PROCEDURE: CENTRAL VENOUS ACCESS DEVICE MANAGEMENT
PURPOSE:
The purpose of this procedure is to ensure the safety of patients during the insertion and ongoing
management of the Central Venous Access Device (CVAD) by implementing evidence-based clinical
practices to prevent complications.
DEFINITIONS:
1.
Central line/CVAD Bundle: The Institute for Healthcare Improvement (2012) describes the
central line bundle as “a group of evidence-based interventions for patients with intravascular
central catheters that, when implemented together, result in better outcomes than when
implemented individually. The science supporting each bundle component is sufficiently
established to be considered the standard of care”. For CVADs this includes hand hygiene,
maximal barrier precautions upon insertion, chlorhexidine skin antisepsis, optimal catheter site
selection with avoidance of femoral vein in adult patients, daily review of line necessity with
prompt removal of unnecessary lines.
2.
Central Venous Access Catheters (CVAD): are intravenous lines placed in a large central
vein for temporary or long-term IV therapy, including but not limited to: peripherally inserted
central catheters (PICCs), tunneled and non-tunneled catheters and pulmonary artery
catheters. The internal jugular and subclavian veins (except for dialysis/potential dialysis
patients) are the preferred insertion sites for non-tunneled catheters to minimize risk of
infection. CVADs are used for blood sampling, hemodynamic monitoring, and intravenous
administration of medications, blood products, and fluids.
3.
Hand hygiene-includes washing with soap and water or hospital approved waterless alcohol
gel. Hand hygiene is required before and after contact with all CVADs and prior to insertion.
4.
SCRUB the HUB: IV hub/injection port is to be scrubbed with alcohol wipe in a twisting motion
as if squeezing an orange for 15 seconds and allowed to air dry before accessing to prevent
central line associated blood stream infections.
AFFECTED DEPARTMENTS/SERVICES:
1.
2.
3.
A.
Nursing Units
Diagnostic Imaging Services
Medical Staff
PROCEDURE: COMPLIANCE – KEY ELEMENTS
1.
The central line bundle will be used for all insertions of CVADs except in life-threatening
emergencies
2.
All CVADs placed under non-sterile conditions in emergent situations shall be removed as
soon as possible,
3.
Chlorhexidine gluconate 2% in 70% isopropyl alcohol (ChloraPrep®) is the antiseptic standard
for central and peripheral CVAD insertion.
4.
Confirmation of proper placement (catheter tip in distal portion of the superior vena cava or the
SVC/atrial junction) by chest x-ray, fluoroscopy, or ultatrasound is required for all CVADs
before using the line (radiologic confirmation method appropriate for device type and insertion
site). 5. Unused ports shall be flushed, clamped (where a clamp is present on the CVAD), and
capped with alcohol port protectors (Swab Caps). Unused ports of IV tubing shall also be
capped with alcohol port protectors
Page 2 of 12
PROCEDURE: CENTRAL VENOUS ACCESS DEVICE MANAGEMENT
B.
6.
When accessing ports of the CVAD, the hub will be scrubbed with alcohol for 15 seconds and
allowed to air dry before access IF ALCOHOL PORT PROTECTOR CAPS (NOT IN PLACE
FOR > 3 MINUTES.
7.
Daily evaluation for continued need for the CVAD will be performed in collaboration with the
physician.
INSERTION OF CENTRAL LINES
1.
An assistant is required to be at the bedside during insertion of all centrally placed CVADs.
2.
The assistant will immediately notify the operator of any deviation from the critical steps, stop
the procedure if necessary, and assure compliance before procedure can proceed.
Sterile technique is required for CVAD insertions.
3.
4.
a.
Hand hygiene with hospital-approved soap and water or waterless alcohol-based
cleanser is required before CVAD insertion.
b.
A surgical scrub is required before insertion of tunneled catheters, implanted ports,
and permanent dialysis or hemapheresis catheters.
