Laboratory Investigation of Infectious Diarrhoea
advertisement

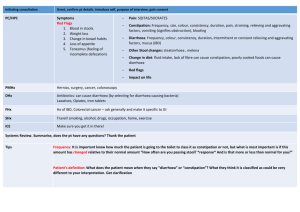
Laboratory Investigation of Infectious Diarrhoea Key Messages • Laboratory investigations are not routinely required for most patients with acute diarrhoea • A single stool specimen for faecal culture is usually appropriate • Giardia and cryptosporidium should only be requested if there are risk factors • “Ova and parasites” is rarely indicated • Notifiy the MOH in outbreaks Introduction • Infectious diarrhoea is the most common cause of diarrhoea • Leading cause of childhood death in undeveloped countries • In New Zealand, the elderly are most vulnerable • On average 1.2 – 1.9 diarrhoea illness/person/year • NZFSA estimates 6.5 million cases/year and 5 million lost working days Defining diarrhoea Diarrhoea is a change in bowel habit for the individual that results in substantially more frequent and looser stools. Diarrhoea may be defined as: • Acute if the duration of symptoms is <14 days • Persistent if it has lasted > 14 days • Chronic when symptoms have been present for more than four weeks Differential diagnosis Consider: • Gastrointestinal infection • An associated symptom of an acute systemic infection/illness • Drugs/diet • Gastrointestinal conditions - acute abdomen e.g. appendicitis, inflammatory bowel disease, malabsorption, tumour • Others as clinical picture dictate e.g. thyrotoxicosis Causes of acute infectious diarrhoea in New Zealand Bacterial Virus Campylobacter Norovirus Salmonella Rotavirus Clostridium difficile Enteric adenoviruses Yersinia Shigella E coli 0157* Vibrio Protozoa Giardia Cryptosporidium *E coli 0157 = verotoxin producing E coli (VTEC) Clinical details For people with acute diarrhoea, it is important to: • determine the severity of their condition • identify if a pathogen may be causative • to check the physical status of the person History: assessing severity • Frequency and duration • Presence of blood or mucus, abdominal pain, or fever • Signs of dehyration • General medical history/social support • Pregnant women who may infect newborn History: identifying pathogen • Alternative water sources, consumption of raw or undercooked meat, raw seafood (Vibrio), unpasteurised milk (E coli, Salmonella, campylobacter) • Travel to undeveloped area (wide range pathogens) • Unwell patient contacts (Shigella, E coli, Salmonella, Campylobacter, Giardia) History: identifying pathogen …contd • Recent hospitalisation or antibiotics (C. difficle) • Swimming in fresh water lake, swimming pools (E coli, Salmonella, Campylobacter, Cryptosporidium) • Recent visit to farm, or contact with pets with diarrhoea (E coli, Salmonella, Campylobacter, Cryptosporidum) Physical examination • Vital signs/abdominal examination/other examination as indicated • Determine the hydration status of patient • Exclude other causes Indications to send specimens to the laboratory Specific investigations are not required for most patients. A laboratory diagnosis is useful for people who: • may have an infection that could benefit from specific therapy, • are at risk of severe complications, • at risk of spreading infection, or • are involved in an outbreak. What samples are required? No risk factors No laboratory tests Culture Single fresh stool sample Giardia and crytpsporidium Single fresh stool sample Ova, cysts, parasites 1-3 stool samples Which tests to request? Culture Giardia crypto No risk factors Ova, cysts C.diff No tests Food handler + < 5 years + Childcare attendance + + Rural + + Raw seafood + Blood in diarrhoea + Antibiotics/chemo + Recent hospitalisation + >70 years + + Immunocompromised + + + Travel/immigrant + + + Persistant diarrhoea + + + Faecal culture first: send only one sample • Approximately 150 000 faecal cultures are requested each year New Zealand • Most of these are part of a series of faecal culture tests i.e. two or more specimens sent over several days. • When testing is required, a single faecal culture is the appropriate first line test Giardia and Cryptosporidium: direct antigen test on single faecal specimen • Testing is indicated when a person has diarrhoea: – For longer than seven days – Following recent overseas travel, tramping trip or drinking from rivers/springs – Following attendance at a child care centre – Is immunocompromised – Cryptosporidium is also associated with lambs and calves, and there are occasionally outbreaks in swimming pools. Ova and cysts are rarely indicated • In New Zealand the most likely causes of parasite diarrhoea are Giardia and Cryptosporidium. • Testing for ova and cysts is only indicated for people who have: – Recently travelled to countries with poor food or water sources – Recently immigrated – Eosinophilia with diarrhoea lasting longer than 15 days – Immunocompromised status Viral Causes • Viral infection is