-steroidal anti-inflammatory drugs • Drug accumulates and is highly concentrated in the renal medullary interstitium Analgesic Abuse Nephropathy Clinical features: • Slow progressive impairment of renal function • Tubular dysfunction characterized by the development of hyperkalemic, hyperchloremic renal tubular acidosis and nephrogenic diabetes insipidus • Impairment of sodium reabsorption •May progress to the development of papillary necrosis •Uro-epithelia cancer Aminoglycoside Nephrotoxicity • Recognized potential for causing acute renal failure in hospitalized patients • Drug enters the tubular lumen by glomerular filtration and is reabsorbed by proximal tubules where tubule cell injury leading to necrosis may occur. • Manifested clinically by progressive increase in serum creatinine, renal K+ and Mg++ wasting, renal glucosuria Cystic Diseases • Cyst Formation: large fluid-filled pouches • Causes • PKD PKD • Autosomal dominant or recessive • Prevalence • ADPKD1, and ADPKD2 PKD • Pathology • Other organs involvment • Prognosis: ADPKD2 is worse Acquired cystic disease • Pathogenesis • Organs involved • Long term risks Balkan Endemic Nephropathy: Clinical Features • Slowly progressive renal insufficiency • Urine sediment usually unremarkable • Proteinuria usually <1.0 g/day • Renal tubular dysfunction • Hypertension in <25% of patients • Gross hematuria: may be a sign of uroepithelial tumor Chinese Herbs Nephropathy • Rapidly progressive interstitial nephropathy attributed to weight-reducing diets containing Chinese herbs • Renal pathology closely resembling the characteristic lesions of Balkan Endemic Nephropathy • Multiple foci of cellular atypia in the renal pelvis and ureters •Aristolochic acid, a known carcinogen and suspected etiologic agent