L5_Parkinson's Disea..
advertisement

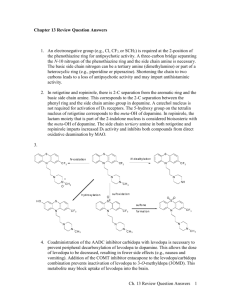
Parkinson’s Disease Ibrahim Sales, Pharm.D. Assistant Professor of Clinical Pharmacy King Saud University isales@ksu.edu.sa Learning Objectives • Describe Parkinson’s Disease • List drugs used in the treatment of Parkinson’s Disease • Describe the pharmacological management of each drug used in the treatment of Parkinson’s Disease • Describe the mechanism of action, toxicities, and pharmacokinetics of drugs used to treat Parkinson’s Disease Parkinson’s Disease (PD) • Second most common neurodegenerative disease • Clinical symptoms are motor and nonmotor • Diagnosis based on motor symptoms • Etiology is unknown • No treatment can stop the progression of PD Epidemiology • Gender non-specific • Average onset is approximately 60 years old • Risk increases with age Clinical Presentation • d Pharmacological Management • There is no treatment that can stop or reverse the loss of dopaminergic neurons • Symptomatic relief • Strategies – Increase the amount of dopamine activity in the brain – Decrease the amount of cholinergic brain activity – Both (dopamine and acetylcholine need to be in balance for normal, balanced movement) Therapeutic Goals • Reduce the incidence and severity of motor and nonmotor symptoms • Maintain quality of life • Improve activities of daily living • Minimize complications of drug therapy Levodopa • First introduced in the 1960s • Gold standard • Dopamine cannot cross the blood-brain barrier • Levodopa (amino acid) precursor of dopamine • Carbidopa – decarboxylase inhibitor in peripheral body tissues Levodopa • Ameliorates the motor symptoms • Improves QOL, lengthens independence and decreases mortality rate • Effects last for several hours initially • Therapeutic response nears t½ eventually Levodopa • Rapidly absorbed from the small intestines • High-protein meals will delay absorption and decrease peak plasma concentration • Peak plasma concentration: 0.5 to 2 hours • t ½ : 1 to 3 hours Levodopa • Contraindications: – Psychotic patients, closed-angle glaucoma, active peptic ulcer (monitor closely), MAO inhibitor if taken within 14 days, undiagnosed skin lesion or history of melanoma • Pregnancy risk factor C • Adverse effects: – Nausea, vomiting, anorexia; postural hypotension; nightmares, agitation, confusion insomnia, depression, somnolence, anxiety Levodopa • Patients may develop myoclonus or dystonia when medication is at its peak concentration • Dyskinesia is not disabling if mild; only severe • “On-off phenomenon” – Initial responders • Decreased absorption/effect: – Oral iron salts (except iron sucrose, ferumoxytol, iron dextran complex and ferric gluconate); sapropterin, metoclopramide, phenytoin, pyridoxine, kava kava; methylphenidate can increase levodopa toxicity Levodopa • Usually prescribed with carbidopa • IR tablet: carbidopa 25mg/levodopa 100mg TID – Increase dose by one tab every other day • Carbidopa 25mg/levodopa 250mg – Increase dose by ½ tab every 1 to 2 days • Max number of tablets is 8 or 200mg carbidopa and 2000mg levodopa Levodopa • Sustained release • Carbidopa 50mg/levodopa 200mg BID at least 6 hours apart – Increase dose every 3 days • Max number of tablets per day is 8 • Initial dose for elderly is carbidopa 25mg/levodopa 100mg two tablets daily Dopamine Agonists • Directly stimulate dopamine receptors • Ergot dopamine agonists (bromocriptine) • Non-ergot dopamine agonists (pramipexole and ropinirole) – Stimulate the D3 and D2 receptors • Ineffective in patients that do not respond to levodopa • Monotherapy or in combination with carbidopa/levodopa – Can postpone levodopa use • Improves tremor, bradykinesia, and rigidity • Dopamine agonists last therapeutically longer than levodopa • Minimize fluctuations in dopamine blood concentrations, allow for levodopa