Sue Estroff: Reconcilable Differences? Finding
advertisement

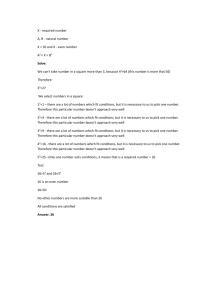
MEANS AND ENDS Getting to Consumer Centered and Provider Sustaining Services Ultimate Origins vs….. Proximate FALSE POSITIVES MEDICATION SIDE EFFECTS TIME LIMITED TX BENEFIT LABELING AND STIGMATIIZING INADEQUATE TREATMENT RESOURCES Developing a Research Framework for Evaluating Comparative Effectiveness of Health Care Delivery Interventions to Improve Patient Outcomes in Serious Mental Illness Directions for Future Patient-Centered & Comparative Effectiveness Research for People with Serious Mental Illness: A Definition of Care, a Care System Model, an Analytic Framework to Guide Future Research, and Key Questions Carla A. Green, PhD, MPH Sue E. Estroff, PhD BobbiJo H. Yarborough, PsyD Mark Spofford, PhD Michele R. Solloway, PhD Rachel Kitson, BS Nancy A. Perrin, PhD Care and Service Delivery Intervention Definition A patient-centered intervention for people with serious mental illnesses is defined as an organized process of care or service delivery that is directed by the person receiving services. Care and/or services are delivered collaboratively, attentively, and compassionately, with providers as partners who understand and respond to the person’s perspective and concerns. The delivery process is structured to educate, inform, guide, and assist the person to be a knowledgeable consumer of the services relevant to attaining the person’s self-defined needs, goals, circumstances, and outcomes. All individuals, including those who have been diagnosed with a serious mental illness, have the right to direct their own care. People who are limited in their ability to direct their care as a result of acute symptoms or legal constraints should be provided with the support necessary to make as many care-direction decisions as possible. If a person is unable to make informed choices about their care, providers will rely on historically expressed preferences and values and, when available, psychiatric advance directives and designated surrogates to maximize the person’s participation in decision-making about services and treatment. Care decisions made for persons when they are unable to direct their own care should be based on the premise that such decisions will enable those persons to make future choices about their care. Care and services provided should take into account available scientific knowledge and the resources of the service system. “The involvement of mental health service users in service delivery is a new and growing phenomenon. Such involvement is complex, given the history of paternalism in the mental health system, the power differential between service providers and service users, and the very differing views each group holds on multiple issues. Unless such differences are addressed, there can be no meaningful involvement. Service user involvement needs to apply to all aspects of the service delivery system, including professional training, service design, delivery, evaluation, and research. User/survivors, and their organizations, have developed a body of experience and knowledge that needs to be recognized and respected. Unless there are multiple opportunities for ongoing and open dialogue on these many difficult issues, real user involvement will not occur (p. 20).”37 --Judi Chamberlin, author and activist 3. The needs of stakeholders that are most commonly agreed upon concern qualities of person, place, and relationships. Choice, respect for persons, attending to basic needs for safety and material living needs, and competence of care are shared aspirations and expectations for mental health services. Therapeutic relationships and working alliances are the fulcrum of mental health services, yet the facets, requirements for, and barriers to this central ingredient have not received adequate attention in research and service design and provision. 4. Processes of collaboration in patient-provider relationships are complicated and easier to imagine than achieve. The widespread deployment of peer providers within, and as adjunct to, mental health services has moved relatively swiftly, as has the number of consumer operated services. It is important to assess these moves with the understanding that their goals and mechanisms differ from those of more traditional providers. 5. The unintended consequences of treatment receive scant attention in outcomes research, and as a result, services and systems lose the opportunity to be self-correcting, learning systems. The use of coerced and involuntary treatment in hospitals and community settings, as well as the more subtle and pervasive manipulation of choice, represent possible sources of injury or harm for consumers, families, and even providers. 