HEMOPTYSIS by Prof. Arvind Mishra
advertisement

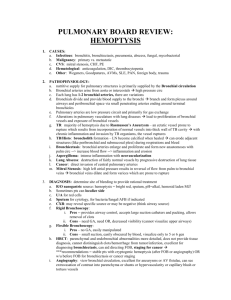
HEMOPTYSIS by Prof. Arvind Mishra M.D. Department of medicine What is Hemoptysis • Expectoration of blood from respiratory tract (from streaking to massive amount) Massive Hemoptysis • Expectoration of >100-600ml over a 24hr period • Acute life threatening condition. • Blood can fill the airways and the alveolar spaces. • Seriously disturbing gas exchange and may lead to asphyxia. Establish Hemoptysis • Should be differentiated from hemetemesis. • Fresh blood and froth on coughing. • Altered blood ( brown) with food particles in vomit. • Associated features. • Dilemma Once established, evaluate etiology A. Bleeding from tracheobronchial tree • • • • • Neoplasms- Bronchogenic CA Bronchitis – Acute/ Chronic Bronchiectesis Airways trauma Foreign Body B. Pulmonary Parenchymal Diseases • • • • • Tuberculosis Lung Abscess Pneumonia Wegner’s Granulomatosis Good Pasture’s Syndrome C. Primary Vascular Diseases • Mitral Stenosis • Pulmonary Embolism • A V Malformations D. Miscellaneous • Systemic Coagulopathy • Pt. on Anticoagulants / Thrombolytic agents Approach HISTORY • Blood streaking with mucopurelent sputum -Bronchitis • Fever with chills+ Blood with rusty sputum – Pneumonia • Blood + putrid sputum - Lung abscess • Blood + copious sputum - Bronchiectesis • Hemoptysis following acute onset of pleuritic Chest pain with dyspnoea – Pulm.Embolism H/O coexisting Disorders • Renal disease-Good Pasture’s Syndrome Wegner’s Granulomatosis • Lupus Eyrthematosus-Lupus Pneumonia • Non pulmonary malignancy-Endobronchial metastasis • AIDS-Kaposi’s Sarcoma • Risk factors for Bronchogenic CA-Smoking Asbestosis Also ask for • previous bleeding disorders • treatment with anticoagulants • use of drugs leading to thrombocytopenia PHYSICAL EXAM. • • • • • Pleural friction rub-Pulmonary Embolism Localised/Diffuse crepts-Parenchymal dis. Evidence of airflow obstr.-Chr.Bronchitis Ronchi +Crackles-Bronchiectesis CVS-Pulm.Hpt., Mitral stenosis, LVF Diagnostic Evaluation • Chest radiograph/CT Scan-- mass lesion, bronchiectatic Changes, focal areas of pneumonitis. • CBC • Coagulation profile • Assessment of renal profile– urine analysis,Blood urea,S.Creatinine • Sputum– Gm. Staining, C/S • Fibreoptic bronchoscopy– useful for localising the siteof bleeding and for visualisation of endobronchial lesions. • Rigid bronchoscopy– preferred when bleeding is massive because this procedure has better airways control and greater suction capability. Treatment What determines the urgency of management -Rapidity of bleeding -Effect on gas exchange (A) If streaking or small amount of bloodDiagnosis is priority. (B) If massive—Mx. Is top priority • Maintaining adequate gas exchange. • Preventing blood spilling into unaffected areas of the lung. Keep the affected lung in the dependent position to avoid aspiration of blood into the unaffected lung. • Avoid asphyxiation • Keep patient at rest/provide codeine containing cough suppressants- may help to stop bleeding. Management of massive bleeding • May necessitate - Endobronchial intubation - Mechanical ventilation to control airways and maintain adequate gas exchange. • To avoid blood spilling into contralateral lung (1)Selective intubation of non bleeding lung (2)Use of specially designed double lumen endotracheal tubes. • Another option- Inserting a ballon catheter through a bronchoscope under direct vision and inflating the ballon to occlude the branches leading to bleeding site. Other techniques • • • • Laser Phototherapy Electrocautery Bronchial artery embolism Surgical resection • Bronchial artery embolisation-it involves an arteriographic procedure in which a vessel proximal to bleeding site is cannulated and a material such as Gelfoam is injected to occlude the bleeding vessel. • Surgical resection of involved area of the lung—(a) Emergency therapy of life threatening hemoptysis that fails to respond to other measures. • (b) For the elective but definitive management of localised disease subject to recurrent bleeding. MCQs 1)Hemoptysis in mitral stenosis occurs due toa)Left atrial enlargement b)Right ventricular hypertrophy c)Bronchial arterial bleed d)Pulmonary venous congestion 2)A chronic smoker patient presenting with superior vena caval syndrome with hemoptysis. Most likely cause isa)Intrathoracic tubercular lymphadenitis b)Bronchogenic CA c)Lymphoma d)Aortic arch syndrome 3)A patient presenting with high fever ,chest pain and hemoptysis. CXR –Air bronchogram sign presenta)Lobar pneumonia b)Lung abscess c)Bronchiectasis d)Bronchogenic CA 4)A patient of hemoptysis presents with normal CXR. Suggest the next best investigation to help Dxa)Sputum cytology b)Bronchoscopy c)Thoracoscopy d)HRCT Thorax