MODULE VII
advertisement

MODULE 10
Pharmacology II
Lifespan Considerations
Pregnant Women
If possible, drug therapy should be delayed
until after the first trimester, especially when
there is danger of drug-induced developmental
defects.
Potential fetal risks must be compared to
maternal benefits when drug therapy is
required.
Minimum therapeutic dose should be used for
as short a time period as possible.
2
Lifespan Considerations (cont’d)
Pregnant Women
FDA Pregnancy Categories:
Drugs in categories A and B most likely
carry little or no risk to the fetus.
Drugs
in categories C and D most likely
carry some risk to the fetus.
Drugs
in category X are contraindicated
during pregnancy.
3
Lifespan Considerations (cont’d)
Pregnant Women
There are certain situations that require judicious
use of drugs during pregnancy:
Hypertension
Epilepsy
Diabetes
Infections that could seriously endanger the
mother and fetus
4
Lifespan Considerations (cont’d)
Breast-feeding Women
Many drugs cross from the mother’s circulation
into breast milk and subsequently to the infant,
although in small amounts because this is not
the primary excretion route.
Again, the risk to benefit ratio must be
evaluated.
5
Lifespan Considerations (cont’d)
Children
Parent is important source of:
Information about the child
Source of comfort for the child
Partner with the health care team during
drug therapy.
Should not be used to refer to a patient under 1
year of age.
6
Lifespan Considerations (cont’d)
Children
Differences in Physiology and
Pharmacokinetics
Immaturity of organs most responsible
Anatomic structures and physiologic systems
and functions are still in the process of
developing
7
Lifespan Considerations (cont’d)
Children
Pharmacodynamics (Drug Actions)
Some
drugs may be more toxic in children and
some less.
More toxic – Phenobarbital, morphine, ASA
Same – Atropine, codeine, digoxin
Contraindicated – tetracycline (discolor teeth),
corticosteroids (may suppress growth)
Fluoroquinolone antibiotics (may damage
cartilage leading to gait deformities)
Some tissues may be more sensitive – smaller doses
8
Lifespan Considerations (cont’d)
Children - Kid Facts
Safe, appropriate drug therapy must reflect
the differences between adults and children.
The child’s stage of growth and development
must be considered when assessing core
patient variables and the interaction of core
drug knowledge and core patient variables.
Pediatric drug dosages must be accurate to
reduce risk of adverse effects and prevent
over dosage.
9
Lifespan Considerations (cont’d)
Children - Drug Administration
Choice of appropriate route and/or site of drug
administration will vary by the child’s age and
size and the drug.
Special techniques may be needed to minimize
traumatic effects to the child:
EMLA cream can be used to numb an area
prior to an injection.
A popsicle or ice chips can be used to numb
taste buds before unpleasant-tasting oral drugs.
Do not mix drug therapy into infant formula.
10
Lifespan Considerations (cont’d)
Children – Nursing Responsiblities
Education about medications should be
provided for the patient, at an appropriate
developmental level, and to the family.
Implement the “6 Rights.”
It may often be necessary for 2 nurses to
check the medication(s). Check agency policy.
11
Lifespan Considerations (cont’d)
Older adults/Geriatric Considerations
Share common age-related changes and risk
factors that alter drug administration, dosage
and expected response to drug therapy.
All pharmacokinetic processes are altered,
placing older adults at higher risk for adverse
drug effects.
12
Lifespan Considerations (cont’d)
Geriatric Considerations Pharmacokinetics:
Alterations in absorption are more likely caused
by disease processes.
Distribution is altered because of:
Decreased
body mass
Reduced levels of plasma albumin
Less effective blood-brain barrier
Hepatic metabolism is slowed.
Renal efficiency is decreased:
Serum
creatinine levels will remain normal even
though kidney function is impaired.
13
Lifespan Considerations (cont’d)
Geriatric ConsiderationsPharmacodynamic Changes
Receptor site changes.
Blood-brain barrier allows more drug to enter
the brain.
Normal aging-related decline in organ or
system function occurs.
14
Lifespan Considerations (cont’d)
Geriatric Considerations
o Polypharmacy
May see multiple MDs for various illnesses and all
may prescribe meds.
Consume approx 32% of all Rx drugs and 40% over
the counter (OTC) drugs
Most common Prescriptions – antihypertensives,
insulin, beta blockers, digitalis, diuretics,
potassium (K) supplements
Most common OTC’s – analgesics, laxatives,
nonsteroidal anti-inflammatory drugs (NSAIDS)
15
Lifespan Considerations (cont’d)
Geriatric Considerations
Nonadherence – Lack of knowledge or incomplete
knowledge leads to misunderstanding about
medication regime.
Lifestyle – Choices may have to be made between
food, rent and purchase of medications.
16
Lifespan Considerations (cont’d)
Geriatric Considerations:
Simplify the therapeutic regimen.
Give memory aids (if necessary).
Give written instructions.
Determine financial access to drug therapies.
Assess cultural barriers.
Titrate the dose upward slowly to minimize
adverse effects.
17
Cultural Considerations in
Drug Therapy
The Law of Cultural Diversity
Each patient needs to be considered an
individual, regardless of cultural, ethnic or
religious beliefs.
Although members of a culture share certain
beliefs and practices, individual variation will
still occur. Many cultural groups in the U. S.
have beliefs that reflect both their original
ethnic culture and the dominant culture of
the United States.
18
Ethnic Considerations in
Drug Therapy
Drug polymorphism
Critical in understanding a patient’s response to drug
therapy
May explain many adverse and idiosyncratic reactions
Refers to how individuals metabolize differently
Looks at genetics that often have a common basis in
ethnic background
Opens up a new field of study in pharmacology that has
been lacking for years due to societal factors
Examples: Why does the African-American respond
differently to antihypertensives, the Chinese patient
require lower doses of benzodiazepines, the Caucasian
respond differently to some pain medications?
19
Ethics and
Drug Therapy
Nurse’s responsibility is to always be a patient
advocate and remain nonjudgmental.
ANA Code of Ethics
Canadian Nurses Association Code of Ethics
Various Nurse Practice Acts
All share the framework for the professional practice of nursing.
All believe that, professionally, the nurse provides safe nursing
care to patients regardless of the group, community, ethnicity or
culture.
Nursing does not impose values or standards on the patient.
Nurses assist the patient and family in facing decisions regarding
health care.
20
Botanical Dietary Supplements
For a complete list of botanical
dietary supplements fact sheets,
(National Institutes of Health), see :
http://www.ods.od.nih.gov/Health_I
nformation/Botanical_Supplements.
aspx
21
The
th
5
Vital Sign
Pain
Opioid & Non-Opioid Analgesics
Aspirin
NSAIDs
COX-2 inhibitor
Acetaminophen
Narcotics
Analgesics
Definition of an analgesic:
“Medications that relieve pain
without causing loss of
consciousness”
Pain is a subjective experience. The nurse must
believe the patient. PET scans now can
visualize brain’s responses to many kinds of
pain.
23
Proposed Pain Pathway
Nociceptors (free nerve endings)
Afferent stimulation of sensory “A” or “C”fibers
Release of peptide substance P from unmylinated
“C” fibers in dorsal horn
Dorsal horn spinal cord – the location of the “gate”
3 major brain pathways:
Spinothalamic, spinoreticular, spinomesencephalic
(Multiple neurotransmitters released)
24
Pathophysiological
Many theories of pain transmission
are not completely understood.
Nociceptive
pain
Neuropathic pain
Psychogenic pain
The type of pain determines the analgesic.
Neuropathic pain is often treated with anticonvulsants,
tricyclic antidepressants added onto narcotics
25
Pain Transmission
These techniques also allow some nonpharmacological relief from pain:
Massage
Deep pressure
Distraction
Relaxation
Vibration
Can be used as independent nursing intervention after
assessment
The above activate the large “A” fibers.
26
Factors Influencing Pain
Perception
Type of pain
Acute vs. chronic
Visceral vs. cutaneous
Nociceptive, neuropathic, psychogenic
Intensity of pain & type of injury
Inflammatory process
Degree of Anxiety
27
Factors Influencing Pain
Perception
Sensory input
Social support
Fatigue
Age, sex & culture
Memory & information processing
Level of consciousness
Type, amount, route of analgesic
28
Drugs Influencing Pain Perception
Narcotics (opioids) modify pain perception
via Central Nervous System (CNS) & dorsal
horn via binding to Mu, kappa & delta opioid
receptors & inhibiting substance “P” and
glutamate (an excitorary neurotransmitter).
Alter perception of pain via opiate receptors,
and alter psychological responses via brain.
Other mechanisms to alter pain involve effects
on the Autonomic Nervous System (ANS),
skeletal muscle response & diagnosis.
29
Drugs Influencing Pain Perception
Nonopiate analgesics (salicylates,
NSAIDS, etc.)
Control pain impulses in the periphery
Often involving the Arachidonic acid
pathway responsible for inflammation and
an immune response
30
Some Pain Mysteries
Phantom
pain
Referred
pain
Pain
experienced after cordectomy
Placebo
response
31
Prostaglandins
Associated with inflammation
Involved in the temperature set point
of the hypothalamus
Sensitize pain receptors to mechanical
and chemical stimulation
Found in many cells and body
processes
32
Leukotrines
Arachidonic acid metabolites
Mediators in inflammation
Synthesized when tissue injury occurs
May be involved in rheumatoid arthritis,
asthma and system wide anaphylaxis
Bronchoconstrictor and vasodilator
33
Synthesis of Prostaglandins
Arachidonic acid
Lipoxygenase
Leukotrines
enzymes
Cyclooxygenase
Prostaglandins
34
TWO Enzyme FORMS
CYCLOOXYGENASE-1 & CYLOOXYGENASE- 2
COX-1
COX-2
Prostaglandins
Protects stomach lining
Inflammation
Pain
35
Peripheral control of pain
Release of prostaglandin
inflammation & pain
Prostaglandins mediate pain and swelling by
triggering vasodilatation. Prostaglandins are
synthesized by the enzyme cyclooxygenase which
breaks down arachidonic acid to synthesize
prostaglandin. This is the basic method of action
of aspirin and NSAIDs.
