Nursing Care of Patients with Central Venous Access Devices
advertisement

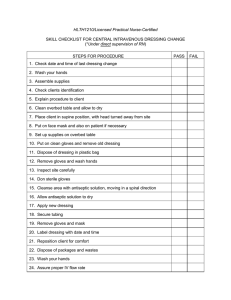
University of Kentucky / UK HealthCare Nursing Policy and Procedure Policy # NI08-16 Title/Description: Nursing Care of Adult Patients with Central Vascular Access Devices Purpose: To provide guidelines for nursing staff who care for patients with a central vascular access device. Policy Definitions Central Vascular Access Device (CVAD) Procedures Placement of a Central Vascular Access Device Central Vascular Access Device Insertion Bundle Components Confirmation of CVAD Placement Documentation of CVAD Daily Care of Patient with CVAD CVAD Dressing Changes Tubing / End Cap Changes Transducer Set-Up and Zeroing Scrubbing the Hub Removal of CVAD References Persons and Sites Affected Policies Replaced Effective Date Review/Revision Dates Appendix 1 Policy Nursing staff shall follow this policy when: 1. Assisting with the insertion of central vascular access devices; 2. Caring for adult patients with central vascular access devices; and 3. Removal of central vascular access devices. This policy is used in conjunction with NI08-03, Administration of IV Therapy to Adult and Pediatric Patients. This policy excludes any dual lumen catheter used for hemodialysis. For hemodialysis catheters, please refer to NE08-02 – Nursing Management of Patients with Dual Lumen Vascular Catheters Placed for Hemodialysis. Policy # NI08-16 Nursing Care of Adult Patients with Central Vascular Access Devices 1 Definitions Central Vascular Access Device (CVAD) A device that permits access to the central vascular system. A catheter is inserted with the tip residing in the lower one-third of the superior vena cava, or above the level of the diaphragm in the inferior vena cava. Procedures Placement of a Central Vascular Access Device 1. Equipment: (a) Central Vascular Access Device Kit; (b) Sterile gloves, sterile gown, mask, and cap: referred to as WildCat Bundle; (c) Sterile dressings (either gauze and tape or transparent semipermeable membrane (TSM) dressing); (d) Chlorhexidine (CHG) (e.g., Chloraprep ®) is used to prep the site for insertion; Note: If hypersensitivity to CHG exists, the site is scrubbed with povidone-iodine using 3 applicators in an outward circular motion away from the site. Allow to dry for 2 minutes. If hypersensitive to povidone-iodine, scrub the site with 70% alcohol only, using 3 applicators in an outward circular motion away from the site. Allow to dry for 2 minutes. (e) Large sterile full body drape to cover the entire patient, exposing only the area intended for placement. 2. Nursing Role: (a) The registered nurse (RN) assigned to the patient shall either be present or shall designate another nurse to ensure Bundle Component Compliance and Time Out documentation. Time Out documentation shall be completed as specified in A08-015 Universal Protocol. (b) The RN shall assist the physician or licensed independent professional (LIP) with patient positioning, prepping equipment, and other activities as requested and appropriate. RN shall document procedure in EMR. Central Vascular Access Device Insertion Bundle Components Best practice components outlined by the Centers for Disease Control (CDC) are: 1. Wash Hands before entering room and prior to donning sterile gown and gloves. 2. Use Chlorhexidine (2%chlorhexidine skin preparation with alcohol for skin antisepsis) as the solution of choice to prep the site. If there is a contraindication to chlorhexidine, Policy # NI08-16 Nursing Care of Adult Patients with Central Vascular Access Devices 2 tincture of iodine, iodophor, or 70% alcohol can be used as alternatives. See above for procedure. 3. Use a Maximum Sterile Barrier. A full body drape must be used to cover the patient, only exposing the area intended for CVAD placement. The clinician who is placing the CVAD must wear a hat, mask, sterile gown and gloves. Anyone directly assisting the clinician with placement must wear the same protective gear. Anyone else in the room must wear a hat and mask during the procedure. 4. Use the subclavian or internal jugular. For the adult population, femoral site should only be utilized if: The line placement is in an emergent situation or if there are medical contraindications to placement in the subclavian or internal jugular. 