Managing Involuntary Weight Loss
advertisement

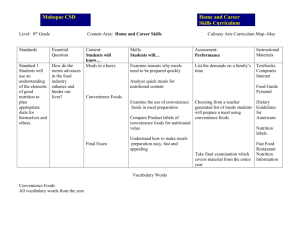
Managing Involuntary Weight Loss in Older Adults Jeannine Lawrence, PhD, RD, LD Division of Human Nutrition Learning Objectives • Identify potential causes of involuntary weight loss in older adults (OAs) • Explore the potential impact of involuntary weight loss on physical function and health outcomes in this population • Describe the goals of weight management in OAs during illness • Discuss effective, multidisciplinary strategies for ameliorating involuntary weight loss in OAs Definitions & Prevalence • Unintentional weight loss - loss of body mass that can occur due to illness or disease, stress, psychological conditions, and/or unknown causes • Weight loss = >3% of body weight or 2 kg • Clinically relevant – >5% body weight in 6 months • “Problematic” weight loss – ≥5% in 1 month – ≥10% in 6 months or longer US Omnibus Budget Reconciliation Act of 1987 Definitions & Prevalence (cont.) • Undernutrition - common in older adults in Geriatric Med. 2002) – – – – 5-12% of community-residing older adults 11% of medical outpatients 20% of higher-risk, community-residing 32-50% of hospitalized • Involuntary weight loss – Affects 15-20% of older adults – Contraindicated in the OA • Including the obese OA (Clinics Factors Associated with Unintentional Weight Loss M – Medication effects E – Emotional problems, esp. depression A – Anorexia nervosa, alcoholism, abuse L – Late-life paranoia S – Swallowing disorders O – Oral factors (e.g. taste, teeth, poorly fitting dentures, caries) N – No money (poverty) W – Wandering and other dementia-related behaviors H – Hyper- and hypothyroidism, hyperparathyroidism, hypoadrenalism E – Enteric problems E – Eating problems (e.g. difficulty/inability to feed self) L – Low-salt, low-cholesterol diets S – Shopping or social issues (e.g. inability to obtain preferred foods, isolation, etc) Morley 1995 Comparison of Causes of Unintentional Weight Loss in OA 70 60 50 40 OP (n=45) 30 LTC (n=185) IP (n=154) 20 OP + IP (n=91) 10 0 No identified cause Psychiatric disorder (including depression) Cancer Benign GI disorder Medication effect Neurologic disorder Other (hypothyroidism, poor intake, TB, food avoidance, DM, etc) Huffman 2002 Functional & Health Outcomes • Physical function – loss of skeletal muscle mass→ frailty → decreased mobility • Health Outcomes – exacerbate disease – ↓ immune function – ↑ morbidity and mortality Nutrition Screening Tools • DETERMINE and MNA – extensively validated, identify at-risk OAs • Nutrition Screening Initiative (NSI) – 25 national health and aging organizations – Developed the Determine Your Nutritional Health Checklist to highlight warning signs of malnutrition – Level I – BMI, weight change, eating habits, living environment, and functional status questions – Level II – anthropometrics, lab data, clinical exam, cognitive/mental status evaluation Lipschitz 1992 Nutrition Screening Tools (cont.) •Mini Nutritional Assessment (MNA) – short and long forms Step 1 - Assessment • Anthropometrics (ht, wt, wt change) – BMI • height may be inaccurate 2° osteoporosis • may not be an accurate estimate of lean mass • 24.0-29.0 may be optimal Beck 1998 • Medical hx, labs • Medications and supplement use • Physical function, physical activity (↓ associated with poorer appetite) • Psycho/Social – cognition, depression, social support and interaction Dietary Intake Assessment in OAs • Methods – Diet records – 24-hr dietary recall – FFQ – Diet history • Validity of multiple methods are comparable to younger adults Special Considerations for Dietary Intake Assessment in OA • Memory impaired – Must assess cognitive abilities – Avoid - Recall, FFQ – Add – memory strategies (multiple pass, product recognition), prior notification of interview, combining methods – Caregiver interview beneficial • Physical limitations – arthritis, eyesight, etc – Avoid – self-administered tools Special Considerations for Dietary Intake Assessment in OA (cont.) • Altered dentition – Probe for specialized food prep • Chronic illness & specialized diets – May introduce bias (both + & -) • Supplement use Step 2 - Weight Management • Identify and treat the underlying cause, then • Dietary goal 1. Stop the weight loss 2. Plan for weight regain (when appropriate) • • What is reasonable? +250-500 kcal/day or up to 35 kcal/kg Interventions to Improve Intake: Problem- Decreased Volume • Provide favored foods – If sweets, choose more nutrient-dense options: pudding > cookies > hard candies • Increase snacking, but monitor effect on meals • Get creative in masking nutrients to ↑ nutrient density without ↑ing volume – Adding protein powders (whey), fiber supplements, fats/oils to foods and beverages – Cookbooks available for