Preterm Labor - Avera Health
advertisement

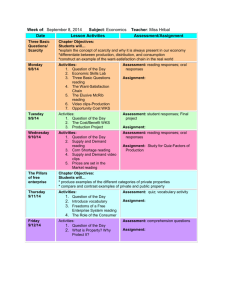
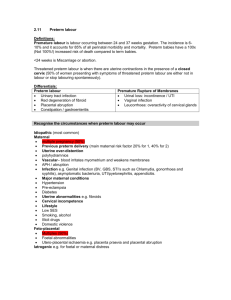
Preterm Labor Preterm Labor • Guidelines for Perinatal Care, 2012 – Preterm labor generally can be defined as regular contractions that occur before 37 weeks of gestation and are associated with changes in the cervix. Scope of the Issue • 12.5% in 2005 (30% increase from 1981) – slight singleton births, significant rise due to in multiple gestations – Twins 55%risk PTB, triplets 90% • PTB causes 75% of neonatal deaths not caused by congenital anomalies – 1999, prematurity became leading cause of neonatal mortality, accounts for 23% of deaths in first month of life South Dakota and US, 1995-2005 Preterm birth Preterm is less than 37 completed weeks gestation. Source: National Center for Health Statistics, final natality data. Retrieved October 2, 2007, from www.marchofdimes.com/peristats. South Dakota, 2005 >37 wks 32-26 wks < 32 wks 10,143 births 1,156 births 158 births Prematurity/LBW accounts for 8.1% of SD infant deaths Cost of PTL/PTB • Does not account for life-long deficits associated w/PTB (< 32 wks) – cerebral palsy, mental retardation, chronic lung disease, vision and hearing loss Etiology • 50% of patients with preterm labor have no risk factors • Risk Factors – Medical/Obstetric – Current Pregnancy – Demographic/Behavioral/Other • Overall, ~20% of PTB are medically indicated due to pregnancy complications or health problems in mom or baby. 3 Groups with Highest Risk • Women who have had a previous preterm birth • Women who are pregnant with twins, triplets, or more • Women with certain uterine or cervical abnormalities Medical Risks Predating This Pregnancy • • • • • • Hx prior PTB (triples risk) 3 or more abortions/miscarriages Uterine anomalies Low pre-preg. weight for height Parity (0 or > 4) Pre-existing conditions (DM, HTN) Current Pregnancy Risks • Uterine distension (multiples, hydramnios) • Maternal infection (incl. untreated vaginal infections & UTI’s) • Incompetent cervix • Short inter-pregnancy interval (i.e. < 6-9 months between pregnancies) • Bleeding in 1st trimester Current Pregnancy Risks (cont) • • • • • Placenta previa or abruptio Anemia Fetal anomalies PROM Abdominal surgery Demographic Risks • Maternal Age < 17 or > 35 • Non-white – Black - 17.5% – Hispanic - 11.4% – White - 11% • Low socio-economic status • Unmarried • Low level education Behavioral Risks • Smoking ( risk by 40%) • Poor nutrition, poor weight gain – risk of LBW infant by 60% and risk PTB 60% • • • • • • Alcohol ( risk 40%) Other substance abuse Pre-pregnancy weight < 100 lbs Late or no prenatal care Occupational & environmental factors Domestic violence Other Risks • Stress • Long working hours with long periods of standing • Inability to rest • Lack of social support • However, the best predictor of having a preterm birth is a history of preterm delivery or prior LBW infant – 1 prior PT delivery --- 2x risk – 2 prior PT deliveries – 4x risk Maternal Effects • Psychological Stress – Threat of Preterm Delivery – Fear for Self and Baby – Potential for Long-Term Bedrest • Physical Stress – Prolonged Bedrest – Medications Fetal/Neonatal Effects • Fetal – Tocolytics – Risk of Birth Trauma • Neonatal – Intraventricular Hemorrhage (IVH) – Respiratory Distress Syndrome (RDS) – Patent Ductus Arteriosus (PDA) – Necrotizing Enterocolitis (NEC) – Other Physiology of Labor • Cervical Ripening – Cervical connective tissue changes – Cervical softening & shortening – Prostaglandins stimulate ripening • Uterine Contractions – Estrogen – Progesterone • Prostaglandins Preterm Labor • Cause often related to factors that stimulate the release of prostaglandins – Infection – Uterine over-distention – Decreased uterine blood flow Signs/Symptoms • Contractions q. 10 min. or more often (may be painless) • Low, dull backache • Menstrual-like cramps • Cramps with or without diarrhea – Thigh pain – Pelvic pressure/heavy feeling – Abdominal/intestinal cramping Signs/Symptoms • Change/increase in vaginal discharge (clear, pink, brownish) • Leaking vaginal fluid • Feeling baby is pushing down • Feeling bad • Remember, Palpate