5. Remove the CVAD as soon as it becomes unnecessary and use peripheral access. Confirmation of CVAD Placement Once the CVAD has been placed and prior to use, the RN shall verify there is an order that states that the catheter is “okay to use.” Documentation of CVAD At the time of insertion or upon admission of patient with CVAD, the RN shall add CVAD parameter in the IV access/lines section of the flow sheet. At a minimum of once per shift, the RN shall add document: 1. Catheter Type 2. Insertion site (Location) 3. Site Assessment 4. Line Patency/Placement 5. Catheter Length Exposed from Insertion Site 6. Line Site Day 7. Interventions 8. Assessment of Dressing 9. Line Necessity Review: If the lines are deemed no longer necessary, staff shall request an order for removal of the line. Daily Care of Patient with CVAD All clinical staff are required to wash hands and apply clean gloves immediately before touching any part of the infusion system (CVAD, tubing, dressing, etc.). 1. The RN shall monitor the catheter sites visually or by palpation through an intact dressing every shift and shall document findings in the nursing flow sheet. 2. The catheter sites shall be assessed visually when changing the dressing. 3. If the patient has tenderness at the insertion site, fever without obvious source, neutropenia, or other manifestation suggesting local or bloodstream infection, the dressing Policy # NI08-16 Nursing Care of Adult Patients with Central Vascular Access Devices 3 shall be removed to allow for a thorough examination of the site. Nursing staff shall notify the physician immediately if a blood stream infection is suspected. 4. Daily skin cleansing using a 4% Chlorhexidine (Hibiclens®) wash shall be conducted daily for adult patients with CVAD. If there is a contraindication to chlorhexidine, tincture of iodine, iodophor, or 70% alcohol can be used as alternatives. CVAD Dressing Changes Adult Services: All dressing changes occur every Wednesday even if the dressing has been recently changed, on a previous day during the week. If patients are admitted with a port-a-cath accessed from an outside facility, change Huber needle within 12 hours of admission, and then every Wednesday. Children and Neonatal Services: Dressing changes occur weekly and whenever they become soiled or loose. The day of the week for central line dressing changes and weekly port-a-cath access mirrors the family’s home routine, in order to provide continuity of care and minimize traumatic events in hospitalized children. 1. Routine dressing changes shall be completed: (a) Within 12 hours of admission (b) Every Wednesday regardless of last dressing change. (c) Hemodialysis (HD) day by HD RN if currently on therapy. If not on HD therapy, unit RN should change per Wednesday schedule. (d) As needed, if the dressing becomes loose, damp, soiled, or previous dressing not done per policy. 2. The RN shall collect supplies prior to dressing change. (a) Central Line Dressing change kit (b) Second Chloraprep® may be necessary (c) Anti-microbial disc (e.g. Biopatch ®) (d) TSM dressing (e.g. Tegaderm®) (e) Mask for everyone in room including patient (f) If non-sutured CVAD, a catheter securement device (Stat-Lock®). (g) Clean non-sterile gloves 3. Don mask and place a mask on the patient. Everyone in the room must wear a mask during dressing changes. 4. The RN shall perform hand hygiene and don clean (non-sterile) gloves. (a) Remove old dressing. Pull old dressing toward the insertion site to avoid dislodging the catheter. (b) Remove old CVAD securement device (Stat-Lock®). (c) Observe insertion site for erythema, exudates and catheter migration. Policy # NI08-16 Nursing Care of Adult Patients with Central Vascular Access Devices 4 5. Remove clean (non-sterile) gloves and perform hand hygiene. (a) Using aseptic technique, the nurse shall: (i) Carefully unfold sterile drape and lay on a clean, dry working surface as a sterile field. The contents from the dressing change kit or appropriate supplies gathered shall be placed on the sterile field. (ii) Don sterile gloves (iii)Disinfect catheter-skin junction site using a friction scrub with 2% Chlorhexidine gluconate prep (Chloraprep®). (If Chlorhexidine is contraindicated, see below for instructions.) (iv) Scrub the site with Chloraprep® by using a back and forth motion for at least 30 seconds. The site includes the skin beyond the parameter, of the intended dressing area. Allow to completely air dry. • A second Chloraprep® may be necessary to remove all dried blood or exudate. • Do not blot, fan, blow, or wipe the site as it dries. • If Chlorhexidine is contraindicated, second choice is to apply povidoneiodine: Apply in a circular motion starting from the CVAD insertion site and