1. Consumers, families/carers, and providers predictably diverge in their assessments of consumer needs for services, and in their assessments of consumers’ status and outcomes. They differ in language, conceptual frameworks, in the bases for their assessments, and in how needs are prioritized. These differences are most apparent in definitions, and thus assessment, of recovery processes. Recovery is increasingly being translated into an outcome by research and policy. The condensation, standardization, and interpretation involved in mainstream outcomes research and evidence-based policy may fundamentally alter and obscure the nuance, complexity, and power of the recovery process. Consumer-directed and informed research is of particular importance and salience here. It is important to distinguish between value-based and evidence-based outcomes practices when assessing the effectiveness of services. Some treatments and services, and the qualities of their provision, are endorsed because they enact deeply held values, not necessarily because there is evidence that substantiates their effectiveness. 2. Demonstrable progress has been made in engaging stakeholders in evaluating treatment and services and in formulating federal, state, and local policy. Organization and financing models, however, are often taken as inevitable, and trump many of the expressed opinions and evidence from these groups and individuals. Providers in particular are awash in reimbursement criteria and documentation, ever-changing requirements for accountability, and inadequate resources. These strictures have a direct impact on their ability to promote the kinds of healthy working alliances with consumers and families/carers that produce continuous healing relationships. Summary. The quality of relationships between patients and providers is perhaps one of the best- documented influences on assessments of care and outcomes and the least attended to in implementation, intervention development and testing, and reform of system level factors that impede patient-provider relationships. Quality and experiences of treatment are clearly seen as patient-centered outcomes among consumers. THERAPEUTIC IMPERATIVE STATUTES, RULES, RESOURCES, RISKS THIS IS YOU I WISH I COULD HELP YOU. THE PROBLEM IS THAT YOU’RE TOO SICK FOR MANAGED CARE Almost all U.S. adults with schizophrenia were found to receive government health insurance, yet a measurable minority remained uninsured. Eighty-seven percent had Medicaid or Medicare, 8% received care through the Veterans Health Administration, and 15% had private insurance for at least one day during the year. About 7% were uninsured all of the year. (Khaykin et al 2010) The vocabulary and practices of current mental health case management are infused with collaboration, consumer choice, shared decision-making, empowerment, recovery and individualized services. The terminology and requirements of the workplace, in stark contrast, are dominated by accountability, making budget, billable units, meeting productivity expectations, deadlines for paperwork, and auditor’s checklists. The juxtaposition of recovery promoting concepts and practices with those of the reporting, auditing, and performance requirements of public (and to some extent private) funding raises questions of whether or how these two are compatible, and together contribute to or interfere with improved consumer outcomes. One staff member remarked, “no one knows what a service coordinator is…we are known as case managers all over the country.” In this context, the reforms were seen as a change in vocabulary that was unlikely to affect practice in a meaningful way, and by some supervisors and service coordinators as additional demands made without the commitment of additional resources. It was common to hear from the informants that “they [administrators and policy designers] have no idea what we actually do,” and that “It [paperwork] has always been tough, but now it is not bearable.” During the course of the study, we interviewed all of the SC supervisors in the sites and asked them to identify the qualities they looked for and valued when hiring and assessing active service coordinators. These attributes can be summarized as: Passion and Heart Problem Solving Ability Experience Relationship Skills Self-Reliant Specific qualities included: Dedication, flexible, won’t settle, creative, trust with others, sense of humor, able to handle frustration and anger, high expectations of self, and ‘no time is ever wasted.’ Case Management Transformation: Single Point of Accountability • Recovery orientation • Become central service coordinators across system • Develop high level Recovery Plan from all supports • System engages differently with case managers • Comprehensive training • Revamped and extended basic training provided by SSW • Addition of mentors • Enhance career ladder SPA Affirmative Responsibilities Go-to person for the consumer/family/system Clearly communicate what can be expected Planning with consumer for development of natural supports, link consumer with resources Assure cross-systems assessment and planning Assure cross-systems coordination Develop relationships that endure Give feedback on systems barriers and problems Provide primary safety net function Help sustain positive outlook for the future Overview of implementation plan • Phase in all system changes over five years • Increase rates and salaries over five years • County contracts re-written to enhance accountability of agencies to implement • Case Mgt competencies & responsibilities tied to common job description and to job evaluations Finance • Agencies collaborated with county to achieve more comparable salaries • 10% rate increase approved to fund salary increases • $8,000 increase in minimum starting salary Workforce Job