for UC’s don’t rely on EFM! Assessment • Diagnostic Testing – CBC – Urinalysis – Cervical assessment (speculum, U/S) – Amniocentesis (culture, L/S ratio, Lamellar Body Count [LBC]) – Fetal Fibronectin (fFN) – Saliva Test Cervical Length Assessment • Cervical length < 30 mm per ultrasound seems to predict PTL – Only accurate up to ~ 30 wks gestation – After 30 wks, short cervix may not mean PTL risk • To compare cervical length, at least 2 ultrasounds should be done • Expensive to do • May be beneficial for women at risk for PTL/PTB Amniocentesis • Removal of amniotic fluid via U/S for fluid analysis (L/S ratio, cultures, chromosomes) • L/S – lecithin/sphingomyelin; ratio of 2.0 or higher indicates lung maturity • PG – phosphatidtyl glycerol (if present, indicates lung maturity) Lamellar Body Count • New method for testing FLM, results in 30 minutes (L/S 4 hours) • Can only be run on clear fluid (do L/S if meconium or blood in fluid) • Results interpretation: – <20 = immature – 21-24 = intermediate – >25 = mature Complications • • • • • • Miscarriage 1:300 – 1:500 (0.2 – 0.3%) Abdominal cramps Leakage of fluid Spotting Infection Mild abdominal cramps/slight abdominal site tenderness at needle puncture site normal Fetal Fibrinectin (FDA, 1995) • A glycoprotein & major component of the extracellular matrix of the membranes of the amniotic sac • Secreted from fetal membranes, found in the junction between the chorion & the decidua • Acts as a “glue”, binds placenta to the uterus • Normally absent (< 50 ng/ml) from vaginal secretions from 24-36 wks gestation. – Levels > 50 ng/ml between 24-34 wks is predictor of PTL Should Not Be Used for Symptomatic Women: • • • • • Advanced cervical dilation (>3 cm) Rupture of amniotic membranes Cervical cerclage Moderate or gross vaginal bleeding Sexual intercourse in past 24 hours Fetal Fibrinectin • Factors affecting accuracy – Sexual activity w/in 24 hrs of sampling – Cervical exam w/in 24 hrs of sampling – Vaginal bleeding – Intraamniotic & vaginal infections – Use of douches Sample Collection • Must be collected during speculum exam B/4 any other exam performed (lubricating gel interferes w/test results) • “Specimen Collection Kit” is the only acceptable specimen collection system Sample Collection • During spec exam, • Remove swab & lightly rotate swab immerse Dacron tip in across posterior fornix buffer. Break shaft (at of vagina (sympt. the score) even w/top of women) or external the top. cervical os (asympt. • Align shaft w/hole in women) for 10 sec. to cap and push tightly. absorb secretions • Send at room temp to lab Salivary Estriol (FDA, 1998) • Levels in maternal saliva just prior to PTL – Wait at least 1 hr after eating, smoking, chewing gum, or caring for teeth/gums – Rinse mouth with water, wait 10 min. – Places funnel to lower lip, catch saliva – Collect between 0900-2000 to avoid normal night-time surges of estriol – Level > 2.1 ng/mL is considered + – 5 samples recommended over 10 wks between 26 to 35 wks Test Interpretation • Negative predictive value high – fFN - up to 95% (1:125 chance of delivering in 2 wks) • Costs ~ $230 – Salivary estriol - up to 98% • Costs ~ $90 each (x5 = $450) • Positive predictive value low – fFN - 25 to 40% (1:6 chance of delivering in 2 wks) – Salivary estriol - 7 to 25% Assessment • Maternal – History – Vital Signs – Uterine Activity – Cervical Status Assessment • Fetal – EFM – Nonstress Test (NST) – Biophysical Profile (BPP) – Serial Ultrasound Assessment • Psychological – Anxiety – Stress Factors Nursing Considerations • Bed rest - lateral recumbent – Benefits: intravascular volume & uterine blood flow, pressure on cervix • Uterine Status – PALPATE!! – Q. shift, palpate to assess UCs • Preterm Labor S/S – interventions – Instruct what to report/what to do for ↑ UCs • Maternal/Fetal Vital Signs – Temp at least q. 4 hours if ROM Interventions • Intake/Output – Careful I&O if on tocolytic therapy – ↑ output may mean ↓ serum Mg levels and vice versa • Education – – – – How to palpate UCs, interventions Fetal movement counts Bedrest/activity restrictions When to call provider • Comfort Measures/Emotional Nursing Interventions B/4 Calling