Learner with Traumatic Brain Injury, Deaf-Blindness

Patrick Rocha
EEX 5051
6/8/09
TBI: Injury to the brain after birth resulting in total or partial disability or psychosocial maladjustment that effects educational performance; may affect cognition, language, memory, attention, reasoning, abstract, thinking, judgment, problem solving, sensory or perceptual and motor disabilities, psychosocial behavior, physical functions, information processing, or speech. http://www.youtube.com/watch?v=_938gpoBbvc Geoffrey’s Story
Deaf-Blindness: defined by significant impairments in both hearing and seeing, although the individual may have some residual hearing or sight.
Low Incidence, Multiple, & Severe Disabilities: occur relatively infrequently and require extensive support in more than one major life activity, such as mobility, communication, self-care, independent living, employment, and self sufficiency.
• One percent of all learners are considered Low Incidence, Multiple, & Severely
Disabled.
-
-
-
-
-
Open head injury: an open wound in the head, such as a gunshot wound or penetration of the head by an object, resulting in damage to brain tissue.
Closed head injury: occurs without penetration of the skull; might be caused by a blow to the head or violent shaking by an adult.
Causes:
Child abuse, shaking a baby or toddler.
Vehicular accidents, accounts for the majority of TBI.
Assault and gunshot wounds to the head, more prevalent among youths.
Prevalence:
Males are more prone to TBI, yet males and females tend to obtain
TBI in later adolescence and early adulthood.
“Silent epidemic”
-
-
-
-
-
-
-
-
-
-
-
-
Characteristics:
TBI is “invisible.”
Problems with short term and long term memory, learning new information, as well as speech and language problems.
Difficulty sequencing things and processing new information.
Able to do some things but not others, quick gains sometimes, no gains other times.
Inappropriate mannerisms.
Failure to understand social situations and humor.
Becomes easily tired, frustrated, or angered.
Unreasonable fear or anxiety, irritability.
Sudden mood swings, depression, aggression.
Change in personality, going from an adult to child-like. (Phineas
Gage)
Persistent repetition of one thought or behavior.
http://www.neuroskills.com/brain.shtml
Diagnosis:
Patients suffering TBI are typically brought to a hospital emergency room for initial diagnosis and treatment. Once vital signs are assessed and stabilized, and other life-threatening injuries are identified and treated, the process of diagnosing the extent of brain injury begins.
A complete neurological evaluation is performed to rule out conditions requiring neurosurgical attention, such as hematomas, depressed skull fractures, and elevated intracrantial pressure (ICP). X-rays, CT scans , and/or
MRI scans may be performed to determine if the bones of the skull are fractured and if bone fragments have penetrated the brain tissues.
The patient may be presented with a series of questions (What is your name?
Where are you? What day is it?) and given simple commands (Wiggle your toes. Hold up two fingers.) to determine if he or she can open their eyes, move, speak, and understand what is happening around them. If possible, a detailed medical history is performed to identify any previous injuries, existing seizure disorders, learning disabilities, prior psychiatric or psychological treatment, and/or substance abuse.
The patient's degree of consciousness is assessed to determine the severity of brain injury and predict his or her chances for recovery.
Glasgow Coma Scale: tests a patients eye opening response, best motor response, and best verbal response.
-
-
-
-
-
-
-
-
-
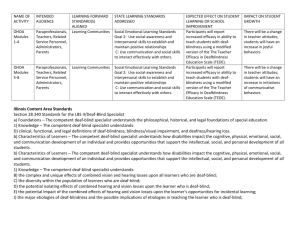
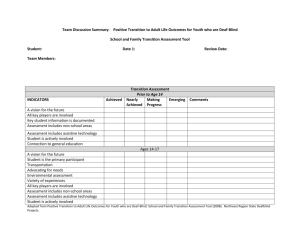
Treatment/Educational Considerations:
Transition from rehab center/hospital to school.
At school, a team approach from faculty and staff is put into place.
IEP is used to track the progress of the student.