working outward. Take care not to return to already cleaned area with a used applicator. Repeat at least 2 times. Do not blot, fan, blow, or wipe the site as it dries. Allow to completely dry for a minimum of 2 minutes. (v) Third choice if sensitive to Chloraprep and povidone-iodine, use 70% alcohol. • Apply in a circular motion starting from the CVAD insertion site and working outward. Take care not to return to already cleaned area with a used applicator. Repeat at least 2 times. • Do not blot, fan, blow, or wipe the site as it dries. • Allow to completely dry. 6. Apply antimicrobial disc (e.g., Biopatch®) to insertion site – blue side up making sure to allow for easy removal of patch with next dressing removal (i.e. slit rotated slightly past catheter). Must be placed circumferential around the insertion site for product effectiveness. Do NOT apply ointment or cream to the insertion site. 7. Apply securement device (Stat-Lock®) to the external hub of CVAD and lock into place. Then secure device to skin. 8. Apply transparent dressing (Tegaderm®) over site – form an occlusive seal by pinching the adhesive portion of dressing against the external catheter lumen. Do not allow the dressing to “tent” where the lumen exits the dressing. (a) If the site is bleeding or seeping, utilize the gauze and tape dressing until drainage is maintained. If using gauze and tape, must be changed every 48 hour or when wet, soiled, or no longer intact. Do not place Tegaderm over gauze, must use tape. Policy # NI08-16 Nursing Care of Adult Patients with Central Vascular Access Devices 5 (b) If the catheter has migrated in or out > 3 cm, notify the LIP or Vascular Access Nurse if PICC, for confirmation of the location of the tip of the catheter. If migration and no blood return, discontinue use and notify LIP immediately. 9. Remove gloves and perform hand hygiene. 10. Label the dressing with the date, time, and RN’s initials. 11. Document the dressing change in SCM. Tubing / End Cap Changes 1. Tubing changes must occur every 96 hours (as long as continually connected) per NI0803. Tubing must be labeled with expiration date, time and initial of RN. 2. End cap changes must occur, with every tubing change, if residual blood noted, and upon admission from outside facility. Replace end caps every seven (7) days when the line is not in use. Scrub hub treads with a new antiseptic swab and allow it to dry completely, before connecting a new cap. Cap change is a sterile procedure with everyone in the room wearing a mask. 3. If intermittent infusion or disconnected for any reason, tubing change is every 24 hours. 4. Tubing should be disconnected at a minimum and ends of tubing should always be kept sterile. If disconnecting tubing for any length of time, end of tubing must be capped with sterile cap. Alcohol packages are NOT acceptable substitutes for sterile caps. 5. When new CVAD is placed, ALL tubing and medications must be changed to new sets. Do not utilize existing tubing from any preexisting site, including peripheral sites. 6. All IV tubing (primary and secondary) must be labeled with the following: (a) Start date/time (b) Discard date/time (c) Initials Transducer Set-Up and Zeroing 1. Perform hand hygiene and don clean non-sterile gloves prior to touching any part of the transducer set. 2. Follow process outlined in Mosby’s. 3. When zeroing a transducer, the end cap can be loosened but not removed . If removed, a new sterile endcap is required. Scrubbing the Hub 1. Performing hand hygiene and don clean gloves. 2. Scrub vigorously in a twisting motion with Chloraprep® or 70% alcohol for 15 seconds prior accessing. Let dry for 15 seconds before accessing the hub. Removal of CVAD It is imperative to follow CVAD removal procedures carefully in order to prevent air embolisms that can lead to patient death. A Time-Out is required for removal of central lines that have been Policy # NI08-16 Nursing Care of Adult Patients with Central Vascular Access Devices 6 placed in the chest, regardless of whether the RN or MD is performing the procedure. A time out is not required for removal of Peripherally Inserted Central Catheters (PICC) lines. To document the time out, enter new document, time out note in documents section. Click on 'other' under procedure being performed, and free text 'central line removal'. For critical care/progressive care areas where the RN is removing the central lines, the time out is conducted RN to RN or RN to MD. The time out consists of: 1. Correct patient and central line removed 