Except in acute, life threatening situations, the primary operator and any second operator shall
use maximal sterile barriers during CVAD insertion, regardless of where in the hospital the
procedure is performed, including:
a.
Cap (to be covered; scalp, beard, mustaches)
b.
Mask
c.
Sterile gown
d.
Sterile gloves
e.
Large sterile patient drape to cover patient from head to foot
5.
Eye protection (e.g., face shield).The assistant in the room will wear a cap, mask, gloves,
isolation gown, and face shield or eye protection. If at any point they are at risk to cross the
sterile field, the assistant should follow the same barrier precautions described above in #4
above.
6.
Chlorhexidine gluconate 2% in 70% isopropyl alcohol (Chloraprep) is the antiseptic of choice
for CVAD insertion and should be applied following manufacturer’s guidelines.
7.
a.
Allow antiseptic to fully dry (usually requires about 30 seconds).
b.
If the patient is intolerant to chlorhexadine, 1% tincture of iodine should be used
c.
Povidone iodine should not be used for CVAD skin prep unless the patient cannot
tolerate alcohol based products. If povidone iodine must be used, the skin should first
be de-fatted with soap and water, and then dried. The povidoneiodine must be
allowed to stay on the skin for a minute or more, to permit it to release the 1% iodine
required for sterility.
If equipment is available and provider is trained to use ultrasound guidance during line
placement, ultrasound guidance should be used for all non-emergent CVAD placements
Page 3 of 12
PROCEDURE: CENTRAL VENOUS ACCESS DEVICE MANAGEMENT
(optional for femoral line placement). When using ultrasound for line placement, sterile gel and
sterile probe and cord cover must be used.
8.
9.
During insertion or rewires, of a subclavian or internal jugular CVAD, the patient should be
placed in a 15-25 degree Trendelenburg position in order to prevent air embolism. If this
position is contraindicated by the patient’s condition (e.g., increased ICP), the physician
placing the line will make this determination for femoral CVADs, the patient should be supine.
Unused ports of multi-lumen CVADs shall be aspirated, flushed, capped, and clamped.
Confirmation of proper placement (catheter tip in distal portion of the superior vena cava or the
SVC/atrial junction) by chest x-ray, fluoroscopy, or ultrasound is required for all CVADs before
using the line (radiologic confirmation method appropriate for device type and insertion site).
All non-tunneled CVADs shall be sutured securely in place.
C.
FLUSHING HEPARIN/SALINE LOCKING CENTRAL LINES
Central lines should be flushed at regular and established intervals to maintain patency. Central lines
should be flushed before and after the administration of incompatible medications and/or solutions.
Scrub the hub of the injection cap with alcohol wipe for 15 seconds prior to accessing the port for
flushing
NSS = 0.9% sodium chloride solution
Heplock solution= 100 units/ml heparinized solution
Routine flush Frequency of Flush prior to
routine flush
med admin.
Flush
after
med or blood
draw
to
resume
infusion
Flush
after
med or blood
draw to lock
Discontinued
by
5 ml NSS
10 ml NSS
10 mL NSS
Nursing
MD order
with
5mL NSS
10 mL NSS
10 mL NSS
followed by 1
mL Heparin
lock solution
(100units/mL)
Nursing
MD order
with
3 ml NSS
5 ml NSS
MD only
Groshong
10 ml NSS
Weekly
catheters
should never
be clamped
(Smith, 2004)
Subcutaneous implanted ports
Implanted
5 ml Heplock
Monthly
port
soln
5 ml NSS
5 ml NSS
20ml NSS
followed by
3ml heplock
soln
10 ml NSS,
but should
never be
clamped
5 ml NSS
10 ml NSS
MD only
Groshong
implanted
10 ml NSS
10 ml NSS
20 ml NSS
followed by 5
ml heparin
20 ml NSS
Central Venous Catheter non-tunneled
Subclavian,
5 ml
Every 8 hours
jugular, or
NSS
femoral
catheter
PICC lines
1 ml Heparin Every 12
lock solution
hours
(100
units/mL)
Central Venous Catheter tunneled
Hickman and 3 ml heplock
Daily
Broviac
soln
catheters
10 ml NSS
Monthly
MD only
MD only
Page 4 of 12
PROCEDURE: CENTRAL VENOUS ACCESS DEVICE MANAGEMENT
Routine flush
Frequency of
routine flush
Flush prior to
med admin.