Doctor • • • • • Make sure patient side-lying Oral or IV hydration (unless contraindicated) Empty bladder Palpate UC’s SQ, oral, or demand dose of terbutaline if ordered Clarify What Bedrest Order Means... • Resting a few times a day at home • Bed with bathroom & meal privileges • Bed with bathroom privileges (meals in bed side lying) • Complete bedrest with no BRPs • Trendelenburg with foley • “Pelvic rest” • Etc. Bedrest Effects: Musculoskeletal System • Muscle atrophy starts to occurs within 6 hours of bed rest – Large, weight-bearing muscle groups affected more • Bone loss occurs – Calcium, phosphorus, magnesium, & zinc excreted in excessive amounts – Great bone loss occurs in the calcaneus (largest bone in foot), hip, and lumbar spine • Recovery prolonged and bone loss is not completely restored in hip & spine may induce early osteoporosis Bedrest Effects: Cardiopulmonary System • Lower extremity fluid redistributed headway (~ 600-700 ml) – ↑ in thoracic fluid volume, stimulates diuresis of fluid & electrolytes – State of hypovolemia produced • Pulmonary changes – Lung volume ↓, so airway resistance ↑ Cardiopulmonary Changes • Cardiovascular changes: – ↓ in plasma volume by 15-20% – ↓ total blood volume 5-10% – ↓ in CO by 25% – HR ↑ gradually, BP remains relatively stable – Trendelenberg bedrest ↑ the losses more rapidly Recovery Cardiopulmonary Changes • Prolonged and varies • Bouts of orthostatic intolerance, fainting, ↑ heart rate, syncope, fatigue • ↑ venous pooling in dependent body parts producing edema, redness, and discomfort Metabolic & Endocrine System • Basal metabolic rate ↓ 2-22%, depending on length of bedrest • Weight loss due to loss of fluid, bone, muscle, & appetite – Loss occurs primarily in lean rather than fatty tissue • Immune system – prolonged activity restriction reported to ↓ natural killer cells, phagocytic activity of neutrophils & T-lymphocytes Metabolic & Endocrine • Dirunal rhythms unstable – Sleep/wake cycles altered – Quantity & quality of sleep affected • Hormonal changes – Alterations in insulin secretion – insulin resistance develops hyperglycemia – Can happen as early as 2nd day of bedrest – The longer the bedrest, the ↑ the intolerance Physiologic Effects • Reduced sensory & social stimulation – Too little sensory stimulation can be as stressful as too much • Sense of physical restriction or confinement • Stress compounds the complex adverse effects of bedrest • Affect, cognition, perception, and motor coordination are adversely affected Family Effects & Finances • Fathers/partner stressed from “having to do everything”, constant state of worry • Mother stressed re: leaving all the work to family members • Child care concerns • Loss of maternity leave time • Loss of pay check Antepartum, Physiologic - Summary • Muscle weakness • Cardiovascular deconditioning • Fatigue • Orthostatic hypotension • Backache • Muscle ache • Joint pain • Difficulty concentrating • Dizziness • Shortness of breath • Difficulty sleeping • Weight loss AP, Physiologic/Psychosocial Summary • • • • • • • Maternal stress Paternal stress Family stress Child care problems Financial difficulties Depression Anxiety • • • • • • • Hostility Mood lability Loneliness/isolation Boredom Sense of confinement Guilt Loss of control/autonomy Post Partum • Muscle weakness • Cardiovascular deconditioning • Fatigue • Orthostatic hypotension • Backache • Muscle soreness • Difficulty walking • Difficulty concentrating • Dizziness • Shortness of breath • Prolonged recovery • Depression • Delay in performing ADLs Postpartum Symptoms After Antepartum Bedrest • Maternal symptoms during PP recovery under-recognized • In 1 study, most common symptoms 8 wks PP were extreme tiredness and backache (Thompson et al, 2002) Implications for Nursing • After bedrest, assessment of symptoms before hospital discharge is needed, and continued assessment may be needed beyond 6 weeks PP • Early DC may not be advisable – need to recover from childbirth & bed rest Nursing Implications • Early ambulation can help women begin to recover from musculoskeletal & cardiovascular deconditioning, but be careful! – Overuse of muscles can cause muscle