2. Patient positioning 3. Drips and medications accounted for and dressings ready For acute care areas where RNs do not remove central lines, coordinating the timeout is the responsibility of the MD and can be conducted MD to RN. The level of responsibility for the RN in acute care is to be aware that a time out is required and to know that the patient needs to be in the supine position, or slight Trendelenburg position if able. Central lines are not to be removed while the patient is upright or sitting. Prior to removal of a CVAD the RN must: 1. RN must have demonstrated competency in the form of three supervised successful completions of the Central Venous Catheter Removal checklist on Mosby’s prior to removal of any CVAD not a PICC. For PICC lines, see nursing guideline NG-050. 2. Verify the LIP order for removal. 3. Know the patient’s coagulation status (INR/PTT) and communicate any concerns to the LIP. If coagulation status suggests the patient is at risk of bleeding, but line must be removed, RN must be prepared to hold manual pressure on site. 4. Line must be pulled while patient is recumbent in bed. Patient cannot be in a chair. RNs in the following care areas may pull CVADs in the following anatomical areas after demonstrated competency: 1. RNs in critical care may remove a non-tunneled CVAD from the femoral, internal jugular, subclavian veins, or PICCs. 2. RNs in progressive care may remove a non-tunneled CVAD from the internal jugular, subclavian veins, or PICCs. 3. RNs in acute care may remove PICC lines. To remove the CVAD, the following steps are performed: 1. Gather sterile petroleum based dressing, sterile gauze, tegaderm, sterile and non-sterile gloves, and suture kit if necessary. Discontinue administration of all infusates. 2. Place the patient supine and in slight Trendelenburg if he or she is able to tolerate. The patient shall not be sitting or standing. 3. Perform hand hygiene and apply non-sterile gloves. Remove old dressing and stabilization device. Policy # NI08-16 Nursing Care of Adult Patients with Central Vascular Access Devices 7 4. Perform hand hygiene. Open sterile petroleum gauze dressing, sterile gauze, and sterile gloves. Perform hand hygiene and apply sterile gloves. 5. Instruct the patient to hold his or her breath and perform the Valsalva maneuver (forced expiration with the mouth closed) when the catheter is being removed at a gentle even pressure. If the patient is unable to cooperate with instructions, the catheter should be removed following inspiration. 6. Cover the insertion site immediately with sterile Vaseline gauze covered with a folded sterile gauze, maintain firm manual pressure until hemostasis is achieved. Then cover the site with an air-occlusive dressing, which remains in place for 24-72 hours. 7. Assess integrity of removed catheter. Compare length of catheter to the original insertion length to ensure entire catheter is removed. 8. Document procedure in patient’s permanent medical record. (a) Catheter make (i.e. Solo dual lumen PICC) (b) Entire length of catheter in cm (i.e. 46cm) (c) Integrity of catheter tip (should be an evenly cut tip) (d) Site assessment (e) Patient tolerance of the procedure 9. Change dressing every 24 hours or until exit site healed. Cleanse daily and redress as needed. After removal of the CVAD: 1. Hemostasis must have occurred prior to the RN leaving the patient’s bedside. 2. Patient must remain on bed rest in a recumbent position for at least 30 minutes. References 1. Infusion Nurses Society. (2011) Infusion Nursing Standards of Practice. Journal of Infusion Nursing, 34(1S). 2. Centers for Disease Control (2011) Guidelines for the prevention of intravascular catheter-related infections. O’Grady, N., Alexander, M., Burns, L., Dellinger, E.P., Garland, J., Heard, S.O., Lipsett, P.A., Masur, H., Mermel, L.A., Pearson, M., Raad, I., Randolph, A., Rupp, M., Saint, S., & HICPAC. 3. Camp-Sorrell, D. (Ed.). (2011). Access device guidelines: Recommendations for nursing practice and education. Pittsburg, PA: ONS Publishing Division. 4. Maintenance Related Interventions Successfully Reduce Central Line Associated Bloodstream Infections. (2012) Parada, Jorge, et.al. American Journal of Infection Control (41) S113-114. 