Flush
after
med or blood
draw
to
resume
infusion
Flush
after
med or blood
draw to lock
Discontinued
by
port
D.
FLUSHING HEPARIN/SALINE LOCKING CENTRAL LINES
EQUIPMENT LIST:
Non-sterile gloves
Heparin 100 units/ml solution or Normal saline solution
Syringes(See Flush Guide for size and number)
STEPS
1.
Verify patient identity and compare name band with source identification
2.
Explain procedure to patient.
E.
3.
Prepare workspace, gather supplies, and perform hand hygiene.
4.
Don non-sterile gloves.
5.
If alcohol protected ports swab caps are not in use, SCRUB the HUB of injection port cap with
alcohol wipe for 15 seconds. Allow to dry.
6.
Insert syringe containing recommended flush solution into middle of injection cap and flush.
See C. Central Line Flush Guide
7.
Remove syringe and discard in appropriate container.
8.
Document site, time, amount, and type of flush in medical record.
BLOOD SAMPLING
EQUIPMENTLIST:
Non-sterile gloves
Heparin 100 units/ml solution
Needleless injection cap & IV tubing cap
Alcohol swab
Syringes
Normal saline flush solution
STEPS
1.
Identify patient and compare name band with lab requisition. A Laboratory tech must be at
bedside and will bring requisition and syringes for sampling to bedside.
2.
Explain procedure to patient.
3.
Prepare workspace, gather supplies, and perform hand hygiene.
4.
Don non-sterile gloves.
Page 5 of 12
PROCEDURE: CENTRAL VENOUS ACCESS DEVICE MANAGEMENT
F.
5.
For sites with IV infusion, stop the IV solution and disconnect tubing from the catheter. Cap IV
tubing.
6.
If alcohol protected ports swab caps are not in use, SCRUB the HUB of the injection cap with an
alcohol wipe for 15 seconds. Allow to air dry before accessing.
7.
Insert 5 ml or 10 ml syringe containing recommended flush solution into injection cap and flush.
8.
Insert empty 5 or 10 ml syringe into middle of injection cap and withdraw 5- 10 mL of blood for
waste. Remove syringe and discard in appropriate container.
9.
Insert empty 5 or 10 ml syringe into middle of injection cap and withdraw sufficient amount for
blood sample. Hand syringe with sample to Lab tech.
10.
Replace injection cap with new cap primed with recommended flush solution.
11.
Insert 5 ml or 10 ml syringe containing recommended flush solution into injection cap and flush.
Discard syringe(s) in appropriate container.
12.
Reconnect IV tubing and restart infusion.
13.
Remove gloves. Perform hand hygiene.
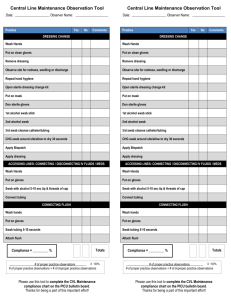
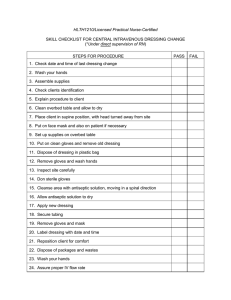
SITE CARE AND DRESSING APPLICATION
1.
Routine CVAD site care includes removal of the existing dressing, cleansing of the catheterskin junction with appropriate antiseptic solution, replacement of stabilization device if used,
and application of a sterile dressing.
2.
Transparent semipermeable (TSM) dressings with chlorhexidine-impregnated disc are to be
used on all CVADs unless the patient is diaphoretic or the site has oozing or bleeding in which
case a gauze dressing may be used.