tears & lead to injury & falls. • Instruct women of s/s after bed rest: limited strength, fatigue, muscle soreness, orthostatic hypotension Nursing Implications • Instruct woman that: – Ambulation will restore function – Extra help will be needed with household chores – Caution is needed to prevent injury & falls, especially when using stairs – Lingering symptoms should be reported to care provider – Referral to rehab program can help women safely rebuild atrophied muscles without injury and restore cardiovascular status. Tocolysis • Goals – Inhibit contractions – Prevent cervical change – Prolong pregnancy Medications - See Med Sheet • Betamimetics (Ritodrine, Terbutaline) • Magnesium Sulfate • Prostaglandin Inhibitors (Indomethacin) • Calcium Channel Blockers (Nifedipine) • Oxytocin Antagonists being studied Progesterone to Risk PTB • Several small studies suggested that 17alpha-hydroxyprogesterone caproate (17P) may reduce the risk of PTB – Must be initiated between 16-20 wks in order to decrease risk – Weekly injections of 250 mg 17P (suppositories also used in studies) – Significantly reduced risk of delivery at < 37, 35, and 32 wks gestation. – Fewer neonatal complications (IVH, NEC, O2) • Ideal formulation unknown (ACOG Committee Opinion) Antenatal Steriods • Benefits – incidence of RDS – incidence of IVH • Disadvantages of Multiple Courses – Fetal Effects (adrenal suppression, cerebral demyelinization, deleterious effect on lung growth) – Maternal effects (increased incidence of infection, adrenal suppression) – Occurred with 3 or more rounds of steroids; 2 rounds might be okay, ie, early & again at 32 wks if S/S PTL SQ Pump • Infrequent use – used for SQ infusion of terbutaline (also Zofran for hyperemesis) • Print policy & follow step-by-step • Notify Home Infusion – they must first check with insurance to see if it is covered! • Ruth P. coordinates program Quick-Set Infusion Set Needle Insertion Prep skin, then remove needle shield and paper backing Needle Insertion Insert with quick “jab”, depress opsite to seal, remove needle Activate needle cover to discard Remove tubing for showers Prevention Strategies • In 2003, AWHONN joined March of Dimes in a 5-year campaign to awareness of PTB and to the rate of PTB in the US – Will invest $75 million and raise new funds to support research – Advocate for an of $10 million annually in federal research into causes of prematurity Home Care/Education • • • • • • Risk Factors PTL Prevention/Treatment PTL Signs/Symptoms Uterine Contraction Assessment Fetal Movement Counts Followup Care If Home on Bed Rest • Develop “control center” – Room near bathroom, phone, TV, electrical outlets – Place bed near window if possible, eggcrate mattress may help – Cooler for snacks, ice, drinks – Water pitcher, large mug – Small shelf/table for books, magazines, etc. • Separate room for day vs. bedtime In-Hospital Bed Rest • Create “home-like” environment (pictures, favorite pillow, blanket, sweat suits to wear, etc.) • Place bed near window • Change patient rooms if extended stay • Enc. patient to develop routine (i.e., breakfast, Dr. rounds, EFM, shower, read, rest, lunch, movie/TV, nap, read, supper, EFM, etc.) • Get movies, hobbies for patient, etc. What Nurses Can Do • Educate on importance of prenatal care, risk reduction, and recognizing S/S of PTL • Screen women for urogenital infections • Assess women’s stress levels • Assess for domestic violence • Assess & help with smoking, alcohol, & drug use • Assess nutritional status References • Fortney, S. M., Schneider, V. S., & Greenleaf, J. E. (1996). The physiology of bed rest. In M. J. Fregley & C. M. Blatteis (Eds.), Handbook of physiology (Vol. 2, pp. 889-939). New York: Oxford University Press. • Maloni, J. A. & Park, S. (2005). Postpartum symptoms after antepartum bedrest. Journal of Obstetric, Gynecologic, & Neonatal Nursing (34):2, 163-171. • Thompson, J. F., Roberts, C. L., Currie, M., & Ellwood, D. A. (2002). Prevalence and persistence of health problems after childbirth: Associations with parity and method of birth. Birth, 29, 83-94. • Maloni, J. (1998). Antepartum Bed Rest: Case Studies, Research, & Nursing Care. AWHONN