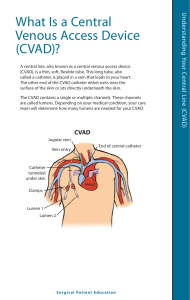
Week 5 Central Venous Access Device
advertisement
Your Mission…. Prevention and Early Detection!!!!! Quality Improvement Evidence-based practice Teamwork and Collaboration Safety “minimize risk of harm to patients and providers through both system effectiveness and individual performance” 1 Indications Long-term Caustic meds TPN (dextrose content > 10%) Monitor RA pressures Dialysis Multiple therapies No peripheral access Frequent blood sampling 2 What’s in a Name? Central Venous Access Device (CVAD) CVC Central line By type (percutaneous) TLC (triple lumen catheter), PICC By site subclavian, jugular, femoral By brand name (tunneled) Broviac, Hickman, Groshong, Mediport 3 What’s the Difference? Similarities Tip of catheter in a “central” vein: • Superior vena cava Differences How/where it is inserted Length of stay 4 Method 1: Percutaneous Needle stick, through skin, directly into vein. Central (7 days-Phillips) PICC (> 7 days to several months) Single, double, or triple lumen Triple: proximal, medial, distal ports 5 PICC line Peripherally Inserted Central Catheter 6 7 Tunneled Surgical procedure Very long-term Exit site: chest or abdominal wall Examples: Hickman Groshong Implanted port (medi-port) 8 CVAD Insertion Supplies : Check P&P tray antiseptic solution Dressing material CONSENT 10 cc Syringes w/ NS Needleless caps “time out” check list 9 Patient Teaching r/t insertion Purpose Position: flat, Trendelenberg keep hands down face covered turn head away 10 Complications of CVAD Pneumothorax Malposition SVC syndrome Occlusions Infection Air Embolism Unintentional disruption 11 Central Venous Catheter Complications — Pneumothorax, Hemothorax, Chylothorax Cause During insertion of CVC, introducer may cause trauma Pneumothorax (collection of air in the pleural space due to trauma to lung) Hemothorax (collection of blood in pleural cavity) Chylothorax (transection of the thoracic duct causes lymph fluid to enter the pleural cavity) 12 Central Venous Catheter Complications: Pneumothorax Treatment early detection: CXR after insertion Oxygen Monitor vital signs Pressure should be applied over the vein entry site Remove the catheter Chest tube if appropriate 13 Obstruction – Prevention is Key Positive Pressure Displacement device Flush unused ports per protocol ‘Push-Pause’ technique Check solution for precipitates Filter if indicated 14 Flushing a CVAD 10 mL syringe or larger Aspirate for blood return before flushing (INS,2006) SAS or SASH (per hospital protocol) Groshong Catheter – saline only “push – pause” technique Q 12 or 24 hours – per protocol Positive pressure caps flush, remove syringe, clamp 15 Infection CRBSI Exit site infection Catheter tract infection Septic thrombophlebitis 16 Central Venous Catheter Complications: Catheter Related Blood Stream Infection (CRBSI) Cause Bacteria or fungi in a patient who has a intravascular device with positive blood culture All BSIs that cannot reasonably be linked to a site of local infection are attributed to CVC Biofilm Contamination 17 Central Venous Catheter Complications: CRBSI (continued) Prevention (National Patient Safety Goals) Strict sterile technique Implementation of bundle approach Tunneling and subcutaneous cuffs Antiseptic-impregnated dressing Colonization-resistant polymers Contamination-resistant hubs Luminal antimicrobial flush/lock solutions Good hand hygiene Frequent site assessment 18 CR-BSI “bundle” Hand hygiene Maximum barrier precautions “time out” during insertion prn Chlorhexidine gluconate site disinfection Optimal catheter site (avoid femoral vein) Daily review of line necessity – remove when no longer medically indicated. 19 Systemic Complication: Venous Air Embolism (VAE) Cause Allowing the solution container to run dry and then hanging a new bag Loose connections that allow air to enter system Poor technique in dressing and tubing changes for central lines Presence of air in administration set Factors that must be present: direct communication with source of air Pressure gradient 20 Systemic Complication: Venous Air Embolism (VAE) Signs and symptoms Patient complains of palpitations Lightheadedness and weakness Pulmonary: dyspnea, cyanosis, tachypnea, expiratory wheezes, cough Cardiovascular findings: “mill wheel” murmur; weak, thready pulse; tachycardia; substernal chest pain, hypotension Neurologic findings: change in mental status, confusion, coma 21 Systemic Complication: Venous Air Embolism (VAE) (continued) Prevention Purge all air from administration sets Use 0.22 micron air-eliminating filter Follow protocol for dressing and tubing changes for central lines Attach piggyback meds to the proximal injection port Use Luer-Lok connectors Do not bypass the “pump housing” of EIDs After removal of central lines initial dressing should be occlusive 22 Systemic Complication: Venous Air Embolism (VAE) (continued) Treatment Call for help and notify physician immediately Once VAE is suspected, any central line procedure in progress should be stopped; clamp line Place in Trendelenburg position on left side Administer oxygen Maintain systemic arterial pressure with fluid resuscitation and vasopressors Monitor vital signs If circulatory collapse initiate CPR 23 CVAD Dressing Change Prevention of infection is dependent upon 1. 2. effectively reducing the number of microorganisms on the skin Limiting access of the microorganisms to the catheter site. 24 Discontinuing a CVAD Only for percutaneous Position: Trendelenburg Valsalva maneuver during removal Apply pressure Pressure dressing 25 Drawing blood from a central line (Dominican procedure) Turn off IV solutions Flush w/10 mL NS Withdraw 5 mL “discard” Use syringe or vacutainer to withdraw desired amt. blood Flush w/ 20 mL NS Label specimens “line draw” 26