Educational procedures test a students attention span, learning new things and memory of facts and skills, cognitive process.
Addresses long term goals along with goals of the IEP.
Teacher needs to help student deal with behavior and emotions.
Retrain motor-speech skills
Medication must also be taken into consideration depending on the severity of the student/patient.
Activity: http://faculty.washington.edu/chudler/chmemory.html
-
-
-
-
The Individuals with Disabilities Education Improvement Act of
2004 describes a deaf-blind individual as:
Having a central visual acuity of 20/200 or less.
Chronic hearing impairment that so severe that most speech cannot be understood.
The combination of both impairments causes extreme difficulties in attaining independence in daily life activities.
The inability to measure accurately through performance assessment.
The definition has caused some controversy due to it being vague by definition. Many states have added to the definition in order for it to become more specific.
-
-
-
-
Major Characteristics:
Individuals who cannot hear or see, or who have a severe problem with doing both.
Prevalence:
Many people who are deaf-blind also have other disabling conditions.
Research indicates that there are about 10,000 individuals from birth to twenty two years old who are deaf-blind.
Adults account for 35,000 to 40,000 of the deaf-blindness population.
-
-
-
-
Causes:
Genetic/Chromosomal Syndromes: Charge syndrome, Usher syndrome, and Down syndrome.
Charge syndrome: characterized by physical anomalies, abnormalities of the retina, cranial nerves, heart defects, atresia, retardation in growth and mental development.
Usher syndrome: an inherited syndrome resulting in hearing loss and retinitis pigmentosa, a progressive condition characterized in seeing low light and tunnel vision. *
Down syndrome: chromosomal abnormality, characterized by intellectual disabilities and such physical signs as slantedappearing eyes, hypotonia, a single palmar crease, shortness, and a tendency towards obesity.
-
-
-
-
Causes Cont…:
Prenatal Conditions: occurs or develops in the fetus before birth.
Common types are rubella aka German measles and congenital cytomegalovirus, which causes intellectual disability and deafblindness.
Postnatal Conditions: occurring in an infant after birth.
Common type is meningitis and TBI.
-
-
-
Developmental Affects:
Problems accessing information
Problems communicating.
Problems navigating the environment.
-
Diagnosis:
We need to have as clear an idea as possible of what a child hears and what he sees. This essential information will enable us to imagine, with as much accuracy as possible, his experience of the world so that we may thereby connect with his and help him to connect with the world around him. The importance of these assessments is often underestimated, especially where a child with multiple disabilities is concerned. Indeed, the use of clinical assessment, combined with specialized functional assessment, is essential in the process of enabling the student with deaf-blindness to join families, friends and environment.
Medical assessment is also a very important component of the diagnosis and assessment process. Many medical treatments exist that can result in a dramatic improvement in seeing and hearing. These can range from the prescription of medication, removal of middle ear fluid, and the surgical treatment of glaucoma. Because so many children are Deaf-Blind in addition to vision and hearing impaired, we must take every opportunity to ensure that we are maximizing the use of every avenue of learning and preserving whatever residual senses exist.
-
-
-
-
-
-
-
Educational Considerations:
Direct teaching
Structured Routines
Communication: your hands become a “voice” for students, Braille, hand-over-hand guidance, hand-under-hand guidance, adapted signs and finally, touch cues.
http://www.youtube.com/watch?v=F8DiZbCu3TM&feature=relate d&pos=0 Intervenor for Deaf-Blind Persons (Short Version)
Orientation and mobility: allowing students to navigate the environment around them. Assistance cards, contains message that alerts the public that the user is deaf-blind and needs assistance.
Considerations for students with Usher syndrome:
Most students have progressive visual impairment, so the introduction of Braille and orientation and mobility must start at an early age.
-
-
-
-
-
-
Augmentative or alternative communication (AAC):
Alternative forms of communication that do not use the oral sounds of speech or that augment the use of speech.
Simplified sign language which represents icons.
Pointing with the hand or a headstick, eye movements, or operation of a microswitch by foot, tongue, or head movement or breath control, Touch Talker.