5. Seven Years, Zero CLABSI: How a California Hospital Did It. (May/June 2013) Reader, Alan. 6. VUMC Standards for Non-emergent Insertion and Management of Central Venous Catheters. Vanderbilt University Medical Center, Infection Prevention Department. Policy # NI08-16 Nursing Care of Adult Patients with Central Vascular Access Devices 8 Persons and Sites Affected Enterprise Chandler Good Samaritan Kentucky Children’s Ambulatory Department Policies Replaced Chandler HP Ambulatory KC Good Samaritan Kentucky Children’s CH Other NI08-09, NI08-10, NI08-25 Effective Date: 01/19/2015 Review/Revision Dates: 8/2011, 10/08/2014; 01/19/2015 Approval by and date: Signature Date _______________ Name Glenda Kay Roberts, Enterprise Infection Preventionist, Review Team Leader Signature Name Richard Zerbee, Chair, Nursing Professional Practice Council Date _______________ Signature Date _______________ Name Robyn Cheung, Director, Nursing Professional Practice and Innovation Signature Name Colleen Swartz, Chief Nurse Executive Date Policy # NI08-16 Nursing Care of Adult Patients with Central Vascular Access Devices 9 Appendix 1: Device Tunneled Peripheral Percutaneous Implanted Type Hickman, Broviac, PowerLine, Groshong PICC Triple lumen, MAC Introducer, Udall Port-A-Cath RN May Remove NO Yes Yes NO Describe Dacron cuff at exit site which eventually adheres to tissue to hold catheter in place and provides a barrier against infection Placed usually in upper extremities. Dwell time weeks to months. Line held in place by sutures. Dwell time recommended up to 14 days. Usually triple lumen. Hubs are color-coded (distalmedial-proximal). Also includes non-tunneled dialysis catheter. Surgically implanted in upper chest, can be arm or abdomen. Access with non-coring Huber needle. Can be single or double lumen. Picture Hubs are color-coded (distal-medial-proximal) Dwell time months. Dressing Change Sterile Procedure: Use mask (RN, patient, and anyone in room), sterile gloves. Ask visitors to leave the room or wear a mask. 1. If line present on admission change dressing within 12 hours 2. Routine dressing changes should occur every 7 days on Wednesday and if loose or wet prn. 3. Use dressing change kit, clean with CHG prep, allow to dry completely for about 30 seconds. 4. Place correct sized antimicrobial disk blue side up and circumferential around the line. If percutaneous line is sutured too tight, ask provider to re-suture. 5. Place correct bordered Tegaderm over antimicrobial disk Assess the site for signs and symptoms of infection. Policy # NI08-16 Nursing Care of Adult Patients with Central Vascular Access Devices 10 Appendix 1: End Cap Change Flushing Drawing Blood Other This is a sterile procedure, with everyone in the room wearing masks. If patient admitted with line, change caps on admission. After removing old cap, scrub the hub treads with antiseptic wipe for 15 seconds and allow to dry completely before attaching new sterile cap. Routinely change prior to drawing blood cultures, with each tubing change and if residual blood is noted in the cap, Prior to accessing end cap or port on tubing, wash hands for 15 seconds, apply clean gloves then SCRUB THE HUB FOR 15 SECOND VIGOROUSLY BACK AND FORTH. ALLOW TO AIR DRY BEFORE ACCESSING, All ports must have endcaps in place. • Must know if open or closed. See below. • Wash hands and apply clean gloves • SCRUB the HUB for 15 seconds and allow to dry before accessing. • Use pulsatile flush technique • Flush with 10mL of normal saline before and after every dose of medication. • Flush with 10mL of normal saline every 12 hours if intermittently used. • Flush with 20mL of normal saline after blood draws and if any blood seen in tubing. • For open lines (see below) when lumen not in use: Flush with 10mL of normal saline, followed by 5mL (100u/mL) of heparin. • Stop IV fluids if infusing. • Wash hands and don clean gloves. • Use proximal lumen for blood specimen. • Scrub end cap with alcohol for 15 seconds, allow to dry. • Flush with 10mL of normal saline. • Aspirate back slowly with 10mL syringe • Draw 5mL and waste • Draw specimen • Flush with 20mL normal saline using pulsatile pulse, followed by heparin if indicated. • Change endcap if blood noted after flush. Power-Injectable: Usually denoted by a purple hub/line. Absolutely necessary if giving power injected contrast. If not power injectable, must start PIV. Open vs Closed: An “open” CVAD means no internal valve, so a clamp is required to close the system. Heparin flushing is also required to lock the system on these open systems. Closed means there is a valve and therefore no clamps will be present on the line and heparin is not required. If unsure, lock with heparin. Groshongs are closed (valved lines). Policy # NI08-16 Nursing Care of Adult Patients with Central Vascular Access Devices 11