36
Inhibition of Cox-1 & Cox-2
Inhibition of both Cox-1 & Cox-2 will be
effective as an:
ANALGESIC
ANTIPYRETIC
ANTI-INFLAMMATORY AGENT
AGENT TO DECREASE PLATLET AGGREGATION
Also associated with stomach damage due
to COX-1 inhibition
37
Aspirin
Inhibits both Cox-1 and Cox-2
Is used as a analgesic
Is used as a anti-inflammatory agent
Is used as a antipyretic
But can cause stomach damage
Is used to prevent coronary heart disease
(CHD) via platelet aggregation
In what other cases should aspirin NOT be
used?
38
Aspirin adverse effects &
interactions
Tinnitus – sign of toxicity
Dyspepsia
Highly protein bound so it displaces other
medications: oral anticoagulants, oral hypoglycemics,
some anticonvulsives.
G.I. Bleeding increased with glucocorticoids, alcohol
High doses may cause excessive bruising
Highly lethal if taken in overdose - No known
antidote
Caution with asthmatic patients (may have aspirin
allergy also)
39
Hold giving Aspirin
40
Children under 15 with
viral infection
Reye’s syndrome is associated with aspirin use.
41
NSAIDS
Non-Steroidal Anti-Inflammatory Drug
First line treatment for inflammation
Both COX-1 & COX-2 inhibitors
Mild to moderate pain of various types
Good for dysmenorrhea
Antipyretic
Reversibly inhibit platelet aggregation (less than
aspirin because aspirin has irreversible
inhibition)
INHIBIT THE PRODUCTION OF PROSTAGLANDINS
THAT MEDIATE PAIN AND INFLAMMATION
42
Side effects & Interactions of
NSAIDs
G.I. Bleeding, dyspepsia
Liver toxicity or renal damage with large
doses, prolonged use
Highly bound to plasma protein so
displace other medications, leading to
exacerbation of their side effects
These adverse effects can occur with oral or
parenteral routes and even if enteric coated.
43
Don’t give aspirin or NSAIDs
Patients with ulcers
Patients going to surgery
Patients with an allergy to aspirin
Alcoholic patients
When patient is nauseated or vomiting
Patients on glucocorticoids (without M.D. order)
Patients taking ACEIs (Angiotensin Converting
Enzyme Inhibitors)
Caution with NSAIDs in patients with CHF
44
COX-2 INHIBITOR
Celecoxib (Celebrex) Approved for
osteoarthritis and rheumatoid arthritis
Acute pain & dysmenorrhea
Do not give if sulfa allergy
Only COX-2 inhibitor currently available
Has anti-inflammatory properties
45
Acetaminophen (Tylenol)
Is a very weak inhibitor of both Cox-1 and
Cox-2
Is used as an antipyretic
Is used as an analgesic
Can not be used as an anti-inflammatory
agent
Does not stop platelet aggregation
May work by inhibiting prostaglandin
synthesis in the CNS
46
Acetaminophen
Is the drug of choice for mild to moderate pain
Is often combined with opioids to treat moderate
to severe pain
Will cause liver failure in LARGE doses or
prolonged use (2.4 to 4 grams/day)
Liver failure with alcohol due to metabolic
pathways
Ceiling effect
Overdose is difficult to treat - use acetylcysteine
47
Acetaminophen
Young children, older adults, daily drinkers of
3 or more alcoholic beverages and those with
kidney or liver disease are at risk for
accidental acetaminophen poisoning
Acetaminophen found in many
pharmaceuticals
Vicodin ES (5 tabs Q. D. = 4 gm)
Tylenol extra-strength (8 tabs = 4 gm)
What other OTC medications might contain
acetaminophen?
48
Neuropathic Pain
Difficult to treat
Use of opioids does not completely control pain
Usually add on another medication from a different class
(co-analgesic agents)
immipramine (Tofranil) Tricyclic antidepressant -TCA
gabapentin (Neurontin) Anticonvulsant
Duloxetine (Cymbalta) newest SNRI (serotonin
norephinephrine reuptake inhibitor) - also used for
depression
Effexor is another medication in this class
New pregabalin (Lyrica) anticonvulsant - alpha2 - delta
ligand
+ other medication classes
49
Natural, synthetic and semisynthetic
ALL COMPARED TO MORPHINE
50
Opiates
Narcotics: Very strong pain relievers
Opiates:
Pain relievers that contain opium, derived
from opium, or are chemically related to
opium
51
Pain Transmission
o
Body has endogenous neurotransmitters
o
Endogenous neurotransmitters are:
enkephalins & endorphins (morphine-like
peptides) produced by body to fight pain
o
Opiates bind to these natural endogenous
opioid receptors
o
Inhibit substance P in dorsal horn of spinal
cord
52
Chemical Classification of Opioids
CHEMICAL CATEGORY & examples
Natural:
codeine, morphine
Semi-synthetic:
hydrocodone (Vicodin)
oxycodone + salicylate
Synthetic:
meperdine (Demerol) can be
neurotoxic and cause
confusion/seizure - NEVER
give to patients with
Parkinson’s Disease
butalbital (Fiorinal)
(Percodan)
53
Opiates
Three
classifications based on their
actions:
agonist
agonist-antagonist
partial agonist
54
CNS Opiate effects/uses
Analgesia
Cough suppression
Euphoria
Reduces fear/anxiety
Raises pain threshold (decreased awareness)
Sleep induction
Respiratory depression
Pupil constriction (miosis)
Nausea and vomiting
55
Peripheral Nervous System
OPIATE Effects
Constipation
Urinary
retention
Diaphoresis & flushing
Hypotension due to vasodilatation
56
Narcotic analgesic routes
PCA example Morphine (acute pain)
Transdermal example Duragesic patch (fentanyl)
(chronic pain)
Epidural example fentanyl or morphine
Oral example MS Contin (morphine)(chronic
pain)
I.M injections example meperidine (acute pain)
(Demerol). Do not give for more than a day –
neurotoxic, lowers seizure threshold, not first line
agent. Metabolite normeperidine neurotoxic and
may cause psychosis in the elderly patient.
57
Gold Standard is Morphine
No ceiling effect
ADVANTAGES
Decreased awareness
Decreased anxiety
Increased sleep
Decreased pain
perception
DISADVANTAGES
Hypotension
Constipation
Nausea
Respiratory depression
Itching
Secondary effects of cough suppression and
constipation are used therapeutically
58
Oral Morphine examples
Oxycontin (oxycodone)
MS Contin (morphine)
Kadian (morphine)
Oramorph SR (morphine)
Avinza (morphine)
New Q day dosing (Do not crush, chew or
dissolve the caps or could deliver fatal dose)
If can not swallow, O.K. to open & sprinkle the
beads on applesauce
59
Mixed agonist-antagonists
Pentazocine
(Talwin)
Buprenorphine (Bupreneax)
Butorphanol (Stadol)
Ultram (Tramadol) - mechanism of action not
clearly understood, weak bond to opioid receptors
& inhibits reuptake of norepinephrine (NE) &
serotonin (5-HT) may cause chemical dependency
These medications are rarely used
DO NOT GIVE THESE MEDICATIONS TO PATIENTS
WHO ARE DEPENDENT ON NARCOTICS.
60
Opiate Antagonists/blockers
Naloxone (narcan) opiate antagonist
[competitive]
Naltrexone (ReVia) now used to help
alcoholics stay abstinent
61
Opiates
Opioid Tolerance:
a common physiologic result of chronic
opioid treatment
means larger doses of opioids are required
to maintain the same level of analgesia
62
Opiates
Physical Dependence
The physiologic adaptation of the body
to the presence of an opioid
Opioid tolerance and physical dependence
are expected with long-term opioid
treatment and should not be confused with
psychological dependence [addiction].
63
Opiates
Psychological Dependence
[addiction]
A pattern of compulsive drug use characterized
by a continued craving for an opioid and the need
to use the opioid for effects other than pain relief
64
Opiates
Misunderstanding these terms
leads to ineffective pain
management and contributes to
the problem of under treatment.
65
Opiates
Physical dependence on opioids is
known when the opioid is abruptly
discontinued or when a opioid
antagonist is administered.
narcotic withdrawal
opioid abstinence syndrome
66
Opiates
Narcotic withdrawal
Opioid abstinence syndrome
Manifested as: (flu-like symptoms)
Anxiety, irritability, chills and hot flashes,
joint pain, lacrimation, rhinorrhea,
diaphoresis, nausea, vomiting, abdominal
cramps and diarrhea
67
Drugs Affecting the Autonomic
Nervous System
68
Photo Source: National Institutes of
Health, Public Domain,
http://catalog.niddk.nih.gov/ImageL
ibrary/searchresults.cfm
69
Sympathetic NS
FIGHT
&
FLIGHT
70
Parasympathetic N.S.
BREED
&
FEED
71
Adrenergic Drugs
Mechanism of action
Mimic Sympathetic Nervous System (N.S.)
Have sympathomimetic properties
Have sympatholytic action also since they oppose
the parasympathic N.S.
Catecholimines are neurotransmitters involved in
adrenergic system
DA (dopamine) NE (norepinephrine) E (epinephrine)
Energizing neurotransmitters
Direct-acting, indirect acting and mixed
adrenergics
72
Adrenergic Drugs (cont’d)
Indications
Bronchodilation (albuterol)
Cardiac stimulation, alpha1, beta 1, beta 2,
increase blood pressure (dopamine, isoproterenol)
Mental alertness & wakefulness (monafnil)
Appetite suppression (adipex)
Decongestion (pseudoephedrine)
Open angle glaucoma (dipivefrin) produces
mydriasis = pupil dilation
ADHD (methylphenidate)
Adverse effects
Tachycardia, hypertension, anxiety, insomnia,
psychological dependency
73
Alpha -Adrenergic Blocking
Drugs
Drug examples: ergotamine tartrate (Egostat),
Phenoxybenzamine, phentolamine (Regitine)
Indications: Raynaud’s disase, hypertension
secondary to pheochromocytoma, extravasation
of vasopressors, vascular headaches
Adverse effects: nasal congestion, orthostatic
hypotension, tachycardia, dizziness,
(Gastrointestinal) GI irritation, and miosis.
