HEMOPTYSIS:
advertisement

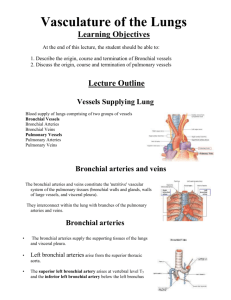
PULMONARY BOARD REVIEW: HEMOPTYSIS 1. CAUSES: a. Infectious: bronchitis, bronchiectasis, pneumonia, abscess, fungal, mycobacterial b. Malignancy: primary vs. metastatic c. CVS: mitral stenosis, CHF, PE d. Hematological: anticoagulation, DIC, thrombocytopenia e. Other: Wegeners, Goodpatures, AVMs, SLE, PAN, foreign body, trauma 2. PATHOPHYSIOLOGY: a. nutritive supply for pulmonary structures is primarily supplied by the Bronchial circulation b. Bronchial arteries arise from aorta or intercostals high pressure circ c. Each lung has 1-2 bronchial arteries, there are variations d. Bronchials divide and provide blood supply to the bronchi branch and form plexus around airways and peribronchial space via small penetrating arteries ending around terminal bronchioles e. Pulmonary arteries are low pressure circuit and primarily for gas exchange f. Alterations in pulmonary vasculature with lung diseases lead to proliferation of bronchial vessels and exposure of bronchial vessels g. TB: majority of hemoptysis due to Rasmussen’s Aneurysm – an ectatic vessel prone to rupture which results from incorporation of normal vessels into thick wall of TB cavity with chronic inflammation and invasion by TB organisms, the vessel ruptures h. TB/Histo: broncholith formation – LN become calcified when healed can erode adjacent structures (like peribronchial and submucosal plexi) during respirations and bleed i. Bronchiectasis: bronchial arteries enlarge and proliferate and form new anastomoses with pulm circ --> increase blood flow --> inflammation and erosion j. Aspergilloma: intense inflammation with neovascularization k. Lung Abscess: destruction of fairly normal vessels by progressive destruction of lung tissue l. Cancer: direct invasion of central pulmonary arteries m. Mitral Stenosis: high left atrial pressure results in reversal of flow from pulm to bronchial veins bronchial veins dilate and form varices which are prone to rupture 3. DIAGNOSIS: determine site of bleeding to provide rational treatment a. R/O nasogastric source: hemoptysis = bright red, sputum, pH=alkal, hemosid laden M b. Sometimes pts can localize side c. U/A for red cells d. Sputum for cytology, for bacteria/fungal/AFB if indicated e. CXR: may reveal specific source or may be negative (think airway source) f. Rigid Bronchoscopy: i. Pros -- provides airway control, accepts large suction catheters and packing, allows removal of clots ii. Cons – need GA, need OR, decreased visibility (cannot visualize upper airways) g. Flexible Bronchoscopy: i. Pros – no GA, easily manipulated ii. Cons – small suction, easily obscured by blood, visualize only to 5 or 6 gen h. HRCT: parenchymal and endobronchial abnormalities more detailed, does not provide tissue diagnosis, cannot distininguish clots/hemorrhage from tumor/infection, excellent for diagnosing bronchiectasis, can aid directing FOB, staging for cancer ***recommendations = stable pts with cryptogenic hemoptysis (after FOB or angiography) OR w/u before FOB for bronchiectasis or cancer staging i. Angiography: view bronchial circulation, excellent for aneurysms or AV fistulae, can see extravasation of contrast into parenchyma or shunts or hypervascularity or capillary blush or tortuos vessels 4. MANAGEMENT: a. airway control to prevent asphyxiation: split lung ventilation (double lumen tube) to protect nonbleeding lung from further spill over (difficult to insert, small bores difficult to suction and easily obstructed by clots, difficult to bronchoscope through), Rt mainstem if bleeding from Lt b. volume resuscitation c. follow HCT, check T & C, correct coagulopathies d. cough suppression, but avoid excessive sedation e. lie on side of lesion f. role of antibiotics if bronchitis, bronchiectasis, TB… g. quantify rate of bleeding: i. >1000 ml/24 or hypovolemic shock or inadequate airway control or inadequate gas exchange early surgical intervention should be attained ii. 500-1000 ml/24 nonsurgical approach via local control of endobronchial bleed or embolization and then when stabilized if recurrent a surgical approach may be attained iii. <500 ml/24 expectant observation following appropriate diagnostic procedures, be more aggressive if more than 4 days 5. INTERVENTIONS: a. Bronch: apply packing to tamponade, ballon tamponade (fogarty), coagulants (fibrin precursors), lavage with iced saline, coagulating lasar therapy b. Bronchial Artery Embolization: i. Remy in 1977: 104 pts, 49 during acute bleeding ( 41/49 had bleeding controlled and 6/41 had recurrent hemoptysis in next 2-7mths.) ii. Overall controls active bleeding in 90% iii. Common recurrence 10-27% 1-2 mths see failure to completely embolize bleeder vessels or to identify the nonbronchial systemic collaterals OR 1-2 yrs later b/c of new recruitment of collateral vessels by underlying disease or recanalization of embolized vessels may need recurrent embolizations iv. bridge to surgery or control in those that dont have sufficient reserve for surgery v. Complications: ant spinal arteries arise form bronchial arteries in 5% embolic infarction of spinal cord, contrast induced transverse myelitis, embolism to arterial system if AV fistulae or shunts or retrograde to aorta c. Surgery: i. If life threatening or uncontrolled by non-surgical methods ii. For elective basis for definitive treatment of anatomically circumscribed lesions iii. Need to preop: PFT’s, V/Q scan… iv. Complications: bronchopleural fistula (10-14%), pulm hemorrhage, lung infarction, wound infection, hemothorax/empyema, and resp insufficiency v. Increased mortality when performed during acute bleeding ~37% 6. PROGNOSIS: a. ***short term mortality directly related to rate of bleeding, NOT underlying pathology b. 600 ml/4 = 71% mortality c. 600 ml/4-16 = 45% d. 600 ml/ 16-48 = 5% e. higher for those deemed inoperable, regardless whether treated medically or surgically f. low mortality among those deemed operable, whether treated medically or surgically g. biases = surgical results b/c selection for pts with most severe bleeding vs. medical pts have poor prognosis b/c deemed not surgical candidates b/c of advanced disease, different criteria for massive hemoptysis, changing in prevalence of causes of hemoptysis