Ch. 13 Notes - Plainview Schools
advertisement

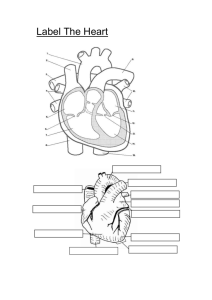
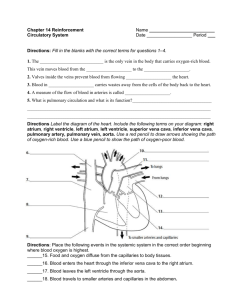
Cardiovascular System Chapter 13 Heart Anatomy • Approximately the size of your fist • Location: – Superior surface of the diaphragm – Left of the midline – Anterior to the vertebral column, posterior to the sternum Coverings of the Heart: Anatomy • Pericardium – a double-walled sac around the heart composed of: – Superficial fibrous pericardium – Deep two-layer serous pericardium • Parietal layer lines the internal surface of the fibrous pericardium • Visceral layer or epicardium lines the surface of the heart • They are separated by the fluid-filled pericardial cavity Coverings of the Heart: Physiology • The pericardium: – Protects & anchors the heart – Prevents overfilling of the heart with blood – Allows for the heart to work in a relatively frictionfree environment Heart Wall • Epicardium – visceral layer of the serous pericardium • Myocardium – cardiac muscle layer forming the bulk of the heart • Endocardium – endothelial layer of the inner myocardial surface External Heart: Major Vessels of the Heart • Vessels returning blood to the heart: – Superior & inferior venae cavae – Right & left pulmonary veins • Vessels conveying blood away from the heart: – Pulmonary trunk, splits into right & left pulmonary arteries – Ascending aorta (three branches) – brachiocephalic, left common carotid, & subclavian arteries External Heart: Vessels that Supply/Drain the Heart • Arteries: – Right & left coronary (in the atrioventricular groove), marginal, circumflex, and anterior interventricular • Veins: – Small cardiac, anterior cardiac, and great cardiac Atria of the Heart • • • • Atria are the receiving chambers of the heart Each atrium has a protruding auricle Pectinate muscles mark atrial walls Blood enters right atrium from superior and inferior venae cavae and coronary sinus • Blood enters left atrium from pulmonary veins Ventricles of the Heart • Ventricles are the discharging chambers of the heart • Papillary muscles and trabeculae carneae muscles mark ventricular walls • Right ventricle pumps blood into the pulmonary trunk • Left ventricle pumps blood into the aorta Pathway of Blood Through the Heart & Lungs • Right atrium tricuspid valve right ventricle • Right ventricle pulmonary semilunar valve pulmonary arteries lungs • Lungs pulmonary veins left atrium • Left atrium bicuspid valve left ventricle • Left ventricle aortic semilunar valve aorta • Aorta systemic circulation Coronary Circulation • Coronary circulation is the functional blood supply to the heart muscle itself • Collateral routes ensure blood delivery to heart even if major vessels are occluded Heart Valves • Heart valves ensure unidirectional blood flow through the heart • Atrioventricular (AV) valves lie between the atria and the ventricles • AV valves prevent backflow into the atria when ventricles contract • Chordae tendineae anchor AV valves to papillary muscles • Right side tricuspid • Left side bicuspid Heart Valves • Aortic semilunar valve lies between the left ventricle and the aorta • Pulmonary semilunar valve lies between the right ventricle and pulmonary trunk • Semilunar valves prevent backflow of blood into the ventricles Microscopic Anatomy of Heart Muscle • Cardiac muscle is striated, short, fat, branched, and interconnected • Intercalated discs anchor cardiac cells together & allow free passage of ions – Sends impulses from cells • Heart muscle behaves as a functional syncytium – All muscle cells are connected & act as 1 unit Blood Vessels • Blood is carried in a closed system of vessels that begins and ends at the heart • Three major types of vessels: – Arteries – carry blood away from the heart – Veins – carry blood toward the heart – Capillaries – contact tissue cells & directly serve cellular needs Generalized Structure of Blood Vessels • Arteries and veins are composed of three tunics – tunica interna, tunica media, tunica externa • Lumen – central blood-containing space surrounded by tunics • Capillaries are composed of endothelium w/ sparse basal lamina • *arteries have more pressure flowing through them Elastic Arteries • Thick-walled arteries near the heart; the aorta & its major branches – Allow low-resistance conduction of blood – Withstand & smooth out large blood pressure fluctuations – Serve as pressure reservoirs – Help pump blood by stretching & constricting, moves the blood Muscular Arteries & Arterioles • Muscular arteries – distal to elastic arteries; deliver blood to body organs – Have thick tunica media w/ more smooth muscle – Active in vasoconstriction • Arterioles – smallest arteries; lead to capillary beds – Control flow into capillary beds via vasodilation and constriction Capillaries • Capillaries are the smallest blood vessels – Walls consisting of a thin tunica interna, one cell thick – Allow only a single RBC to pass at a time – Pericytes on the outer surface stabilize their walls • There are three structural types of capillaries: – Continuous – Fenestrated – Sinusoids Continuous Capillaries • Abundant in the skin, muscles, & brain – Endothelial cells provide an uninterrupted lining because of tight junctions between cells • Continuous capillaries of the brain: – Have tight junctions completely around the endothelium – Constitute the blood-brain barrier Fenestrated Capillaries • Found wherever active capillary absorption or filtrate formation occurs (e.g., small intestines, endocrine glands, kidneys) • Characterized by: – An endothelium riddled with pores (fenestrations) – Greater permeability than other capillaries Sinusoids • Highly modified, leaky, fenestrated capillaries w/ large lumens • Found in the liver, bone marrow, lymphoid tissue, & in some endocrine organs • Allow large molecules (proteins & blood cells) to pass between the blood and surrounding tissues • Blood flows sluggishly, allowing for modification in various ways Capillary Beds • A microcirculation of interwoven networks of capillaries, consisting of: – Vascular shunts – metarteriole-thoroughfare channel connecting an arteriole directly with a postcapillary venule • Closes blood flow if the tissues don’t need the blood & helps blood keep its oxygen – True capillaries – 10 to 100 per capillary bed, capillaries branch off the metarteriole and return to the thoroughfare channel at the distal end of the bed – Metarteriole – passageway between terminal arteriole & the postcapillary venuole Capillary Beds Venous System: Venules • Venules are formed when capillary beds unite – Allow fluids and WBCs to pass from the bloodstream to tissues • Postcapillary venules – smallest venules, composed of endothelium and a few pericytes • Large venules have one or two layers of smooth muscle (tunica media) Venous System: Veins • Veins are: – Formed when venules converge – Composed of three tunics: • Thin tunica media • Thick tunica externa consists of collagen fibers and elastic networks – Capacitance vessels (blood reservoirs) that contain 65% of the blood supply Venous System: Veins • Veins have much lower blood pressure & thinner walls than arteries • To return blood to the heart, veins have special adaptations – Large-diameter lumens – offer little resistance to flow – Valves (resembling semilunar heart valves), which prevent backflow of blood • Venous sinuses – specialized, flattened veins w/ extremely thin walls Blood Pressure (BP) • Force per unit area exerted on the wall of a blood vessel by its contained blood • The differences in BP within the vascular system provide the driving force that keeps blood moving from high to low pressure areas