Ergotamine may cause chronic poisoning.
74
Beta-Adrenergic Blocking
Drugs
Drug examples: selective for beta 1 receptors - atenolol,
metoprolol
Non-selective for beta 1 & 2 receptors - propranolol
(contraindicated in pt. with COPD, asthma, depression)
Indications: treat hypertension, angina,
tachyarrhythmias, CHF, Post MI because they are cardiocardio-protective
Contraindications: bradyarrhythmias, bronchospasm,
heart blocks
Adverse effects: arrhythmias, bradycardia,
bronchospasm, nausea, vomiting, diarrhea, increased
sensitivity to cold, rebound HTN if stopped abruptly
75
Cholinergic Drugs
cholinergics
cholinergic agonists
parasympathomimetics
Sympatholytics
All are terms that refer to drugs that stimulate the
Parasympathic Nervous System
MIMIC ACETYLCHOLINE
Cholinergic drugs
76
Cholinergic Drugs
Cholinergic
receptors [two types]
Based on location & their action
Nicotinic {N}
&
Muscarinic {M}
77
Drug & Side Effects of
Cholinergics
Salivation
Lacrimation
Urinary incontinence
Diarrhea
Gastrointestinal cramps
Emesis
(Also bronchospasm, decreased intra ocular
pressure (IOP), decreased heart rate, increased
bronchial secretions, miotic, sweating)
78
Cholinergic Drugs
Indications
Direct- acting
Indirect-acting
Cholinesterase inhibitors (reversible) – for Alzheimer’s & to treat
myasthenia gravis (MG) and open angle glaucoma not responsive
to other agents – prevents postoperative paralytic ileus
Drug examples – bethanechol, pilocarpine
Cholinergic agonists – used to treat open angle glaucoma and dry
eyes and to stimulate bladder
Bethanechol – treat nonobstructive urine retention, neurogenic
bladder, adynamic ileus
Pilocarpine – treat glaucoma
Contraindications
Possible urinary or GI obstruction and pregnancy
79
Cholinergic-blocking drugs
Class of drugs that block or inhibit the
actions of Acetylcholine in the
Parasympathetic Nervous System
anticholinergics
parasympatholytics
antimuscarinic agents
80
Cholinergic-blocking drugs
(also called anti-cholinergic drugs)
Inhibit nicotinic {N} or muscarinic {M} receptors
Anticholinergic effects are the result of
muscarinic blockage, primarily on the post
synaptic receptor of the Parasympathetic Nervous
System.
There are medications that are designed for their
anticholinergic effect.
Many medications have anticholinergic side
effects that are NOT wanted.
81
Cholinergic-blocking drugs
Atropine
Dicyclomine (Bentyl)
Preop for secretion control, therapeutic
anticholinergic effect, Bradycardia, anticholinesterase
effect for insecticide poisioning CNS excitation
Irritable bowel syndrome (IBS)
Propantheline bromide (Pro-Banthine)
Adjunct in Treatment of peptic ulcer, IBS,
pancreatitis
82
Cholinergic-blocking drugs
Glycopyrrolate (Robinul)
Scopolamine (Transderm-Scop)
Control of secretions intraoperative, preop control
of secretions, preop for electro convulsive therapy
(ECT)
Prevents motion sickness
Orphendrine (Norflex)
A central acting anticholinergic muscle relaxant
83
Therapeutic effects of
Anticholinergics
Tolterodine (Detrol) & Trospium
Chloride (Sanctura) new
Benztropine (Cogentin)
Overactive bladder
Parkinson’s DZ and EPS (neurological side
effects) from antipsychotics
Ipratropium Bromide (Atrovent)
Inhaled drug used to treat COPD, asthma,
little systemic effect because inhaled
84
Drug Interactions
ADDITIVE EFFECTS WITH: antihistamines,
anticholinergics, phenothiazines,tricyclic
antidepressants, MAOI’s (monoamine oxidase
inhibitor)
Antihistamines have anticholinergic effects
This could cause confusion & or psychosis in the
ELDERLY PATIENT.
Contraindicated in: glaucoma, benign
prostatic hypertrophy (BPH), Cardiac disease and
obstructive bowl & asthma unless inhaled
85
Secondary effects/Side
effects
(anticholinergic)
Xerotomia (dry mouth)
Blurred vision
Urinary retention
Decreased perspiration
Constipation
Tachycardia
These are common in many of the
psychoactive drugs
86
Neuromuscular Blocking
Agents
Prevent nerve transmission in certain muscles,
leading to paralysis of the muscle at neuromuscular
junction by binding to Ach receptor
Indications – Maintains controlled ventilation
during mechanical ventilation or during
endotracheal intubation
Contraindications – Drug allergy, previous
history of malignant hypertension, penetrating
eye injuries and narrow-angle glaucoma
Side/Adverse Effects – Hypokalemia,
dysrhythmias, fasciculations, muscle pain,
increased intraocular and intracranial pressure
and apnea
87
CNS Depressants
Hypnotics and Sedatives
Classified into barbiturates,
benzodiazepines and miscellaneous agents
Act primarily on the brainstem; sedative
and hypnotic effects are dose related.
88
Barbiturates
Habit forming and have narrow therapeutic index
Contraindications –pregnancy, significant respiratory
difficulties and severe liver disease
Side Effects – Drowsiness, lethargy, dizziness,
hangover, and paradoxical restlessness or excitement
Adverse Effects – Vasodilatation, hypotension blood
dyscrasias, hypersensitivity reactions
Interactions – synergistic with other Central Nervous
System (CNS) depressants
Can be lethal in overdose
Can have lethal consequences of uncontrolled
withdrawal
89
Barbiturates Uses
Short-term treatment of insomnia (rare)
Sedation in lower doses
Ultra-short acting for anesthesia induction
Pre-op medication
Epilepsy, mainly status, but the long-acting
Phenobarbital can be used as anticonvulsant at small doses does not produce sedation, but
seizure activity
Not used as often today because of newer
agents for sleep, seizure and anxiety
90
Action and General Characteristics
of Benzodiazepines
Specific for cerebral cortex and limbic system
Also called anxiolytics
Increase action of GABA + other inhibitory
neurotransmitters
Highly lipid soluble to facilitate crossing into
CNS
Highly bound to plasma protein
Metabolized by the liver, some with long
duration of action due to active metabolites
91
Benzodiazepine Uses
Anxiolytics – examples: alprazolam (Xanax)
Anticonvulsants – examples: clonazepam
(Klonopin) and diazepam (Valium)
Anesthesia induction – examples: midazolam
(Versed), diazepam (Valium)
Muscle Relaxant – example: diazepam (Valium)
Withdrawal from alcohol – example:
chlordiazepoxide (Librium), diazepam (Valium)
Hypnotics – examples: flurazepam (Dalmane), and
temazepam (Restoril) do not depress REM sleep;
but prevent deep sleep (not natural)
92
Secondary/side effects of
Benzodiazipines
Daytime sedation
Ataxia
Dizziness
Anterograde amnesia
Idiosyncratic paradoxical excitement
SELDOM FATAL IF TAKEN ALONE
Can be dangerous for the elderly because of
fall potential
93
Centrally Acting Muscle
Relaxants
Primarily used for the relief of painful
musculoskeletal conditions–muscle spasms
and spasticity.
Side Effects – Euphoria, lightheadedness,
dizziness, drowsiness, fatigue and muscle
weakness - usually short-lived
Adverse Effects – GI upset, headache, slurred
speech, constipation, sexual difficulties in
men, hypotension, tachycardia and weight
gain
94
Anticonvulsant Medication
Causes of Seizure
Congenital abnormalities
Metabolic disorders – hypocalcemia
Trauma – accidents
Tumors – brain plus status post craniotomy
Vascular diseases – stroke
Degenerative disorders- Alzheimer’s
Infectious diseases – meningitis, AIDS
Fever & toxins
Medications – example = antipsychotics
Alcohol withdrawal + hypomagnesemia
95
Types of Seizure
according to International League Against Epilepsy
Partial Seizures:
focal area of brain initiates seizure
Simple partial:
focal symptoms, aura, conscious
Complex partial:
simple then impairment in consciousness
Generalized partial:
spread to both hemispheres
96
Types of Seizure
Generalized Seizures: both hemispheres
usually effected, unconscious
Absence seizures: impairment of
consciousness, autonomic components,
usually in children/adolescence
Tonic-clonic: (grand mal) tonic is muscle
stiffing, clonic is jerking
Monoclonic: single or multiple jerks
97
Status Epilepticus
Single seizure lasting for 20 minutes or
longer
Or recurrent generalized seizures without
regaining of consciousness in between
each seizure episode
Considered a medical emergency
98
Possible Action of
Anticonvulsants
Pharmacologically distinct action for
each group of anticonvulsants is
PROPOSED
Many mediate actions by limiting discharge
from a focal point – surrounding it
Others elevate seizure threshold through
neurotransmitters or ions
99
Possible General Mode of Action
Increase concentration
of GABA by
Blocking reuptake into glia & nerve endings
Inhibiting enzymes that catabolize GABA
Facilitating GABA & other inhibitory receptors
100
Mode of Action other than
potentiation of GABA
Suppression of calcium influx
Inhibition of voltage-sensitive sodium channels
Binding to the amino acid glycine
(neurotransmitter & inhibitory A.A.) at receptor site
Decreasing metabolism of glutamate
EXACT MODE OF ACTION NOT KNOWN
Agent chosen depends on type of seizure, age, sex,
pharmacologic properties, side effects and cost
101
Anticonvulsants
FIRST LINE AGENTS - USED AS
MONOTHERAPY for Tonic Clonic
Seizures
Phenytoin ( Dilantin)
Carbamazepine (Tegretol)
Valproic acid (Depakene or Depakote)
Primidone (Mysoline)
Phenobarbital
102
Anticonvulsants
FIRST LINE AGENTS USED AS
MONOTHERAPY for Partial Seizure
Carbamazepine (Tegretol)
Valproic Acid (Depakene or Depakote)
Lamotrigine (Lamictal)
Topiramate (Topamax)*
Gabapentin (Neurontin)*
* Not FDA approved for monotherapy, but studies support
103
Anti-convulsant
Drugs(Antiepilieptics)
Indications: Prevention and control of seizures
Main adverse effects of most anticonvulsants are mental
confusion and drowsiness
Interactions of many older meds:
Potentiate CNS depressants and alcohol
Concurrent use with tricyclic antidepressants or phenothaizines
lowers the seizure threshold and decreases the effectiveness of
anticonvulsants
Many drugs alter hepatic metabolism of anticonvulsants leading
to decreased serum levels and loss of seizure control and
toxicity
Phenytoin’s cytochrome P-450 enymatic reaction inhibits
atazanavir’s action (depakote becomes the drug of choice in this
104
example).