descriptions re-written Name changed to “Service Coordination” Comprehensive training developed Mentors instituted in all SC agencies Three local Schools of Social Work worked to develop BASW Service Coordination certificate Plan to expand to Psychology 100-hour certificate through CE for other majors & current staff 100-hour certificate through CE for mentors County Standardize and centralize new hire trainings on policies/procedures Workforce recruitment plan developed What we learned • Many opportunities to observe the different cultures and practices of community practice and academia • Opportunity to define the “jagged edge” • Demanding, but different incentive structures • Medicaid and Service Definitions • Program announcements and cutoff scores • Different timeframes • Providers are ready to implement immediately • “Chasing baselines” • Different regulators • CMS vs. IRB Case Management Research • Consumer Base Line Study • Interviews with Mentors • Participant observation study of implementation • Follow-up Mixed Methods study (Summer 2010) • Staff retention (pre and post) • Salary surveys (pre and post) • Training survey (pre and post) BILLABLE UNIT REQUIREMENTS ↔↔↔↔↔ 1 “MAKING BUDGET” AGENCY SURVIVAL=MY JOB MORALE, PERFORMANCE, AND TURNOVER/RETENTION CASELOAD SIZE AND TYPE AUDITING: INTERNAL AND EXTERNAL ADMINISTRATIVE REQUIREMENTS CHANGES IN REPORTING FORMAT AMOUNT AND TIME TO COMPLETE TRAINING TIME MENTORS The service coordinators and supervisors were ever mindful of the precarious fiscal condition of their agency, and understood that their work was in part responsible for the financial health of the agency, and ultimately their jobs. Nearly all service coordinators keep a running account of billable units per day, and many have developed an internal gauge that they update as their interaction with consumers unfolds. As one explained, “I can see one encounter leading to a whole bunch of [additional] billable units with the labs and appointments.” Most SCs are also conscious of the necessity of justifying their time. “I have to show that I’m not just giving rides,” one SC stated, noting that if a visit with a client lasted for 30 minutes, he needed to show “30 minutes of activity.” 2 COORDINATION AND COMMUNICATION + CHALLENGES “BEING THE HUB IS DIFFERENT THAN ‘WHATEVER IT TAKES” “SPA MEETINGS” “FROM TAXI TO TRAVEL GUIDE” DOCS AND THERAPISTS CONSUMER OUTCOMES 3 Q46 (k) Overall, are you satisfied with the respect shown to you by the service coordinator who works with you? Dissatisfied ............. 10 Satisfied ................... 381 (2%) Q49 Neutral .................... 12 (95%) (3%) Overall, how satisfied are you with the service coordination services you received? Dissatisfied 12 (3%) Satisfied...... 349 (87%) Neutral........ 35 (9%) Unsure ....... 4 (1%) I need to see him more often. He knows I need to, but he has problems of his own. At least weekly visits. I had a visit every two weeks and I would have liked to have them every week. Visits have been decreased to once a month. They told me that the visit will be decreased. I'm going through something right now, therefore I'd like to see her more, so she can help me with it all. I rarely see her; I get no visits. I would like to see my service coordinator more often than once a month. I would like more visits, more than one or two times per month. I want more. Weekly. My service coordinator is too busy to see me as much as I would like. Would like service coordinator to come several times a week. I could use one or two visits a week. She comes about two or three times a month. Would like visits every two weeks. I'd like to see her once every two weeks, instead of every three weeks. Mayview Overview Trajectory Types/Outcomes Stable (at limit, satisfied, QOL) Stuck (could but can’t due to lack of resources/services) Stuck (won’t engage with services that would promote recovery that are available) Decline (steady, gradual, episodic) quietly, intensive services Improve (steady, gradual, episodic) intensive services, self-directed • “The best experience has been knowing that I can make it in the real world. Not as hard as I projected it to be.” Leaving Mayview: The Sanity of Place Percent with at least moderate illness (BPRS >41) 45 40 35 30 Hosp 25 6 mo 20 12 mo 15 18 mo 10 24 mo 5 0 F (4, 196) = 2.44, p < .05 Progress needed on community integration • Many participants would welcome more varied activities • Q: What do you do? A: Sleep. Get up and watch TV. Come out here and smoke. • Q: What is there to do? A: Sleeping. Groups. That’s about all. • I don’t go anywhere. I don’t have any money. • Some participants are very active • I am in the process of getting prepared to get a job. I’ll see what kinds of things I want to do. Some do not get the chance to rise like golden loaves of hallah, filled with sweet raisins and crowned with shiny braids. Rushed, neglected, not kneaded by caring hands, we grow up afraid that any touch might cause a break. There are some ingredients we never receive. Tonight, let us bless our cracked surfaces and sharp edges, unafraid to see our brittleness and brave enough to see our beauty. Reaching for wholeness, let us piece together the parts of ourselves we have found, and honor all that is still hidden. Tamara Cohen Gould Farm Wordpress