dose reduction, improve ADLs Bromocriptine • Partial dopamine agonist • Ergot derived • Ergot derived side effects: Pulmonary/cardiofibrosis infiltrates • Dosing: 1.25 mg BID – Increase at 2 to 4 weeks by 2.5mg/day – Average dose: 20-40mg daily in TID or QID doses – Max dose: 90mg/day Rotigotine • Transdermal Patch – Daily patch formulation – Start at 2mg/24 hours; max 6mg/24 hours – Do not discontinue abruptly • Neuroleptic malignant syndrome like • Akinetic crisis Pramipexole • Stimulates the D3 receptors • May be prescribed for mild cases of PD; especially effective for treating patients experiencing the “on-off phenonmenon” – Reduces the “off” time Pramipexole • Rapidly absorbed from the GI tract • Plasma concentration peaks in 2 hours for the IR form; peaks in 6 hours for the extended release form • t ½ is 8.5 hours; 12 hours for the elderly • Excreted in the urine, 90% unchanged Pramipexole • Initial dose for the IR form is 0.375mg daily divided into 3 doses – Titrate dose every 5 to 7 days to minimize adverse effects – Maximum dose 4.5mg daily CrCl (mL/min) >60 35 to 59 15 to 34 Initial dose 0.125mg TID 0.125mg BID 0.125mg daily Maximum dose 1.5mg TID 1.5mg BID 1.5mg daily • Initial dose for the ER for is also 0.375mg daily – Titrate dose by 0.75mg a day every 5 to 7 days – Maximum dose is 4.5mg a day – CrCl 30 – 50 mL/min, dose every other day up to 2.25mg daily Pramipexole • If discontinuing, taper over one week – Risk of developing a disorder resembling neuroleptic malignant syndrome • Pregnancy risk factor C Ropinirole • Stimulates the D2 receptor and is effective in mild cases • Effective in patients in an advanced stage who have “on-off phenomenon” • Absorbed in the GI tract; unaffected by food • Plasma concentration peaks at 1 to 2 hours for IR form; 6 to 10 hours for ER form • t ½ 6 hours • Excreted in the urine; clearance is decreased from 15 to 30% in patients over 65 years old Ropinirole • Initial dose for the IR tablet for the first week is 0.25mg TID – – – – – Titrate slowly to avoid toxic effects Week 2: 0.5mg TID Week 3: 0.75mg TID Week 4: 1mg TID Can increase by 1.5mg a day on a weekly basis up to a total dose of 9mg a day – Can raise dose by 3mg a day on a weekly basis up to a total of 24mg a day Ropinirole • If discontinuing, gradually taper over a 7 day period – Frequency should be decreased to BID for the first 4 days then lowered to once daily for the remaining 3 days Ropinirole • The initial dose for the ER tablet is 2 mg once daily for the first 1 or 2 weeks • The dose can be increased by 2 mg a day on a weekly basis with the maximum dosage as 24mg daily • Taper in the same manner as the IR tablet Apomorphine • Stimulates D2, D3, D4, and D5 receptors • “Rescue therapy” for a patient who has severe “off” period and is not responding to other medication • Subcutaneously injected • Therapeutic benefit begins in 10 minutes and lasts for 2 hours • Plasma concentration peak in 20 minutes • t ½ is 40 minutes Apomorphine • Contraindications – Hypersensitivity to apomorphine or ingredients; administration IV; concomitant use with serotinin antagonists (loss of consciousness and extreme hypotension) – Toxic effects include hypotension, chest pain, dyskinesia, sweating, drowsiness, falls, abnormal EKG (QT prolongation), nausea and vomiting (pre and post antiemetics ) • Trimethobenzamide at 300mg TID should be started 3 days before the patient receives the first dose and continued at least for the first 2 months • Ondansetron is a serotonin antagonist and should not be used Apomorphine • Three days before initial dose, administer trimethobenzamide 300mg TID; continue for 2 months then assess • Initial dose is a test dose of 2mg given during an “off” period • If patient tolerates the test dose, start at 2mg – May increase dose by 1mg every few days • Max dose