Anti-convulsant Drugs
Hydantoins
Drug examples: Mephenytoin, phenytoin
(Dilantin)
Indications: treat tonic-clonic (grand mal) seizures
and complex partial seizures, arrhythmias, and
painful condition such as trigeminal neuralgia
Adverse effects: (long term) gingival hyperplasia,
liver function abnormalities, blood dyscrasias,
(toxicity) as evidenced by diplopia, nystagmus,
ataxia, and drowsiness
Caution driving or operating equipment because of
mental confusion
105
Anti-convulsant Drugs
Tell patient to use alternate birth control
if on the pill
Supplement with Vitamin D, Calcium and
folic acid
Interactions with Calcium Channel
Blockers, Antipsychotics and steroids
P-450 = many interactions
106
Anti-convulsant Drugs
Interactions…
Oral tube feedings with osmolite or isocal may
interfere with absorption of oral dilantin
diminishing drug’s effectiveness
IV dilantin precipitates with D5W.
Characteristics of fosphenytoin (Cerebyx) –
preferred over IV Dilantin
Prodrug of phenytoin
Rapidly converted by blood and liver
enzymes to phenytoin (Dilantin)
Given I.V. only
107
Anti-convulsant Drugs
Barbiturates and deoxybarbiturates
Examples: Mephobarbital, phenobarbital, primidone
Indications:
Treat tonic-clonic seizures, partial seizures and
insomnia
Used as adjuncts to anesthesia
Adverse effects: Dizziness, drowsiness, hypotension,
respiratory depression with high doses
Interactions: Drugs decreases serum dilantin level
when used concurrently
Primidone plus phenobarbital may cause
phenobarbital toxicity
108
Anti-convulsant Drugs
Benzodiazepines
Examples: clonazepam (Klonopin) Diazepam
(Valium)
Indications: treat absence seizures, status
epilepticus, anxiety and skeletal muscle
spasms.
Adverse effects: ataxia, drug dependence,
respiratory and cardiovascular depression
109
Valproic acid (Depakene)
Divalproex (Depakote)
Low side effect profile, well tolerated
May cause liver failure (rare) in first 6 months
of therapy
Lethargy, muscle weakness, sedation
Leukopenia
Ataxia
Depakene causes nausea/vomiting
Interacts with many other anticonvulsants
110
Nursing Considerations
Good for generalized and partial seizure
Monitor blood levels
Monitor CBC and liver function tests
Highly protein bound, do not take with
NSAIDs, aspirin & other drugs that alter
coagulation
Potentiates CNS depressants
Reassure patient of alopecia, hair will regrow
Used as mood stabilizer for bipolar disorder
and has FDA approval for this
111
Carbamazepine (Tegretol)
Blood dyscrasias
* Notify health care provider
Liver toxicity
Rash
Drowsiness
Low side effect profile – well tolerated
* Immediately discontinue & switch to another
agent
112
Nursing Considerations
Low behavioral and toxicologic profile
Good for both generalized and partial
seizures
Autoinduction – dosage needs monitoring
via blood levels, decreases after initial doses
Advise alternate birth control if on pill
Monitor CBC for bone marrow depression
Used “off label” as mood stabilizer for
bipolar disorder
113
Lamotrigine (Lamictal)
Monotherapy in partial seizures
Well tolerated
No weight gain, no sedation
Rare, but can be associated with life
threatening rash (Stevens-Johnson
syndrome)
Nausea, vomiting, weight loss (rare)
Dizziness, ataxia
114
Nursing Considerations
Discontinue at once if rash/inform health care
provider
Nurse asks patient every visit
Taper on very slowly to avoid rash – 25 mg Q 2 weeks
until 200 mg
No blood levels required
Note many anticonvulsants raise or lower plasma
levels
Monitor for adverse reactions if not monotherapy
May reduce effectiveness of estrogen
Used for mood disorder in bipolar, good for
depressive side, and has FDA approval for this
115
Topiramate (Topamax)
Adjunctive therapy in partial and generalized
seizures (studies support monotherapy)
Well tolerated
Fatigue
Confusion
Difficulty concentrating, speech problems
(unable to recall words)
Nausea
Weight loss
No blood levels required
116
Gabapentin (Neurontin)
Adjunct therapy for partial seizures (studies
demonstrate monotherapy)
Excellent side effect profile
Main problem is initial sedation, ataxia
Not metabolized by liver so no interactions with
other anticonvulsants
Used extensively for neurogenic pain
Excellent for elderly and those on poly drugs
No blood levels required
Used “off label” as mood stabilizer for bipolar
disorder but no FDA approval for this
117
Other uses for
Anticonvulsants
Mood stabilizers
Migraine headache
Neurological pain
Chronic pain syndrome
Anxiolytics
118
Anti-Parkinsonian Drugs
Groups of Drugs Used
Antidyskinetic Drugs or anticholinergics
Antihistamines (have anticholinergic effects)
Dopaminergics
Dopaminergic
agonists
MAOI-B
(monoamine oxidase inhibitor)
COMT Inhibitors (catechol-0-methyl-transferase)
119
Anti-Parkinsonian Drugs
Dopaminergic agonists are mainstay
Contraindications and precautions:
Used
with caution in patients with residual
arrhythmias after MI, history of peptic ulcer,
psychosis or seizure disorders
Contraindicated with narrow angle glaucoma
Used with caution for patients with bronchial
asthma, emphysema, or severe cardiovascular,
pulmonary, renal, hepatic or endocrine disease
Adverse Effects:
Dizziness,
confusion, mood changes, orthostatic
hypotension, nausea, vomiting, hallucinations
120
Anti-Parkinsonian Drugs
General Information
Mechanism of of action: Restore the natural balance of the
neurotransmitters in CNS to decrease S/S of Parkinson’s
Disease. Imbalance between Achetylcholine (ACH) and
Dopamine. Too much ACH and too little dopamine. Meds
correct this.
Dopaminergic agonists
Mechanism of Action is to increase the amount of DA
available in the CNS or enhance the neurotransmission of
Dopamine
Medication examples:
Levodopa restores dopamine levels
Amantadine increases the amount of dopamine in the brain
Pramipexole (Mirapex) – newer DA receptor agonist
Ropinirole (Requip) – newer DA receptor agonist
121
Anti-Parkinsonian Drugs
anticholinergics
Drug examples: Benztropine (Cogentin)
Indications:
Bradyarrhythmias, dyskinesia, parkinsonism, peptic ulcer and bowel
spasms
Nausea, vomiting, induce mydriasis, decrease salivation and bronchial
secretions before surgery
Contraindications:
Trihexyphenidyl (Artane)
Procyclidine (Kemadrin)
Narrow-angle glaucoma, severe hemorrhage, uncontrolled tachycardia,
urinary tract/GI obstruction, BPH
Adverse effects:
Blurred vision, conjunctivitis, and photophobia, tachycardia,
constipation, dry mouth and urinary hesitancy
CAN CAUSE PSYCHOTIC CONFUSION IN THE ELDERLY
when drugs with anticholinergic effects are combined.
122
Two Newer class to treat
Parkinsons
Selegiline (Eldepryl)
MAOIB (monoamine oxidase inhibitor – B)
May have neuroprotective effects slowing the
progression of the Disease
Tolcapone (Tasmar) & entacapone (Comtan)
Catechol O-methyltransferase (COMT) inhibitors = newest class
Not used as monotherapy, but as add on to levadopa
to increase its efficacy.
Tasmar has been associated with liver dysfunction.
123
Two classes that reduce
dosage of Levadopa
MAOI-B DA in brain by inhibiting its
metabolism by MAO. Form “B” metabolizes
DA. At oral doses < 10mg Q.D. like MAOI- A
so acts more on tyramine NE, E, DA & 5H-T.
No food restrictions with low doses.
COMT inhibitors work by inhibiting the enzyme catecholO-methyltransferase the 2nd enzyme involved in the
metabolism of levodopa - so increased amount of
levodopa available.
124
Wearing off syndrome
Doses need to be adjusted upward and
downward as adverse mental changes occur
or Parkinson’s symptoms worsen.
Changing doses is done slowly.
125
Advanced Parkinson’s
A new DA agonist Apomorphine (Apokyn) given
S.Q. is available for advanced Parkinson’s as a
rescue drug for acute rigidity.
This is temporary add on, not replacement. N/V.
Rx for antiemetic.
Not 5-HT3 antagonists like ondansetron (Zofran)
because of hypotension.
Use trimethobenzamide (Tigan). Why do you
NOT want to use prochlorperazine (Compazine)??
126
Drugs used to Treat
Alzheimer’s
Cholinesterase inhibitors
Increase Acetylcholine (Ach) in key areas of brain
(cerebral cortex)
Reversible cholinesterase inhibitors
Used to Treat mild to moderate disease
Do not reverse symptoms; slow progression
Check P450 for drug interactions
Examples
Donepezil (Aricept)
Tacrine (Cognex) (1st, most adverse effects, not used
today)
Rivastigmine (Exelon) – newer {may have greater
efficiacy}
127
New class to Treat Alzheimer’s
Memantine (Nameda)
Released Jan. 2004 for Treatment of
moderate to severe Alzheimer’s Disease
May have more favorable side effect profile
than Ach inhibitors
May be possible to combine with ACh
inhibitors for better result
128
Drugs Affecting the
Cardiovascular and Renal
Systems
Drugs to Treat:
Congestive heart failure
Hypertension
Angina
129
Inotropic (increase force of contraction)
Drugs and Cardiac Glycosides
Indications
Used to treat CHF in combination with other medications.