3.
Site care and TSM dressing changes are to be routinely performed every 7 days, unless
the dressing integrity becomes compromised, if moisture, blood, or drainage is present, or if
signs and symptoms of infection are present.
4.
Gauze dressings should be changed every 2 days.
DRESSING CHANGE EQUIPMENT LIST:
Sterile gloves
2 Masks
Non-sterile gloves
Tape
Sterile 2x2s
Transparent dressing
Chlorhexidine swab (3 ml)(Chloraprep®)
Chlorhexidine-impregnated disc (Biopatch®)
STEPS
1.
Verify patient identity.
Page 6 of 12
PROCEDURE: CENTRAL VENOUS ACCESS DEVICE MANAGEMENT
G.
2.
Explain procedure to patient.
3.
Position patient. Place mask on patient unless intubated.
4.
Prepare workspace, gather supplies, and perform hand hygiene with soap and water or hospital
approved waterless alcohol-based gel.
5.
Don non-sterile gloves and mask.
6.
Remove and discard old dressing. Discard blood-tinged dressing (dried or saturated) in
biohazard container.
7.
Remove gloves. Perform hand hygiene.
8.
Don sterile gloves.
9.
Clean site with alcohol swab if needed. Apply chlorhexidine swab in scrubbing motion for 30
seconds to clean site. Allow to air dry for 30 seconds.
10.
Place BIOPATCH® around the catheter, making sure the PRINT side is facing upward.
a.
The WHITE foam side releases the Chlorhexidine Gluconate (CHG) and should be in
contact with the patient’s skin.
b.
In order to ensure easy removal when used with a film dressing, place BIOPATCH®
around the catheter/pin site in such a way that the catheter rests upon the slit portion
of the BIOPATCH®. The edges of the radial slit must be pushed together and remain
in contact to maximize efficacy.
11.
Apply adhesive side of transparent dressing to site. Take care to touch non-sticky side of
dressing only.
12.
Secure tape included in transparent dressing package over catheter hub. If necessary, tape
external catheter tubing to the skin, so tubing is secure and tension-free.
13.
Remove gloves. Perform hand hygiene.
14.
Label dressing with date, time and initials of clinician.
15.
Document dressing change and assessment of site in medical record.
ACCESSING IMPLANTED PORT
EQUIPMENT LIST:
Sterile gloves
Mask
Non-sterile gloves
Non-coring needle. Needle selection is based on needle length necessary to reach the back of
the port and the smallest gauge necessary to deliver prescribed therapy.
Sterile 2x2s
Tape
Chlorhexidine swab (3 ml)(Chloraprep®)
Transparent dressing
Heparin 100 units/ml solution
Page 7 of 12
PROCEDURE: CENTRAL VENOUS ACCESS DEVICE MANAGEMENT
Syringes See Central Line Flush Guide for size and number.
Chlorhexidine-impregnated disc (Biopatch®)
Normal saline flush solution
STEPS
1.
Explain procedure to patient.
2.
Position patient to expose implanted port. Place mask on patient unless intubated.
3.
Prepare workspace, gather supplies and perform hand hygiene.
4.
Don sterile gloves and mask.
5.
Clean site with alcohol swab if needed. Apply chlorhexidine 2% swab to clean site. Allow to dry.
6.
Apply needleless injection cap to non-coring needle extension and prime with normal saline.
7.
Anchor port with non-dominant hand. Locate port septum with between thumb and index
fingers. Move fingers to confirm septum location and to determine any septum movement.
8.
Extend fingers to stretch the skin over the port septum and to stabilize the reservoir.
9.
Hold non-coring needle between thumb and forefinger and perpendicular to the septum.
a.
H.
In one movement, firmly push the needle through the skin and septum until the needle
makes contact with the back of the reservoir. This action will require some force. The
septum will feel stiff. When the needle is in proper position, the nurse will feel metal
against metal. This contact must be felt to confirm proper placement of the needle
10.
Rotate the wing so that the extension points down or toward the sternum and not towards arm.