probably the most common cause of infectious diarrhoea • Rotavirus is a common cause of diarrhoea in infants and young children – Management should focus on hydration status. – Faecal testing is not routinely indicated. • Norovirus is frequently implicated in outbreak situations. – Laboratory testing in outbreaks is managed by the Medical Officer of Health. Clostridium difficile toxin • C. difficile is the major identifiable cause of antibiotic-associated diarrhoea. • The prevalence of asymptomatic colonisation of the bowel ranges from <5% in the community to over 20% in hospitalised patients. It is more prevalnt in the elderly. • C. difficile toxin testing is indicated for patients who develop diarrhoea while in hospital, on antibiotics or receiving chemotherapy. Listeria monocytogenes • Infection with Listeria monocytogenes can cause febrile gastroenteritis accompanied by bacteraemia and sometimes meningitis. • Infection during pregnancy may be complicated by amnionitis and foetal infection. • Diagnosis requires blood cultures. Clinical information is important for the laboratory • Blood and mucus in the stool, hemolytic-uremic syndrome (HUS) will generate culture on a special agar for E. coli 0157 (VTEC). • Ingestion of raw seafood will generate culture specific for Vibrio species. • Recent hospitalisation or antibiotic will generate testing for Clostridium difficile toxin. Specimen collection • Most laboratories have patient information sheets available explaining specimen collection. • Rectal swabs may be used for babies or children when collection of a faecal specimen is impractical. • The causative agent in cases of infectious gastroenteritis is most likely to be found in faeces specimens obtained when the patients are actually experiencing diarrhoea. • The yield from faeces collected in convalescence is reduced. • Patients should collect enough faeces to approximately half fill the specimen container. • Specimens should be kept cool (preferably at 4°C) and taken to the laboratory as soon as possible and within 24 hours. Specimen containers Test Specimen container Culture Fresh stool with no additive Giardia and Crypto Fresh stool with no additive Rotavirus Fresh stool with no additive Ova, cysts, parasites Check with your local laboratory. Some will provide a special container with fixative, others will accept fresh samples and add fixative themselves. Notifiable diseases • Notification of diseases and conditions is a legal requirement under the Health Act 1956. • Disease surveillance can be used to help prevent and control the spread of diseases. • Both GPs and laboratories are required to notify the Medical Officer of Health of the possibility of a notifiable disease. • The local public health unit will manage the testing of faecal specimens in an outbreak situation. Conditions that are notifiable to a Medical Officer of Health Acute gastroenteritis * Yersiniosis Campylobacteriosis Cholera Giardiasis Taeniasis Cryptosporidiosis Typhoid and paratyphoid fever Shigellosis Listeriosis Salmonellosis *Not every case of acute gastroenteritis is necessarily notifiable – only those where there is a suspected common source or from a person in a high risk category (eg, food handler, early childhood service worker, etc) or single cases of chemical, bacterial, or toxic food poisoning such as botulism, toxic shellfish poisoning (any type) and disease caused by verocytotoxic E. coli. Cases and rates per 100 000 population of notifiable diseases in New Zealand for 2005 and 2006. Disease 2005 2006 Cases Rates Cases Rates Campylobacteriosis 13836 337.6 15873 383.5 Cryptosporidiosis 889 21.7 736 17.8 Gastroenteritisa 557 13.6 931 22.5 Giardiasis 1231 30.0 1214 29.3 Salmonellosis 1382 33.7 1335 32.3 Shigellosis 183 4.5 102 2.5 VTEC/STEC infection 92 2.2 87 2.1 Yersiniosis 407 9.9 487 11.8 Causative agent: Campylobacter • Sources of infection: Contaminated food or water, in particular undercooked chicken or other meats . • Incubation period: 1 to 10 days (usually 2 to 5 days ) • Symptoms: Watery or bloody diarrhoea, abdominal pain and nausea preceded by muscle pain, headache and fever. Symptoms may last 1 day to 1 week or longer (usually 5 days). • Organism Survival: Organism survives better in food under refrigeration than at room temperature. Rapidly deactivated by heating to 55oC • Treatment: Usually none, but fluids may be given. Some cases warrant treatment with antibiotics. Causative agent: Salmonella • Sources of infection: Undercooked food e.g. chicken, eggs and meat; food or water contaminated with faeces from an infected person or animal • Incubation period: 6-48 hours (usually 12-36 hours). • Symptoms: Diarrhoea, abdominal pain, vomiting, nausea and fever lasting 1-7 days. • Organism Survival: Salmonella can survive up to 28 days under refrigeration, even on the surface of vegetables