Control ventricular rate in atrial fibrillation, atrial flutter,
paroxysmal atrial tachycardia
Contraindications and precautions
Uncontrolled ventricular arrhythmias, constrictive pericarditis,
complete heart block
Increased risk of toxicity with hypercalcemia, hypokalemia,
hypomagnesemia, hypothyroidism, or renal failure
Very narrow therapeutic index
Elderly patients more sensitive to toxic drug effects
Adverse effects – bradycardia, fatigue, weakness, nausea,
vomiting, diarrhea, visual disturbances
Monitor pulse – hold if less than 60/min. apical
Do not increase longevity in CHF
130
Inotropic Drugs and Cardiac
Glycosides
Interactions
K-wasting diuretics and other drugs causing K loss increase risk
of toxicity
Amiodarone, diflunisal, diltiazem, nifedipine, quinidine,
verapamil increase the serum drug level and may cause toxicity
Concurrent use of beta adrenergic blocking drugs causes
additive bradycardia
Antacids, cholestyramine, and colestipol decrease the absorption
of cardiac glycosides
Digitalis preparations
Examples: Digitoxin (long ½ life –not used often), digoxin
Nursing responsibilities
Digoxin excreted unchanged by the kidneys, dosage must be
reduce with renal impairment
Monitor serum digoxin levels to prevent toxicity
Digoxin Immune Fab IV to reverse toxicity
131
Antihypertensive Drugs
Antihypertensive drugs
Indications
Classes
HTN not controlled by life style modifications
Beta-adrenergic blocking drugs, angiotensinconverting enzymes (ACE) Inhibitors, angiotensinreceptor blockers,(ARB’s), calcium channel blockers,
alpha 1 blockers, centrally acting alpha 2 agonists,
diuretics, peripheral acting vasodilators
Contraindications and precautions
Each class has own action, side effects, specific
recommendations and adverse reactions
132
Antihypertensive Drugs
2nd line agent
Peripheral vasodilating drugs
Drug examples: hydralazine
Mechanism of action: exert direct action on both
arteries and veins to decrease peripheral vascular
resistance (with beta blockers)
Indications: treatment for hypertension and
hypertensive crisis
Adverse effects: fluid retention, tachycardia,
orthostatic hypotension, severe hypotension and
nausea
Nursing responsibilities
Closely monitor for fluid volume excess
Rarely used
133
Antihypertensive Drugs
ACE Inhibitors (1st line agent)
Drug examples: benazepril, catopril, enalapril, fosinopril, lisinopril
Mechanism of action: block conversion of angiotensin I to
angiotensin II
Mode of Action
Vasodilation due to inhibition of Renin Angiotension Aldosterone
system, decreased blood volume due to decreased (Sodium) Na+
Adverse effects: dizziness, light-headedness, fainting, tachycardia,
palpitations, rash, proteinuria
Nursing responsibilities
Not effective with African Americans
Do not give with Na+ sparing diuretics
Monitor for dry cough
Contraindicated in pregnancy and renal stenosis
Not to be given with lithium and caution with NSAIDs
Indications: HTN, CHF, diabetes, Angina
134
Antihypertensive Drugs
Calcium channel blockers (1st line agent)
Drug examples:
Mechanism of action:
Grapefruit juice can cause toxic overdose
Dizziness, AV blocks, headache, edema, flushing, nausea,
constipation, bradycardia
P-450 interaction with other meds
Do not give with grapefruit juice- can cause toxic overdose
Nursing responsibilities
Dilate vessels by blocking the slow channel, preventing calcium
from entering the cell
Adverse effects:
Amlodipine, diltiazem, felodipine, verapamil, nifedipine
Watch for weight gain if CHF
Indications: Angina, arrhythmias, HTN
135
Antihypertensive Drugs
Diuretics – thiazide (1st line agent)
Drug examples: chlorothiazide, hydrochlorothiazide
Mechanism of action: inhibit sodium and chloride
reabsorption, distal tubule, reduce blood volume
Adverse effects:
Fatigue, dizziness, orthostatic hypotension, rash,
hypokalemia, hyperglycemia
Indications: 1st line for HTN, take in the morning
Diuretics – loop
Mechanism of action: Loop of Henley, reduce blood
volume example: furosemide (Lasix)
Adverse effects: electrolytes
136
Indications: CHF
Antihypertensive Drugs
Selective Beta Blockers – 1st line agent
Drug examples: Atenolol
Mechanism of action: Selectively block beta 1 receptors in
the heart so slows heart rate – chronotropic effect and –
inotropic effect
Adverse effects: Bradycardia, rebound HTN if abruptly
stopped, fatigue, dizziness, dyspnea
Indications: HTN, Prophylaxis for angina, CHF, post M.I.
for cardioprotective effects
Nursing responsibilities: Monitor pulse, watch for drug
interactions (CCBs), potentiated by alcohol and other CNS
depressants, give cautiously with asthma patients
137
Antihypertensive Drugs
Angiotensin-receptor blockers
Alpha 1 blockers
Centrally acting alpha 2 agonists
All 2nd line agents
138
Antianginal Drugs
Mechanism of action:
Indication:
Hypotension, uncorrected hypovolemia
Adverse effects:
Angina pectoris
Contraindications:
Reduce myocardial oxygen demand or increase coronary
blood supply
Flushing, headache, orthostatic hypotension
Interactions:
Produce additive hypotension when used with alcohol,
antihypertensives, beta-adrenergic blocking drugs or
calcium channel blocker drugs for erectile dysfunction.
139
Antianginal Drugs
Nitrates
Drug examples:
Erythrityl
tetranitrate, isosorbide dinitrate (Isordil)
Nitroglycerin, Nitro-BID
Mechanism of action:
Produce
vasodilation. Decrease preload and
afterload, and reduce myocardial oxygen
consumption
Indications:
Management
of angina, and chronic anginal attacks
Beta Blockers and Calcium Channel Blockers also
for long term management
140
Diuretic Drugs
Thiazide and thiazide like diuretics
Drug examples: Clorothiazide, hydrochlorothiazide
Mechanism of action: Increase sodium and water
excretion by inhibiting sodium reabsorption in the distal
tubule of the kidney
Contraindications: Sensitivity to sulfonamides
Adverse effects: Hypokalemia, hyperglycemia,
arrhythmias, orthostatic hypotension, weakness, muscle
cramps, photosensitivity reactions
Interactions:
Decrease excretion of lithium causing toxicity
Concurrent use with other K-depleting drugs and cardiac
glycosides may cause low K and risk of digitalis toxicity
NSAID may reduce response to thiazide diuretics
141
Do not take if allergic to sulfa drugs
Diuretic Drugs
Loop diuretics
Drug examples:
Bumetanide
(bumex) ethacrynic acid, lasix, torsemide
Mechanism of action:
Inhibit
sodium and chloride reabsorption from the
loop of Henle and the distal tubule
Adverse effects:
Metabolic
alkalosis, hypovolemia, dehydration.
Hyponatremia, hypokalemia, hypochloremia,
hypomagnesemia, photosensitivity, orthostatic
hypotension
142
Diuretic Drugs
K-sparing diuretics
Drug examples:
Mechanism of action:
Act at the distal tubule to cause excretion of sodium,
bicarbonate, and calcium and conservation of K
Adverse effects:
Amiloride, spironolactone, triamterene
Hyperkalemia, nausea, vomiting, diarrhea
Interactions:
Decrease excretion of lithium
Concurrent use with ACE inhibitors or K increases risk
of hyperkalemia
NSAIDs may reduce the effects of K sparing diuretics.
143
Give cautiously with renal insufficiency patients
Diuretic Drugs
Osmotic diuretics
Drug examples:
Mannitol,
Urea
Mechanism of action:
Increase
osmotic pressure of the glomerular
filtrate inhibiting reabsorption of water and
electrolytes
Osmotic diuretics create an osmotic gradient in the
glomerular filtrate and the blood
Adverse Effects:
Hyponatremia,
rebound IICP
dehydration, circulatory overload,
144
Antilipemics
WE EAT TOO MUCH FAT
in the typical American diet.
DRUGS TO LOWER CHOLESTEROL:
VDRL, LDL and TGs
Syndrome X
metabolic syndrome
Glucose intolerance
Insulin resistance
Hypertension
Dyslipidemia
Hypertriglyceridemia
Associated with
Cardiac Disease
Male-shaped obesity
Female hip-to-waist ratio
146
Classes that lower lipids
HMG-CoA Reductase Inhibitors or
Statins
Nicotinic Acid
Fibric Acid Derivatives
Cholesterol Absorption Inhibitors
•Bile Acid Sequestrants
147
Anticoagulant, antiplatelet
and thrombolytic drugs
Anticoagulant drugs prevent extension
and formation of clots by inhibiting
factors in the clotting cascade
Thrombolytic drugs activate
plasminogen, leading to its conversion to
plasmin
Antiplatelet drugs interfere with platelet
aggregation, preventing thromboembolic
events
148
Common Pathway
Vit. K + warfarin
Heparin +
antithrombin =
Activated Heparin
Factor X
Low molecular
weight heparin
Prothrombin
(factor II)
Thrombin
Fibrinogen
Thrombolytics
Fibrin clot
Photo Source: Used courtesy of E. McCabe,
RN, Santa Barbara City College
Clot
dissolves
plasmin
plasminogen
149
Anticoagulants
Examples: Dalteparin, enoxaparin, heparin, warfarin
Indications: prevent and treat thromboembolic
disorders such as DVT, PE, and atrial fibrillation with
embolization
Adverse effects: thrombocytopenia (with heparin)
Androgens, chloral hydrate, chloramphenical,
metronidazone, quinidine, sulfonamides, thrombolytic
drugs, and valproic acid increase the risk of bleeding
and enhance the effects of coumadin
Alcohol, barbiturates, estrogen-containing oral
contraceptives and foods high in Vitamin K increase
risk of clotting and may decrease effect of heparin
150
Heparin
Accidentally discovered by medical student
in 1916, used medically first time in 1935 on
humans
High molecular weight – called
unfractionated
Does not cross the blood brain barrier – can
be used during pregnancy
Half life IV = 45 to 90 minutes
Half life SQ = 60 to 120 minutes
Bioavailabity is about 20 to 30 %
151
Heparin
Destroyed by enzymes in the GI tract
Administered IV or SQ – IM = muscular
hematomas
Varying bioavailability
Monitor with - aPTT (activated partial
thromboplastin time) =
Preferred because more sensitive to
intrinsic pathway
152
Heparin
Highly protein bound = variable anticoagulation b/c
the ill have reactive proteins that also bind to heparin.