is 6mg Apomorphine • Patients tolerating the test dose, but not therapeutically responding – 2nd test dose of 4mg administered – If responds, starting dose is 3mg – Increase dose every few days; max is 6mg • Patients who don’t tolerate the test dose of 4mg – 3rd test dose of 3mg can be given – If tolerated, the start dosage is 2mg – 2mg dose may be increased by 1mg to a max of 3mg Apomorphine • If not administered for more than 1 week, the start dose is 2mg; the dosage must gradually be increased • Standing and supine BP must be checked before administering a test dose – Both pressures must be checked 20, 40, and 60 minutes after the test dose – If additional test dosed are needed, there must be a 2-hour wait before the next test dose which should be only given during an “off” period Apomorphine • Use cautiously in patients with mild to moderate impairment of the liver • The test dose and starting dose should be 1mg for patients with mild to moderate renal impairment • Pregnancy risk factor C Dopamine Agonists ADEs • Nausea, vomiting, dyskinesias, somnolence, sedation, hallucinations, nightmares, confusion, and postural hypotension • Obsessive-compulsive disorder and impulsecontrol disorder • Excessive daytime sleepiness – Modafinil 200 – 400mg daily MAO-B Inhibitors • Monoamine oxidase type B is an enzyme which metabolizes dopamine to homovanillic acid in the striatum • Selegiline and rasagiline interfere with dopamine metabolism, thereby increasing the concentration of dopamine at the neuronal synapse MAO-B Inhibitors • They provide some therapeutic benefit when used as monotherapy in early or mild symptomatic PD • May decrease the effects of the “off” period when administered with levodopa and prolong its effects, allowing the dosage of levodopa to be reduced Pharmacokinetics • Selegiline – Effects start within 1 hour and last for 24-72 h – T ½ is 10 h for the tablet, but 18 to 25 for the transdermal form • Rasagiline – Effects start within 1 hour and last for 1 week – T ½ is 1.3 to 3 h Selegiline and Rasagiline • Dyskinesias may increase if administered with levodopa, but can be controlled by lowering the levodopa dose • Potential for serotonin syndrome • Pregnancy risk factor C • Adverse effects – Selegiline: nausea, confusion, hallucinations, insomnia, headache, jitteriness, orthostatic hypotension, dyskinesias – Rasagilinie: diarrhea, weight loss, hallucinations, rash – Tyramine – hypertensive crisis Dosing • Selegiline – 5mg BID at breakfast and lunch (insomnia) – Initial dose for ODT is 1.25mg daily x 6 weeks • May increase to max dose of 2.5mg daily • Rasagiline – 1mg daily if needed and tolerated – Lower levodopa dose 9 to 13% (dyskinesias) – Mild hepatic impairment dose: 0.5mg daily • Avoid in moderate to severe hepatic impairment COMT Inhibitors • The enzyme catechol-o-methyltransferase (COMT) metabolizes dopamine to homovanillic acid • Levodopa is mainly metabolized by COMT • COMT inhibitors increase the levodopa halflife and allow more levodopa to cross the BBB • COMT administered with levodopa decreases the “off” period and increases the “on” period • Possible lowering of the levodopa dosage COMT Inhibitors • Entacapone – Quickly absorbed; quick onset of action – Peak effect at 1 hour – T ½ is 2 hours • Tolcapone – Rapidly absorbed – T ½ is 2-3 hours – Peak plasma concentration in 2 hours Adverse Reactions • Entacapone – Diarrhea, brown-orange colored urine from the accumulation of metabolites, dyskinesia, nausea and vomiting • Dyskinesia and nausea can be decreased or avoided by lowering the dose of levodopa by 20 to 30% in the first 48 hours of administering entacapone Adverse Reactions • Tolcapone – Same as entacapone – Dyskinesia and nausea can be decreased by lowering the levodopa dose, but the diarrhea can be so severe that 5 to 10% of patients d/c – Dizziness, hallucinations, somnolence, postural hypotension; hepatic toxicity (some fatal cases) • Administer if no other treatment is available or responsive; patients must sign a consent form; liver enzymes must be monitored every two weeks for the first year Dosing • Entacapone – With every dose of levodopa/carbidopa, 200mg is prescribed – Max frequency is 8x daily; max dose is 1600mg daily • Tolcapone – – – – More potent; advanced patients 100mg TID; can be increased to 200mg TID If no improvement in 3 weeks, d/c If hepatic impairment develops, d/c • Both medications are pregnancy risk factor C Anticholinergics • Antimuscarinic anticholinergic medications lower the actions of the cholinergic neurons in the striatum; basis for therapeutic effects is not understood • Due to the toxicity of the other PD medications, if the patient is in early stages of PD, not elderly and the main symptom is tremor, may prescribe Anticholinergics • Benefits: – Rest tremor – Urinary frequency – Excess sweating – Drooling • Less effective for bradykinesia, rigidity, or gait problems Anticholinergics • Elderly concerns – Increased risk of confusion, cognitive problems, hallucinations – Dementia • 2.5-fold increase in amyloid plaque and neurofibrillary tangle densities • Baseline cognition evaluation, psychiatric history, and blood pressure • Monitor for typical symptoms; decreased gastric acid secretion; decreased gastric emptying Anticholinergics • Trihexyphenidyl – t ½ or 33 hours – Plasma concentration peaks in 1.3 hours • Benztropine – Effects start in 1 hour and lasts for 6 to 48 hours Adverse Reactions • Constipation, urinary retention, mydriasis, blurred vision, tachycardia, confusion, hallucinations, nausea, vomiting, hyperthermia • Use with caution in CV disease, renal impairment, hepatic impairment, glaucoma, and prostatic hyperplasia • KCl can interact and lead to ulcers Dosing • Trihexyphenidyl – Initial dose is 1mg daily • • • • Increase by 2 mg every 3-5 days Usual dose is 6-10mg daily in 3-4 doses Some patients need 12-15mg daily If prescribed with levodopa, dose is 3-6mg daily in divided doses • Benztropine – Initial dose is 1 to 2 mg daily in 2-4 doses • May increase dose by 0.5mg each week; max 6mg/daily • Avoid in patients > 60 years of age • Pregnancy risk factor C Amantadine • Releases stored dopamine and inhibits the NMDA glutamate receptor (excitatory) • Prescribed in early PD; primarily prescribed to decrease the dyskinesia, tremor and rigidity of the advanced stage • May only be beneficial for a few weeks or months Amantadine • Well absorbed and takes effect within 48 hrs • t ½ from 9 to 31 hrs • Plasma concentration peak of 2 to 4 hrs • Adverse effects – Nausea, dizziness, insomnia, livedo reticularis (benign purple mottling of the skin of dependent extremities), peripheral edema, orthostatic hypotension, hallucinations, and confusion – Its stimulant action may worsen insomnia and restlessness Dosing • Standard dose for monotherapy is 100mg BID – May be increased to 400mg daily in divided doses • Patients taking high doses of other medications for PD – Initial dose is 100mg daily • Dose can be increased after 1 week or more to 100mg BID • Pregnancy risk factor C Treatment Algorithm Treatment Algorithm Treatment Algorithm Wearing off therapy • If monotherapy with levodopa – Increase frequency of levodopa • Change to SR/CR formulation – Increase dose of levodopa – Add a dopamine agonist – Add COMT-I • If monotherapy with dopamine agonists – Add carbidopa/levodopa • Apomorphine – rescue therapy • Diet – Avoid high protein On-Off Phenomena • Rapid fluctuations from “on” to “off” motor states • Freezing gate • Occurs in patients with advanced disease – Have motor fluctuations – Dyskinesia – On chronic levodopa • Increase the frequency of levodopa • Add dopamine agonist • Add COMT-I