which have become contaminated. Deactivated by heating to 70oC • Treatment: The infection is usually self-limiting although fluid replacement may be required. Causative agent: E coli 0157:H7 • Sources of infection: In New Zealand, most from food or water contaminated by the faeces of a ruminant animal; or direct spread from an infected person • Incubation period: 3 to 9 days (mean 4 days) • Symptoms: Symptoms range from no symptoms to kidney disease and death. In more serious cases there is a period of bloody diarrhoea followed by HUS*. The elderly may suffer from TTP#. • Organism Survival: Survives well in chilled and frozen foods Rapidly deactivated by heating to 71oC. • Treatment: Usually none, but fluids may be given. Special management for HUS and TTP * HUS = haemolytic uraemic syndrome # TTP = thrombotic thrombocytopaenic purpura Causative agent: Giardia / cryptosporidium • Sources of infection: Food or water contaminated with faeces from an infected person or animal. • Incubation period: Giardia: One to 3 weeks after infection. (mean about 7 – 10 days) Crypto: 1 – 12 days (mean about 7 days) • Symptoms: May be asymptomatic or cause GI upset. Serious disease may occur in the immunocompromised. Symptoms may last from 4 to 6 weeks, and consist of diarrhoea followed by flatulence, foul-smelling stools and cramps. • Organism Survival: In general the cysts are stable and can last for long periods (months) in the environment. Heating cysts to 60-70oC for 10 min inactivates them. Treatment: Most cases are self-limiting, but antibiotics may be indicated. Causative agent: Shigella • Sources of infection: Food or water contaminated with faeces from an infected person or animal; • Incubation period: 12 hours to 4 days. In outbreaks incubation times of up to 36 hours are observed. • Symptoms: Abdominal pain, diarrhoea, fatigue, malaise and fever. Mucus and occasionally blood appear in the faeces. The illness may progress to the “colonic phase” within 1-3 days where the symptoms are intense cramps as well as frequent and painful bowel movements. Lasts for 3 to 14 days. • Organism Survival: In general they survive best at low temperatures (subzero and refrigeration). Can survive storage in butter for more than 100 days at – 20oC and 4oC. Rapidly inactivated at temperatures above 65oC. • Treatment: Antibiotic treatment is not required in milder cases. Resistance is common. Causative agent: Yersinia • Sources of infection: Food or water contaminated with faeces from an infected person or animal: farm animals (especially pigs), infected pets (puppies and kittens) • Incubation period: Approximately 7 days, range 1-11 days • Symptoms: Abdominal pain, headache, fever, diarrhoea, nausea and vomiting. Often produces a watery/mucoid diarrhoea in children. Approximately 2/3 of cases report being ill for >1 week. • Organism Survival: Can grow in the presence or absence of oxygen. Able to grow in refrigerator temperatures. Rapidly inactivated at 60oC. • Treatment: Usually self limiting, antibiotics do not reduce the severity or duration of the illness. May used in more serious manifestations of the disease. Instructions for the collection of faeces • Label the specimen jar carefully, with your name, age/date of birth and date of collection. • Place a large clean container (e.g. disposable container) in the toilet bowl. Pass faeces directly into the container. • Do not contaminate faeces with urine. • Using a wooden spatula or similar, scoop enough of the faeces to at least half fill the specimen jar. If a specimen jar is not available, place a sample at least as large as a golf-ball into a clean jar. • Dispose of excess faecal matter from container into the toilet, then place inside 2 plastic bags and dispose of in domestic waste. • Screw the lid on the specimen jar firmly. Place in a zip-lock plastic bag. • Keep specimen cool but DO NOT FREEZE. Natural Toxins in Food Food Precautions Apple and pear seeds Apricot and peach kernels Eat no more than 1-2 apricot kernels per day. Young children should avoid swallowing seeds Parsnip Avoid parsnip that are damaged or mouldy. Levels of toxin drop with cooking. Discard cooking water Potatoes Do not eat sprouts or green potatoes, they remain toxic even when cooked. Store potatoes in the dark, to minimise production of glycoalkaloids (green potatoes) Kidney beans Kidney beans must be soaked (for 5 hours) prior to cooking. As few as 4 – 5 raw beans can produce symptoms. Rhubarb Large quantities of rhubarb would need to be consumed to cause death. Zucchini Very occasionally occurs in home grown zucchini, rarely found in commercially grown zucchini. Discard zucchini with unpleasant smell or bitter taste. Cassava Grinding cassava to a fine powder effectively removes the toxin. Bamboo shoots Can be fatal. Degrades easily with prolonged boiling to safe levels