Most serious side effect is hemorrhage
Administer protamine sulfate by slow IV infusion to
neutralize heparin
Drug-drug interactions: antiplatelet drugs, NSAIDs oral
anticoagulants, nitroglycerin, cephalosporins,
penicillins, salicylates all may affect of heparin
Uses: Hemodialysis, open-heart surgery, prevention of
thromboembolism, post MI, inhibits platelets from binding,
DVT, PE, atrial fib, stroke prevention a.k.a. acute brain
attack or CVA
153
Anticoagulants
Nursing Responsibilities
Heparin given initially because of its rapid
action, then switch to coumadin over several
days until therapeutic level is reached
Heparin affects PTT and coumadin PT
Inject SQ in abdomen and do not aspirate or
rub at injection site
Protamine sulfate antidote for heparin
Vitamin K antidote for coumadin
Soft toothbrush and electric razor
154
Anticoagulants
Monitoring heparin therapy
Obtain baseline PTT
Administer a bolus dose of heparin IV, as
ordered
Follow with continuous infusion as ordered
Obtain follow up PTT at specified
Values> 1 ½ time the control
Continue to monitor
Assess for S/S of bleeding
Values < 1 ½ time the control
Contact MD
Anticipate dosage increase
Increase dosage as ordered
155
Low molecular wt. Heparin
example enoxaparin (Lovenox)
Given by SQ injection
Mainly Acts on factor X to begin the
coagulation cascade to inhibit the
conversion of prothrombin to thrombin.
Produces greater prothrombin effect than
binding to factor II as Heparin does.
Also called fractionated heparin
156
Low Molecular wt. Heparin
T.I.A.s
Ischemic symptoms
Unstable angina
Atherosclerosis
Non ST elevation M.I. a.k.a, Q wave M.I.
(without elevated enzymes - homocystine)
ST elevations a.k.a. acute M.I. (with elevated
enzymes- homocystine)
157
Low molecular wt. Heparin
High bioavailability and so more predictable
than heparin because binds to factor X
No routine testing required
Can be administered at home
Bleeding is main adverse effect
Usually weaned off and when stable onto
warfarin (Coumadin)
158
Oral anticoagulant
Warfarin (Coumadin)
AKA “rat poison”
May also be given IV, but rarely is
Bound tightly to plasma protein – other drugs
can displace + other proteins may be present
during tissue breakdown (example C- reactive
protein)
Very difficult to monitor PT (prothrombin time)
and dosed by INR (international normalized
ratio)
Long half- life 1 to 3 days
159
Warfarin (Coumadin)
Variable dosing and unpredictable; MUST COME
IN FOR FREQUENT MONITORING.
Used prophylaxis for deep vein thrombosis (DVT),
Pulmonary Embolus (PE), atrial fibrillation, off
label for recurrent Transient Ischemic Attack (TIA),
recurrent Myocardial Infarction (MI)
Suppresses coagulation activity by interfering with
the production of vitamin K-dependent clotting
factors in the liver.
Reduced amount of available Vitamin K for clotting
factors II, VII, IX and X
160
Warfarin (Coumadin)
Humans can not synthesize Vitamin K, but
bacteria in GI tract can
Treat excessive bleeding with Vitamin K
Watch for bruising
Careful in older adult because MANY drug
interactions and fall can cause excessive bleeding
Used to prevent clot formation in conditions such
as atrial fib, not acute situations
IV Heparin to PO warfarin administer the 2
drugs simultaneously for 2 to 3 days to ensure
continuous therapeutic anticoagulation
161
Antiplatelets
Clopidogel (Plavix) & ticlopidine (Ticlid) bind to
ADP (adenosine dephosphate) which inhibits its
effect on platelets (60 – 70% )
Aspirin inhibits thromboxane (TX2) in
Arachidonic Acid Pathway (30-40%)
Abciximab (ReoPro) binds to the GP IIb/IIIa
receptor and inhibits platelet aggregation (90%)
Tirofiban (Aggrastat) {new}
162
Antiplatelet Drugs
Drug examples:
Indications for use:
Aspirin, dipyridamole (persantine), Ticlopidine (Ticlid)
Prophylaxis for thrombo-embolic events
Ticlid – second line drug use to prevent stroke in high
risk individuals, decrease intermittent claudication, and
decrease graft occlusion after coronary artery bypass
Contraindications:
Active bleeding, thrombocytopenia, severe liver
impairment
Adverse effects: Bleeding, tinnitus, dizziness,
neutropenia (Ticlid)
163
Thrombolytic Drugs
Drug examples:
Alteplase (tissue plasminogen activator) (activase),
streptokinase, urokinase
Indications for use:
Drugs used to lysis coronary artery thrombi
Alteplase, streptokinase, and urokinase used to
treat PE
Streptokinase and urokinase used to treat DVT
and to clear arterial catheters and arteriovenous
shunt
MRI needed for CVA to determine cause
164
Thrombolytic Drugs
Contraindications: Recent streptococcal infection,
active internal bleeding
Adverse effects: urticaria, fever
Nursing responsibilities:
Monitor V/S for bleeding or hypotension, check
peripheral pulses to ensure circulation
Keep typed and cross matched blood on hand to
administer in case of hemorrhage
Thrombolytic drugs should be administered only when
the patient’s hematologic function and clinical response
can be monitored
Ensure that aminocaproic acid (Amicar), the antidote for
thrombolytic overdose, is readily available
165
Antiplatelet Drugs
Drug examples:
Indications for use:
Aspirin, dipyridamole (persantine), Ticlopidine (Ticlid)
Prophylaxis for thrombo-embolic events
Ticlid – second line drug use to prevent stroke in high
risk individuals, decrease intermittent claudication, and
decrease graft occlusion after coronary artery bypass
Contraindications:
Active bleeding, thrombocytopenia, severe liver
impairment
Adverse effects: Bleeding, tinnitus, dizzines,
neutropenia (ticlid)
166
Drugs Affecting the
Endocrine System
167
Thyroid Hormones
Thyroid replacement increases metabolism,
cardiac output, regulates cell growth and
causes diuresis.
Most commonly used: – thyroid and levothyroxine
(Synthroid)
Contraindications: – Recent MI, adrenal insufficiency,
hyperthyroidism
Side Effects: – Cardiac dysrhythmias
Adverse Effects: – Tachycardia, angina, hypertension,
insomnia, headache, anxiety, increased or decreased
appetite, menstrual irregularities, weight loss, heat
intolerance (“hot flashes”) and thyroid storm
168
Antithyroid Drugs
Used to treat hyperthyroidism
Most commonly used: – methimazole and
propylthiouracil which inhibit formation of thyroid
hormone
Contraindication: – Drug allergy, avoid in pregnancy if at
all possible
Side Effects: – Drowsiness, smoky colored urine, aching
Adverse Effects: – Increased BUN and creatinine,
enlarged thyroid, liver and bone marrow toxicity
Interactions:– Increase in activity of anticoagulants
Propranolol (Inderal) (non-selective beta blocker) given to
control symptoms before antithyroid drugs work 2-3 weeks
169
Insulin
Replaces insulin not made or made
defectively in the body.
Indicated primarily for Type I diabetes but may be used
with Type II
Requires careful dosing regimen
Contraindications: – Drug allergy to specific product.
Adverse Effect: – Hypoglycemia from overdose, weight
gain
Interactions: – corticosteroids, epinephrine,
furosemide, phenytoin, thiazides, thyroid hormones,
alcohol, anabolic steroids, MAO inhibitors
170
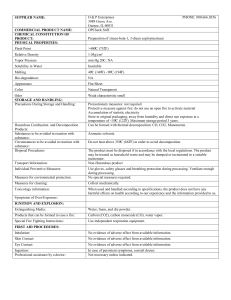
Action of Insulins
Preparation
Onset of Action
Peak Action
Duration of
Action
Humalog
10-15 minutes
30-60
minutes
5 hours or less
Regular*
30-60 min
2-4 hrs
6-10 hrs
NPH/Lente
1-2 hrs
4-8 hrs
10-18 hrs
Ultralente
2-4 hrs
8-14 hrs
18-24 hrs
Insulin glargine (Lantus) - a basal insulin for tighter glycemic control.
Do not mix with insulin. May be used also for type 2 glycemic control.
Regular insulin can be given IV in emergency situations
171
Sliding Scale (Rainbow Coverage)
Regular insulin is given according to blood
glucose results.
Used mostly with newly diagnosed diabetics
when stress occurs, such as illnesses requiring
hospitalization and surgery
Used with blood glucose greater than 200 mg/dl
Example:
4 units = 200 – 250
6 units = 251 – 300
8 units = Greater than 300
May need to call MD – Carefully check order.
172
Classes of agents for Type 2
SULFONYLUREAS
1ST generation
2nd generation
ALPHA-GLUCOSIDASE INHIBITORS
BIGUANIDES
MEGLITINDES
THIAZOLIDINEDIONES
INCRETIN MIMETICS (injected, new for type 2)
SYNTHETIC ANALOGS OF AMYLIN (injected,
new (1 & 2)
Insulin glargine for tighter control (1 & 2)
Inhaled insulin (1 & 2)
“EXTRA, EXTRA!