Typewriter or computer terminal that is fitted with a key guard so that the keys are not likely to be pressed accidently.
Communication boards: an array of pictures, words, or other symbols, direct selection or scanning strategy.
Three challenges that are faced: AAC is much slower than natural communication, AAC users are not all literate and must use vocab., and AAC must be constructed for variety of social settings.
Functional behavioral assessment: What triggers behavior?
Positive behavioral support: Positive reinforcement.
Self-stimulation: Swishing saliva, twirling objects, hand-flapping, fixed staring.
Self-injurious behavior: repeated physical self-abuse, biting, scratching, or poking oneself, head-banging. Unchecked results in self mutilation.
Tantrums: self-injury, screaming, crying, throwing or destroying objects and aggression towards others (Sometimes can come without warning).
Lack of daily living skills, yet these skills must be taught for progress to occur.
Neonatal intensive care units: around the clock monitoring of newborns with severe physical problems staffed by professionals from several disciplines.
Research or value-based practices: individualized practices for each child and family.
Family Centered practices: Emphasis on parents, siblings, and extended family to be apart of the educational progress of a child who is disabled.
Multicultural Perspective: Importance of communicating with family of all ethnic backgrounds.
Cross-Disciplinary Collaboration
Developmentally Appropriate Practice: same-age peer education.
Principle of Normalization: Inclusion.
Sheltered Workshop: structured environment for people with disabilities, can be transitional or permanent.
Community residential facility: group home in a residential neighborhood, three to ten adults live under one roof who are supervised by professionals.
Competitive employment: jobs that pay minimum wage, work alongside nondisabled workers, Ex: bagger at Publix.
Philosophy changers: self-determination, person-centered plan, natural supports, job coach, daily living skills, and of course, IEP.
Brain Injury Association of America www.biausa.org
National Association of State Head Injury Administrators http://www.nashia.org/
Neurology Channel www.neurologychannel.com
OPI Deaf and Blind Facts Sheet http://www.opi.state.mt.us/DBServices/Facts.html
American Association of the Deaf-Blind http://www.aadb.org/
Florida School for the Deaf and the Blind http://www.fsdb.k12.fl.us/
Helen Keller National Center For Deaf-Blind Youths and Adults http://www.hknc.org/
“About Brain Injury.” Brain Association of America. 2009. Caring Bridge. 2 June 2009. http://www.biausa.org/aboutbi.htm
“TBI Diagnosis.” Neurology Channel. March 2009. Healthcommunities.com. 2 June 2009. http://www.neurologychannel.com/tbi/diagnosis.shtml
McGregor, Gail. “Deaf-Blind Fact Sheet.” Montana State Project for Children and Youth with Deaf-Blindness. Sept. 2005. University of Montana. 3 June 2009. http://www.opi.state.mt.us/DBServices/Facts.html
Hallahan, Daniel P., Kauffman, James M., and Pullen, Paige C. Exceptional Learners: An
Introduction to Special Education. 11ed. Boston: Allyn & Bacon, 2009. 456-491.
Mo. “The Incredible Case of Phineas Gage.” Neurophilosophy. Dec. 2006.
Scienceblogs.com. 4 June 2009. http://neurophilosophy.wordpress.com/2006/12/04/theincredible-case-of-phineas-gage/
“Intervenor for Deaf-Blind Persons (Short Version).” Youtube. Oct. 2008. George Brown
College. 3 June 2009. http://www.youtube.com/watch?v=F8DiZbCu3TM&feature=related&pos=0
“Geoffrey’s Story.” Youtube. Feb. 2009. Ability Beyond Disability. 3 June 2009. http://www.youtube.com/watch?v=_938gpoBbvc
Lehr Jr., Robert P. “Brain Functions and Map.” TBI Resource Guide. 2009. Centre for Neuro
Skills. 5 June 2009.
Chudler, Eric C. “Simon Says & Face Memory Test 1&2.” Neuroscience for Kids. 2008.
University of Washington. 5 June 2009.