11.
Attach syringe and check for blood return.
12.
Insert syringe containing recommended flush solution into injection cap and flush. Discard
syringe(s) in appropriate container.
13.
14.
Place Biopatch® blue printed side up under non-coring needle wings.
Apply adhesive side of transparent dressing to site. Take care to touch non-sticky side of
dressing only. The needle should be changed every 7 days
15.
Remove gloves. Perform hand hygiene.
16.
Label dressing with date and time changed.
17.
Document in MEDICAL RECORD.
REMOVING A CVAD
SUPPORTIVE DATA: A non-tunneled, non-implanted catheter may be discontinued by an RN upon
the order of a licensed provider.
EQUIPMENT LIST:
Non-sterile gloves
Suture removal kit
Page 8 of 12
PROCEDURE: CENTRAL VENOUS ACCESS DEVICE MANAGEMENT
Sterile gloves
Transparent dressing
Sterile 4X4s
Tape
Chlorhexidine 2% swab (3 ml)
Mask
STEPS
1.
Verify patient identity.
2.
Explain procedure to patient.
3.
Position patient in supine position, HOB flat. Turn patient’s heads away from the insertion
site.
4.
Turn off IV pump.
5.
Prepare workspace, gather supplies, and perform hand hygiene.
6.
Don non-sterile gloves and mask and remove old dressing.
7.
Discard dressing.
8.
Remove gloves and perform hand hygiene.
9.
Don sterile gloves.
10.
Clean site with alcohol swab if needed. Apply chlorhexidine 2% swab to clean site. Allow to dry.
11.
Remove sutures. Hold a 4X4 gauze pad over the insertion site without pressure. Have patient
hold breath. Grasp catheter and withdraw in a continuous motion, rotating the catheter slightly
during removal. Have the patient resume normal breathing once the catheter is out. If
resistance is met while withdrawing catheter, stop removal, apply sterile dressing and contact
physician.
12.
Immediately following catheter removal, apply a 4X4 gauze pad to the exit site and hold
direct pressure for 5 minutes or until hemostasis is achieved.
Apply new sterile 2X2 gauze covered by a transparent dressing. Label dressing with date/ time
and clinician’s initials.
13.
I.
14.
Inspect catheter for integrity.
15.
Discard catheter and all other supplies appropriately.
16.
Remove gloves. Perform hand hygiene.
17.
Document in MEDICAL RECORD.
ASSESSMENT:
1.
Assessment of the patient is ongoing and requires nursing judgment, interpretation and
synthesis of data, focused observation, and critical thinking. The nurse must be aware of the
potential complications of central line therapy, and assess patient for signs and symptoms of
those complications.
Page 9 of 12
PROCEDURE: CENTRAL VENOUS ACCESS DEVICE MANAGEMENT
a.
Site: Assessment of the catheter site and dressing must be done daily. The
catheter-skin junction site should be visually inspected or palpated daily for
tenderness through the intact dressing.
b.
Equipment/Solution:
Observe for:
1)
2)
3)
4)
J.
Correct settings: flow rate, and volume settings
Correct solution and additives
Secure tubing connections
Unused device/tubing hubs capped with alcohol port protector caps (swab
caps)
REPORTABLE CONDITIONS:
1.
Report signs and symptoms of complications to the physician.
a.
Air Embolus:
1)
2)
b.
2)
c.
All sites should be routinely assessed for signs and symptoms of infiltration
using the Infiltration Scale.
Phlebitis:
1)
e.
Observe for:
a)
Thrombotic catheter occlusion-Consider thrombus caused by
coagulated blood or fibrin products.
b)
Non-thrombotic catheter occlusion: occlusion caused by patient’s
position or lipid residue or drug/mineral precipitate
c)
Catheter migration: Inability to aspirate or flush; Pain and swelling in
clavicle area, shoulder, chest, neck, face.
If unable to flush, do not force. Label lumen “clotted”.
Infiltration:
1)
d.