Two new classes!”
173
Complications of uncontrolled
Type 2
Vascular disease especially hypertension
Urinary Tract Infections (UTIs)
Vaginitis
Prostatitis
Retinopathy
Nephropathy
Nonketotic coma (uncontrolled)
174
Sulfonylureas (secretagogues)- means
stimulates the secretion of insulin
First generation
EXAMPLE=Diabinese
(chlorpropamide)
Potentiated by NSAIDs
Highly protein bound
P450 system so drug
interactions
Hypoglycemia
Stimulates pancreas
May increase incidence of
increased glucose intolerance
Rarely used today
Second generation
EXAMPLE=
Diabeta (glyburide)
Much the same as 1st
generation
May increase insulin
sensitivity
Also potential
hypoglycemia
175
Biguanides
EXAMPLES
Action
Metformin (Glucophage XR) &
Metformin (Fortamet XR)
Decrease hepatic glucose production
Increases insulin sensitivity
Decreases intestinal absorption of glucose
Improves lipid profile, decreases Triglycerides
DOES NOT produce hypoglycemia
Used as monotherapy or combination therapy
176
Biguanides
New use as prevention of Type II with FBS <
110 mg/dL > 125 mg/dL & History in family
May lower vitamin B12 levels ? Best to
supplement
Side effects: Usually good side effect profile, GI
symptoms, WEIGHT REDUCTION
Do not give to patients who are being treated for
CHF because of possibility of lactic-acidosis
177
Alpha-Glucosidase
Inhibitors
EXAMPLES
Action:
Acarbose (Pecose)
Miglitol (Glyset)
Blocks intestinal amylase so delays breakdown
of complex carbohydrates
Decreases postprandial glucose
Monotherapy or combination therapy
Side effects: are minimal - flatulence, diarrhea,
abdominal cramps
178
Thiazolidinediones
EXAMPLES
Pioglitazone (Actos)
Rosiglitazone (Avandia)
Action:
Reduce insulin resistance
Monotherapy or combination with sulfonylureas,
metformin
Enhance insulin action in skeletal muscle, liver
and fat tissue
Reduce hepatic glucose output
Glucose uptake into peripheral tissue
179
Thiazolidinediones
Precautions:
Side effects:
Do not use in patients with hepatic dysfunction
Monitor liver function tests
Caution with cardiac patients
In combination with other antidiabetic agents,
can cause fluid retention, may exacerbate CHF;
caution with insulin use
May cause edema and weight gain, headache,
upper respiratory infection
Does not cause hypoglycemia when used as
monotherapy
180
Meglitinides
(partial secretagogues)
EXAMPLES
Side effects:
Repaglidine (Prandin)
Taken ½ hour before meals
Rapidly absorbed
Needs presence of glucose to exert it’s action
Stimulates release of insulin
Potential for hypoglycemia, URI
Monotherapy or combination with metformin
181
Amino Acid Derivative
a secretagogue
EXAMPLE
Naeglinide (Starlix)
Give adjunct with diet & exercise
Give to those who have not been treated
chronically with other antidiabetic agents
Take 1 hr. to 30 min. before meals
Caution if patient is malnourished
Skip dose if meal skipped
Contraindicated in Type I and ketoacidosis
Not recommended in pregnancy
Monitor when concurrent highly protein-bound
182
drug given
183
Parathyroid hormone (PTH)
Stimulated by low serum calcium
Inhibited by normal or high levels of
calcium via negative feedback system
Phosphate also regulated by PTH via an
inverse relationship with calcium
PTH activates Vitamin D which increases
intestinal absorption
Less urinary excretion of calcium
Bone reabsorption of calcium from bone
184
Calcitonin & decreased PTH
Hypercalcemia decreases secretion of PTH
Calcitonin is synthesized in the thyroid
Calcium is lost in urine
Decreased absorption of calcium from the
intestine
Decreased reabsorption of calcium from bone
185
Vitamin D
In activated form acts like hormone (intermediate
metabolism in liver then to active form in kidney
called calcitriol)
Obtained from foods and by sunlight on skin
Deficiency limits amount of calcium absorbed
from diet
Causes release of calcium from the bone
(reabsorption)
Causes G.I. absorption of calcium
Decreased levels caused by medications including
tetracyclines and Dilantin
186
Osteoporosis
Risk factors
Current low bone mass (DXA) [dual energy xray absorptiometry]
Thin, small frame female
Advancing age
Family history of osteoporosis
Estrogen/testosterone deficiency
Anorexia nervosa
Low lifetime calcium intake
History of fracture after age 50
Smoking, alcohol and sedentary life style
Use of oral glucocorticoids for chronic disease
187
Drugs used for Calcium/bone Disorders
(osteoporosis & osteopenia)
Biphosphonates: alendronate (Fosamax), risedronate
(Actonel) new once a month ibandronate (Boniva)
used for osteopenia, osteoporosis, Paget’s disease
Action: undergo incorporation into bone.
Osteoclasts begin to reabsorb biphosphonatecontaining bone so they ingest some of the drug,
which then acts to inhibit their activity
All poorly absorbed from GI tract.
Take in a.m. with full glass of water, but without
food for 30 minutes and remain in upright position
to minimize risk of esophagitis.
188
Drugs used for Calcium/bone Disorders
(osteoporosis & osteopenia)
Thyroid hormone: Calcitonin (Miacalcin)
• Produced by body when low levels of
•
•
•
•
•
calcium
Used to treat osteopenia
Nasal spray
Suppresses bone reabsorption
Main side effect is runny nose and sneezing
Hormone Replacement Therapy
189
Mechanisms that raise
serum calcium levels
If decreased Serum Calcium
Parathyroid hormone secretion
renal excretion of calcium
Intestinal absorption of
calcium via activation of Vit D
Bone resorption so
calcium
190
Mechanisms that lower
serum calcium levels
If increased Serum calcium
Parathyroid hormone secretion
Calcitonin secretion
Renal excretion of calcium
Intestinal absorption of calcium
Bone resorption
Serum calcium
191
Arthritis
Osteoarthritis
Rheummatoid
arthritis (RA)
Excessive wear & Autoimmune
tear of wt.
disorder with
bearing joints
autoantibodies
(rheumatoid
factors)
Often thought as Systemic
normal part of
manifestations
aging process
Acute gouty
arthritis
Uric acid crystals
accumulate in
joints
Sudden onset,
triggered by diet,
injury/stress;
often big toe
192
Corticosteroids
There are 2 types – Glucocorticoids and
Mineralcorticoids
Cortisol is primary glucocorticoid
Aldosterone is primary mineralcorticoid
Some Indications:
Replacement therapy for Addison’s Disease
Inflammatory diseases
Arthritis
Ulcerative Colitis
Nephrotic syndrome
Liver disorders
Ocular inflammations
193
Corticosteroids (cont’d)
o
Some indications: (cont’d)
o
o
o
o
o
o
o
Allergic conditions – status asthmaticus,
asthma, allergic reactions
Neoplastic diseases
Brain-injuries (cerebral edema)
Skin conditions (psoriasis/dermatitis)
Collagen disease (Lupus)
Ophthalmic – conjunctivitis, corneal
abrasions
Asthma
194
Corticosteroids (cont’d)
Precautions:
Therapy is tapered and not discontinued abruptly
Vaccinations are contraindicated
Use with caution during pregnancy, lactation, clients
high risk for infections, peptic ulcer disease (PUD),
cardiac or renal failure, diabetes, myasthenia gravis
Do not use with fungal or viral eye infections
Interactions – Increased risk of:
Hypokalemia with K-depleting diuretics
Digitalis toxicity
Gastric ulcers with NSAIDS
Hyperglycemia
195
Estrogen
Indications:
Side Effects:
Hormone replacement therapy
Normal sexual development with estrogen deficiency
Androgen suppression with prostate Ca
Oral contraception by inhibiting ovulation
Headache
Depression
Adverse Effects:
Hypertension
Thrombo-embolic disorders
Abnormal uterine bleeding
Unopposed may lead to endometrial cancer
196
Estrogen (cont’d)
Contraindications:
Pregnancy and lactation
Previous or active thrombo-phlebitis or embolic disorders
Estrogen-dependent Cancers
History of CVA or Coronary Artery Disease (CAD),
Breast Cancer, liver disorders
Precautions:
Oral contraceptives by diabetics or smokers
Interactions: Some anti-convulsants decrease the
effectives of oral contraceptives due to P450 system
197
Progentins
(not progesterone)
Indications - Oral contraception with estrogen,
HRT, endometriosis, dysmenorrhea, uterine bleeding
Adverse Effects:
Breakthrough bleeding
Impaired glucose tolerance
Depression
Edema and weight gain
Contraindications:
Pregnancy, undiagnosed vaginal bleeding, Thrombophlebitic or embolic disorders, Ca of reproductive
organs
198
Androgens
Most important is testosterone
Uses:
Males – erectile dysfunction, delayed puberty, muscle
wasting in AIDS
Females – Endometriosis, fibrocystic breast changes,
some menopausal symptoms, advanced breast cancer
Females – increases libido
Adverse Effects:
Virilization, hepatotoxicity, edema, gynecomastia in
males
199
Androgens (cont’d )
Precautions:
Contraindicated in pregnancy and prostate
enlargement
Children must have bone growth evaluated q 6 months
Anabolic Steroids – Schedule III controlled substance
(not same as testosterone)
Testosterone
Interactions:
Enhance effects of oral anticoagulants, oral
hypoglycemics and insulin
Barbiturates and calcitonin interfere with the effects of
androgens
200
Drugs Affecting the
Respiratory System
Photo Source: National Cancer Society, Public Domain,
http://visualsonline.cancer.gov/details.cfm?imageid=1775
201
Antihistamines
Indications:
Various allergic reactions
Induce sleep
Relieve nausea
Prevent motion sickness
Side Effects:
Drowsiness
Dry mouth and blurred vision
Elderly
are at high risk for dizziness,
confusion, hypotension, unsteady gait & CNS
stimulation - Lower doses due to
anticholinergic effects
202
Antihistamines (cont’d)
Adverse Reactions:
Contraindications:
Headache, hypertension, GI distress
Drug allergy – anaphylaxis
Excessive sedation with other CNS depressants
Narrow angle glaucoma, prostatic hypertrophy,
pregnancy, bladder neck obstruction, PUD
Not recommended in bronchitis or pneumonia because
they dry secretions making it difficult for removal.