hiding vegetables in meals (targeted to parents) • Diet liberalization – often warranted Problem: Decreasing Ability to Prepare Foods • Keep nonperishable, ready-to-eat foods available • Batch cook and freeze complete meals that can be microwaved (avoid stove reheating if fatigue or cognition is an issue) • Consider enrollment in a community meal provider service (like Meals on Wheels) Problem: Forgetting to Eat or Drink • Provide visual cues – Place foods and beverages in areas where OA will see them – Attach notes with reminders to eat in high-traffic areas • Offer foods regularly • Have OA eat with others (in a controlled setting) Problem: Loss of appetite • Due to ↓ taste and smell acuity or medication side effects – ↑ spices to enhance flavor – Serve foods warm to increase aroma – Cook other foods that smell delicious at mealtimes • Cookies, bread • Due to reduction in PA – ↑ PA • Due to fatigue – Maximize on best meal –typically breakfast – Offer small snacks periodically – Make every food/beverage count Problem: Isolation, Depression, or MCI • Eat with others • Easily distracted – Eat with others so all are performing the same task – Serve meals in a quiet, pleasant, controlled environment – Use plain plates and tablecloths Problem: Dental, Chewing, or Swallowing Issues • Dental eval • Swallowing evaluation – may require medical intervention – Texture-modified foods – Thickened liquids • Dehydration risk • Supplements – an option, offer >1hour apart from meals – consider whole milk with CIB • Supplemental enteral feeding, or full enteral feeding Additional Methods to Ameliorate Weight Loss • Engage social and family support • Increase physical activity • Address fatigue, sleeping issues Management During Illness • Be proactive and aggressive – Weight loss is a downward spiral • Consider it a comorbidity (to primary diagnosis) when developing tx plan Medications and Supplements that May Increase Appetite* Comments Megace Remeron Trazodone Dexamethasone Marinol Metoclopromide Ornithine oxoglutarate (OGO) Do not use – contraindicated for use in OAs Anti-anxiety, anti-nausea Avoid unless for gastroparesis * All except Megace are non-FDA approved for this usage in this population Summary • Involuntary weight loss -15-20% of older adults – Contraindicated in the OA, including the obese • Interventions require a multidisciplinary approach – Begin with identifying the cause – Assess the patient from medical, pharmacological, nutrition, and sociological perspectives – Address weight management plan from multiple avenues Case Study A 73-year-old woman presents to your clinic complaining of unintentional weight loss. She reports having lost 15 lbs (6.8 kg) over the past year. She reports that she is eating three meals per day as usual. The patient’s past medical history is notable for: • Osteoporosis • Left hip fracture three years • Osteoarthritis with osteoarthritic changes in the knees • Hypothyroidism • Hypercholesterolemia. • Radiograph of the chest, CBC, electrolytes, creatinine, TSH, and albumin are WNL. Medications • levothyroxine • a statin • a bisphosphonate • vitamin D and calcium • nonsteroidal anti-inflammatory medications (NSAIDs; prn for knee pain) She is an ex-smoker and does not drink alcohol. Weight -120 lbs (54.5 kg) Usual weight - 135 lbs (61.3 kg) 89% of UBW Body mass index (BMI) - 22.0. Adapted from Alibhai CMAJ 2005 Case Study (cont.) On further questioning, the patient admits that: • Even though she had been eating three meals per day, she eats less at each meal than previously. • Her husband of 50 years died suddenly 10 months ago. – She reports her mood is fine but that she still has not gotten over his death. She feels lonely and is finding it difficult to motivate herself to prepare adequate meals for only one person. • She also reports experiencing nausea and some difficulty chewing over the past month. • You take a closer look in her mouth and notice that her dentures are loose and that there are a few small ulcers on her hard palate. Plan • In an attempt to address her risk factors, you advise her to have her dentures adjusted. Suspecting that the NSAIDS may be contributing to her nausea, you advise her to use acetaminophen for her knee pains instead. At your encouragement, she starts attending grief counseling and becomes involved in social activities, including a supper club, at her local seniors centre. • Over the next two months, her appetite improves and she gains 4#. • Her weight loss appears to have been the result of multiple factors, including social isolation, bereavement, chewing issues, decreased oral intake and possibly the use of NSAIDs. • Risk factor modification appears to have been successful so you do not consider further nutritional or pharmacologic interventions at this time.