Observe for: tachycardia, dyspnea, hypotension, pallor, cyanosis, syncope,
chest pain, anxiety, sudden fear, confusion.
If air embolus is suspected, immediately apply oxygen and place in left
Trendelenberg to minimize embolus migration.In the presence of a damaged
external line, clamp the catheter as close to the chest wall as possible.
Catheter Occlusion:
1)
All sites should be routinely assessed for signs and symptoms of phlebitis
using the Phlebitis Scale.
Septicemia:
1)
K.
Assess the infusion devices, systems, every 12 hours.
Observe for chills, backache, fever, hypotension, headache, increased white
count. Evaluate for other sources of infection, such as UTI, wound,
respiratory.
INFECTION CONTROL AND SAFETY:
Page 10 of 12
PROCEDURE: CENTRAL VENOUS ACCESS DEVICE MANAGEMENT
1.
Wash hands before and after all clinical procedures, and before and after donning gloves.
Keep catheter site covered with transparent or gauze dressing. Use 2% chlorhexidine for site
disinfection unless patient allergic. Apply according to manufacturer’s recommendations. Use
closed stopcock and piggyback connections, which provide for secure, aseptic connections.
Keep all unused ports clamped/closed at all times.
2.
Maintain aseptic technique (using methods to minimize contamination or introduction of
pathogens) for all infusion-related procedures. Follow Standard Precautions, Exposure
Control Plan {including use of Personal Protective Equipment (PPE)}, Infectious Waste, and
Sharps/Needle Disposal policies when performing infusion related care.
3.
4.
Alcohol Port Protector (Swab caps)
a.
All needleless connector ports with CVAD (including PICC lines) access will be
protected by swab caps
b.
The swab caps is single use only. Discard any removed swab cap and replace with
new cap.
c.
New swab cap(s) will be applied to each port with each 96-hour tubing change and
with each 96-hour needleless connector valve changes. Applied swab caps musts be
exchanged at least every 7 days.
d.
If swab caps cap has been in use for 3 minutes or longer, no additional disinfection
(“scrub the hub" is required before port access.
e.
If an IV port is immediately needed for access and the swab cap has not been in place
for 3 minutes, remove the cap, “scrub the hub” per policy before accessing the IV port.
Once the port access is completed, apply swab cap.
f.
Correct use of swab cap
1)
2)
3)
4)
5)
6)
L.
Prior to applying cap, wipe away any visible blood or soil with alcohol swab.
Peel foil tab from cap
Push and twist cap onto the end of needleless connector and IV tubing ports
until secure.
Apply to all ports of entry on every CVAD (including PICC line).
When ready to access line, simply remove cap and discard. Maintain sterility
with port and access with aseptic technique.
Apply new cap when completed.
g.
Educate patient/Significant other on placement and purpose of alcohol port protector.
Instruct to leave in place.
h.
Document teaching and any interventions appropriately in the medical record.
PATIENT/SIGNIFICANT OTHER (SO) INSTRUCTION:
1.
Instruction should be individualized to patient. All aspects of therapy, including risks and
benefits should be explained. Patients should be cautioned not to tamper with the infusion
pump and not to pull or unclamp tubing. Patients should be instructed to report the following to
the RN:
a.
Tension or disconnection of tubing
b.
Pain at insertion site
Page 11 of 12
PROCEDURE: CENTRAL VENOUS ACCESS DEVICE MANAGEMENT
M.
N.
c.
Wet, loose or bloody dressing
d.
Pump alarms
e.
Swelling of neck/face, shortness of breath, pain in shoulder, arm, or chest.
DOCUMENTATION IN MEDICAL RECORD:
1.
Record assessment data in the nursing assessment form
2.
Record implementation of Central Line Bundle during insertion.
3.
Record patient/SO education.
4.
Record removal procedure including indication.
5.
Record provider communication of reportable conditions.
REPLACEMENT OF CVADs, INCLUDING PICCS AND HEMODIALYSIS CATHETERS:
1.