Interactions:
Some antibiotics enhance effects
MAOIs inhibit metabolism thus enhancing effects
203
Mode of Action Antitussives
narcotic antitussives directly
suppress cough reflex in
medulla of the brain (CNS)
dextromethorphan same
mode of action as narcotic
benzonatate anesthetizes or
numbs the cough reflex
Photo Source: Wikimedia Commons, Creative Commons,
http://commons.wikimedia.org/wiki/Image:Brain_bulbar_region.svg
204
Antitussives
Used to relieve coughs: suppresses cough center in
Side Effects for centrally acting:
medulla if centrally acting
Antitussives containing codeine are Schedule IV meds.
Dextromethorphan, non-opioid
Drowsiness, sedation, dizziness, restlessness,
agitation, euphoria
Adverse Effects:
Respiratory depression – antidote opioid toxicity
(Narcan)
Hypotension, Tachy or bradycardia
Drug allergy - Anaphylaxis
205
Drugs Affecting the Respiratory
System
Beta-Agonists inhaled - short acting +
long acting
Beta-agonists – oral agents
Methylxanthines
Anticholinergics
Antiasthmatics
[cromolyn & nedocromil]
Corticosteroids
Leukotriene modifiers
206
Bronchodilators
Used to relax smooth muscles in bronchi
and bronchioles for asthma, bronchitis,
emphysema
3 Types of Drugs
Adrenergics(beta -2)
Xanthines
Anticholinergics
(given by inhalation)
207
Follow step approach guidelines when doing
health teaching.
See health care provider at least every 6
months for evaluation.
Identify and list triggers.
Keep asthma diary & record “personal best”
from peakflow meter. Record three times a day.
Contact provider if peak flow drops and go to
established plan.
208
Step Approach Terms
Step one
Step Two
Mild Persistent
Step Three
Mild Intermittent
Moderate Persistent
Step Four
Severe Persistent
209
Beta-Agonists
Rescue drugs (short acting)
Used most often
During acute phase of asthmatic attack
For COPD acute attack of SOB
Quickly reduce airway constriction
Are Sympathomimetics
Stimulate beta-2 receptors
210
Anticholinergics
Corticosteroids
Indirect-acting Agents
211
Anticholinergics
Controller drugs
Ipratropium bromide = Atrovent
New powder inhaler (not metered dose inhaler)
24 hr. duration & may be superior to atrovent =
tiotropium bromide (Spiriva)
NOT for acute attacks!
For maintenance tx of bronchospasms
MAINSTAY FOR COPD (when combined with
atrovent is called Combvient – brand name)
212
Side Effects of Anticholinergics
Respiratory:
Gastrointestinal:
Dry mouth or throat and coughing
GI distress
CNS:
Headache & anxiety
Mild anticholinergic effects if inhaled – do not use if
patient has glaucoma or BPH
Atrovent or Combivent inhalers produce serious
allergic reactions to those with peanut allergy
213
Xanthine Bronchodilators
Controller agent
Aminophylline
*usually I.V. when patient
in distress
Theophylline
*[examples]
aerolate, bronkodyl, elixophyllin, slo-bid,
theobid, theo-dur, theolair, & uniphyl
214
Theophylline
Wide variability as to plasma half-life
Narrow therapeutic index
Unpleasant side effects of anxiety, agitation,
insomnia, tachycardia, palpitations
Need to draw blood samples to stabilize patient
on correct dosage to minimize adverse effects
Older adults with liver disease and CHF with
pulmonary edema have prolonged half-life
Smokers and children have shorter half-life
215
Antibiotic classes:
Sulfonamides, Penicillins,
Cephalosporins, Macrolides,
Quinolones, Aminoglycosides,
Tetracyclines, Glycycyclines
Carbapenems,
Monobactams, Oxazolidinones
Streptogramins, Ketolides &
Glycylcyclines
216
Drugs Used to Treat
Infections
Drugs for treating infections are referred
to as antibiotics (most common term) or
anti-infectives, antimicrobial
Antibiotics are not effective against
viruses
Resistance is the BIG PROBLEM
217
Anti-infectives General Action
Modifies
protein
synthesis
Damages
the cell wall
Types of
antibiotic action
Modifies
DNA
synthesis
Modifies
energy
metabolism
via folic acid
218
Antibiotics
Actions
Adverse Reactions:
Some are very nephrotoxic
Hearing impairment- ototoxic
Superinfections
May potentiate decreased effectiveness of other medications
(Be aware of specific interactions with specific drugs)
“Sunburn” reaction – Avoid direct sunlight with tetracyclines
Contraindications:
Inhibit the growth of bacteria
Inhibit cell wall synthesis
Are bacteriostatitic and bacteriocidal
Known drug allergy
Many should not be used during pregnancy
Many resistance patterns
219
Penicillin resistance
Penicillinases (enzymes) produced by
bacteria that destroy penicillin by cleaving
the beta-lactam ring of the drug
Clavulanic acid enhances the activity of
penicillins. Binds to the active sites of
penicillinases rendering the enzyme
inactive
220
Some Commonly Used
Antibiotics
Sulfonamides
One of the first anti-infectives
Often used today for Urinary Tract Infections
Drink fluids to prevent urinary crystals
Septra
Bactrim
Assess allergy to other sulfa medications
(Sulfonylureas,Thiazide diuretics)
Penicillins
Penicillin G, Ampicillin, Amoxicillin
Observe for clostridium difficule
Fruit juices can inactivate the drug
Assess electrolytes
221
Some Commonly Used
Antibiotics (cont’d)
Tetracyclines (not with milk, CA products)
Take one hour before or two hours after meal
Causes brown teeth in children!
Photosensitivity
Macrolides – Erythromycin and Biaxin can have
many drug interactions, problems with G.I. distress
Used to treat mycoplasma (penicillins & cephalosporins
not effective!)
Used when patient is allergic to penicillin
Use cautiously with heart, renal, liver disease
Not given with fruit juice
222
Cephalosporins
• Similar to PCN but broader spectrum
• Differ as to generation for coverage. When
anaphylaxic reaction to PCN, should not be
given a cephalosporin
• A beta-Lactam antibiotic
• May be ineffective against bacteria that produce
enzyme beta-lactamase
• Called cephalosporinase
• Avoid alcohol. Also, now may not be effective
against MRSA
223
Quinolones
Kill bacteria = bactericidal
Active on a wide variety of bacteria
gm- & gm+ as well as a-typical infections
Excellent oral absorption
Antacids reduce their absorption
* gm- coverage & excellent [drug] for kidneys
Great for treating UTI’s & prostatitis first oral class
of antibiotic to kill gram- bugs
Good for Salmonella typhi and Shigella
Not used in children. May damage cartilage,
leading to deformities in gait
224
Quinolones
Used to treat:
lower respiratory tract infections
bone & joint infections
infectious diarrhea
urinary tract infections
skin infections
Overuse! They should be reserved for serious
infections and resistant strains. MRSA can be
susceptible. Do not want to create resistance
Should not be used in children - may damage
cartilage leading to deformities in gait
225
Aminoglycosides
Used to Treat:
Pneumonias, resistant UTIs, septicemia, CNS
infections – serious & life threatening
Action:
Bind to 30S & 50S ribosomal subunits
Cause inhibition of protein synthesis
Precautions:
Nephrotoxicity & ototoxicity (8th cranial nerve)
Drug levels help prevent high peaks & troughs,
many drug interactions; must monitor carefully.
226
Miscellaneous antibiotics
Vancomycin
Rapidly bactericidal so low resistance
Glycopeptide antibiotic not related to PCNs
Given by intermittent IV infusion
Used in life-threatening staph or strep infections and
MRSA
Adverse reactions are nausea, flushing and itching
Red Man Syndrome
Toxic reactions: tinnitus, hearing loss, nephrotoxicity
Often given with piperacillin (Zosyn) IV a broad
spectrum PCN + B-lactamace inhibitor for MRSA
227
Antituberculars
Ethambutol (Myambutol)
INH isoniazid (Nydrazid)
Hepatotoxicity & hyperuricemia
(reports of liver failure)
Rifampin
Peripheral neuritis & rarely hepatotoxicity
Don’t give for prophylaxis after age 40
because of increase in side effects
Peripheral neuropathy
Selegiline (SEL)-like syndrome
Pyrazinamide
RARE retrobulbar neuritis & blindness
GI upset
Hepatitis, body fluids turn orange/red color
Streptomycin
228
Latent TB
If skin test is positive
Follow up with chest x-ray
Use INH for 9 months or rifampin for
4 months for latent TB
229
Antifungal Agents = drug interactions +
liver toxicity
Examples of systemic antifungals
Itaconazole (Sporanox): inhibitor of cytochrome
3A4 = increased statins, Ca + channel blockers,
some Benzodiazipines, etc.
Ketoconazole (Nizoral): inhibitor of
cytochrome 2C19 = increased levels of
phenytonin, some Tricyclic Antidepressants,
some Benzodiazipines, etc.
Fluconazole (Diflucan): inhibitor of
cytochrome 2C9 = increased level of celebrex,
NSAIDs, Warfarin, phenytoin, etc.
230
Antivirals
Drugs used to kill viruses
Inhibit their ability to replicate
Difficult to kill because they live inside our cells
Utilize
our cells to replicate
Any drug that kills a virus may kill our cells
Only work during viral replication
Mutations & resistance common
Antimicrobials not effective unless accompanying
secondary bacterial infection
231
Photo Acknowledgement:
Unless noted otherwise, all photos
and clip art contained in this module
were obtained from the
2003 Microsoft Office Clip Art Gallery.
232