Do not routinely replace CVADs, PICCS, hemodialysis catheters, or pulmonary artery
catheters to prevent catheter-related infections.
2.
Do not remove CVADs or PICCs on the basis of fever alone. Use clinical judgment regarding
the appropriateness of removing the catheter if infection is evidenced elsewhere or if a noninfectious cause of fever is suspected.
3.
Do not use guidewire exchanges routinely for non-tunneled catheters to prevent infection.
4.
Do not use guidewire exchanges to replace a non-tunneled catheter suspected of infection.
5.
Use a guidewire exchange to replace a malfunctioning non-tunneled catheter if no evidence of
infection is present.
6.
Use new sterile gloves before handling the new catheter when guidewire exchanges are
performed.
CENTRAL LINE IV MANAGEMENT
CENTRAL IV CARE
Insertion
Frequency
Follow strict sterile technique
Assessment
Frequently throughout shift; Visually, or palpate
via transparent dressing, remove dressing if
tender or infection is suspected
Occlusive transparent dressing – WEEKLY and
PRN soiling, damp loosening
Gauze – use if diaphoretic or site bleeding or
oozing – change every 2 days
See section B above
Dressing changes
Flushing of catheter
Comments
Label the insertion site
dressing
with
insertion
date/time
Assess continued need daily
with physician
Label the dressing
dressing change dates
Tubing Changes
Frequency
Comment
All IV tubing must be labeled with change day sticker and date/time of next tubing change
with
Page 12 of 12
PROCEDURE: CENTRAL VENOUS ACCESS DEVICE MANAGEMENT
Primary and secondary tubing,
including stopcocks and extension
tubing
Intermittent tubing
Every 96 hours
TPN, procalamine, solution
concentrations greater than D10
and lipids, PCA syringe
Blood/blood component
Every 24 hours
Hemodynamic/ arterial pressure
monitoring
HANG TIME OF FLUIDS
Maintenance IV Solution
Every 96 hours (includes flush fluid)
Medicated solution
TPN
24 hours if mixed in unit; as specified on label if
prepared by Pharmacy
Within 24 hours
Lipid emulsions
Every 12-24 hours
Blood/blood products
Hang within 20-30 minutes after receiving from
Blood Bank, transfuse within 4 hours
Frequency depends on type
of solution running
Every 24 hours
Propofol infusion tubing to be
changed every 12 hours.
After second unit of blood or at the end of 4
hours whichever comes first
Frequency
Every 24 hours
Comment
Label with date/time hung
Propofol change every 12
hours
REFERENCE LIST:
1. American Association of Critical Care Nurses. (2005). AACN Procedure Manual for Critical Care. (5th ed.). Saunders Elsevier:
Philadelphia:PA.
2. Bard Access Systems, Inc. (2013). Poly-Rad PICC catheters instructions for use. Retrieved from:
http://www.bardaccess.com/assets/pdfs/ifus/0714229-3153155-Poly_RADPICC_IFU-web.pdf
3. Centers for Disease Control. (2011). Guidelines for the prevention of intravascular catheter-related infections. Retrieved from:
http://www.cdc.gov/hicpac/BSI/BSI-guidelines-2011.html
4. Infusion Nurses Society. Infusion Nursing Standards of Practice (2011). J Infusion Nurs. Supplement 34 (1S). pp. S1-S110.
5.
Institute for Healthcare Improvement. (2012). How-to Guide: Prevent Central Line-Associated Bloodstream Infections (CLABSI).
Retrieved from: http://www.ihi.org/knowledge/Pages/Tools/HowtoGuidePreventCentralLineAssociatedBloodstreamInfection.aspx
6. Ivera Medical Corporation. (2012). Policy and clinical practice guidelines: Curos alcohol port protector. Retrieved from
http://www.curos.com.
7. Johnson & Johnson, Ethicon, Inc. (2008). Biopatch protective disk with CHG (package insert). Retrieved from:
http://www.ethicon360.com/ifu