Basic Concepts and Compensation
advertisement

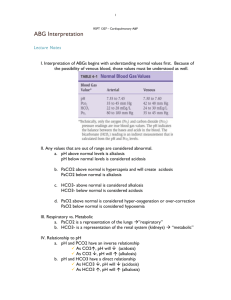
Acid-Base Balance Disorders of acid base balance can be found in as many as 9/10 ICU patients. So we should know how to approach and treat acid-base abnormalities. I will start with basic concepts and build on them. This is a combination of books I used to learn acid-base. Those books are Harrisons Pulmonary and Critical Care Medicine, Pocket Medicine, and The ICU Book. Basic Concepts and Compensation [H+] (nEq/L)= 24 x (PCO2/HCO3) If you use a normal PCO2 of 40 mmHg and a normal HCO3 of 24 mEq/L, the normal [H+] in arterial blood is 40 nEq/L=pH 7.4. Notice that [H+] is expressed in nanoequivalents (nEq) per liter. A nanoequivalent is one-millionth of a milliequivelant, so there are millions more sodium, chloride, and other ions measured in mEq than there are hydrogen ions. Because nanoequivelants represent such a small amount, the [H+] routinely is expressed in pH units, which are derived from taking the negative logarithm of the [H+]. A normal [H+] of 40 nEq/L corresponds to a pH of 7.40. Because the pH is a negative log of the [H+], changes in pH are inversely related to changes in [H+]. So, if you look at the above equation, you can see that the determinants of pH are PCO2 and HCO3. Our body maintains very tight control of pH. Thus, a change in one of the determinants must be met by a proportional change in the other determinant. This is known as the compensatory response. Look at the table below and keep the equation in mind: Primary Acid-Base Disorders and Associated Compensatory Changes [H+]= 24 x PCO2/HCO3 Primary Disorder Respiratory Acidosis Respiratory Alkalosis Metabolic Acidosis Metabolic Alkalosis Primary Change Increased PCO2 Decreased PCO2 Decreased HCO3 Increased HCO3 Compensatory Change Increased HCO3 Decreased HCO3 Decreased PCO2 Increased PCO2 *Please notice that each compensatory change is designed to keep the PCO2/HCO3 ratio constant With these compensatory responses being mentioned, please always remember that a compensatory change is not strong enough to keep the pH constant. They only serve to limit the change in pH that results from a primary change in PCO2 or HCO3. So, with that being said, there is no such term as “OVER/UNDER COMPENSATION”. If the compensatory response is more/less than predicted giving you a normal pH there is a mixed acid-base disorder. The question now is how do we predict the expected compensation? There are 6 well known calculations for this depending on the primary disorder: 1. Metabolic Acidosis Expected PaCO2= (1.5 x HCO3) + 8 (+ 2)= Winters Formula* 2. Metabolic Alkalosis Expected PaCO2= (0.7 x HCO3) + 21 (+ 2) 3. The ones for acute/chronic respiratory acidosis/alkalosis I always have to look up and can be found in the green book on pg 4-1. *Winters formula is used to evaluate the respiratory compensation when analyzing metabolic acidosis. Winters gives an expected value for the patient’s Pco2; the patients actual (measured) Pco2 is then compared to this. If the values correspond, respiratory compensation is adequate. If the measured PCO2 is higher than calculated, you have a concominant respiratory acidosis. If the measured PCO2 is lower than the calculated value, there is also a primary respiratory alkalosis. *All of the compensations can be thought of this way and do not merit explanation Gaps, Gaps, Gap-Gap-Gap-Gaps The only other concept to discuss is if we have a metabolic acidosis, how to calculate the anion gap and the delta gap. The anion gap is calculated for you on the BMP drawn at the hospital. It merely represents the difference between positive ions (Na + K) and negative ions (HCO3 and Cl-). The reason we measure the anion gap is because it is used to determine if a metabolic acidosis is due to an accumulation of non-volatile acids (e.g, lactate, ketones, etc, increased anion gap) or a net loss of bicarbonate (e.g., diarrhea, normal anion gap). I am going to completely explain how we get to the equation for an anion gap. If you’re not interested, just skip over this section. The delta gap is the difference between the change in anion gap and HCO3. This is used to evaluate the possibility of a concominant metabolic alkalosis or non-gap acidosis. See details below. Measuring the Anion Gap Look at the definition for electrical neutrality. Na + UC= (Cl- - HCO3) + UA Where UC is unmeasurable cations and UA is unmeasurable anions (+ charged molecules). To achieve normal balance, the neg. charged anions should equal the concentraion of positively charged cations. This is the case in normal physiology. All ions participate in this balance including those we see (measure) and don’t see. So the anions and cations we don’t see are termed UA and UC, respectively. If you rearrange the eqn. above you get: UA- UC= Na – (Cl- + HCO3) The difference between UA and UC is a measure of the excess unmeasured anions and is called the anion gap (AG). There is usually a difference, or excess of anions, of 12 mEq/L. But since labs are prone to error, we say a normal anion gap is between 8-12. If you consider potassium in the equation the typical difference is 15 mEq/L. Increased AG are always due to the accumulation of some form of unmeasured anion (e.g., lactate, b-hydroxybutyrate, ethanol, etc.). Now, the majority of the difference in the UA and UC is due to albumin concentration. NOTE THAT THE MAJOR UA IS ALBUMIN. STUDIES HAVE SHOWN THAT A 50% REDUCTION IN ALBUMIN LEADS TOA A 75% REDUCTION IN THE ANION GAP!! What does this mean? This means that a pt with metabolic acidosis and hypoalbuminemia will have a falsely low anion gap. So how do we correct for this? It’s a simple calculation that can be written down in the green book: Adjusted AG= Observed AG + 2.5 x [4.5 – measured albumin] If youre wondering why this is important, its strictly due to the fact that we divide metabolic acidosis into 2 categories: normal AG and elevated AG acidosis. Increased AG This is simple: when a fixed acid is added to the extracellular space, the acid dissociates to produce hydrogen ions and anions. The hydrogen combines with HCO3 and according to our equation above, the decreased HCO3 will result in an increased AG. The causes of elevated AG are always due to the addition of an acid! Here is the way I remember it: LA MUDPIE Lactic acid ASA toxicity Methanol ingestion Uremia (CKD or AKI) DKA Propylene glycol Isoniazid, iron, infection Ethylene glycol, ethanol (ethanol actually leads to increase in lactic acid) If the anion gap is elevated, we need to calculate the gap-gap Gap-Gap In the presence of a high AG metabolic acidosis, it is possible to predict another metabolic acid base disorder (a normal AG met acidosis or met alkalosis) by comparing the AG excess (the difference between the measured and normal AG) to the HCO3 deficit (the difference between the measured and normal HCO3 concentration in plasma). The ratio (AG Excess:HCO3 deficit) is shown below using 12 mEq/L as the normal AG and 24 mEq/L as the normal plasma HCO3 concentration: AG Excess/HCO3 deficit= (measured AG -12) / (24 – measured HCO3) This ratio can me used to determine if there is a concominant non gap acidosis or concomininat metabolic alkalosis. Coexisting Anion Gap and Non Anion Gap Metabolic Acidosis If you stop and think about it this makes perfect sense. When a fixed acid accumulates in the ECF (high AG met acidosis) the decrease in the serum bicarbonate is equivelant to the increase in the anion gap. Therefore, the gap-gap should be unity (=1). However, when a non gap acidosis, or hypercholremic acidosis, is present (loosing HCO3 instead of gaining fixed acid) the amount of HCO3 lost is replaced with chloride. Therefore the decrease in HCO3 is greater than the increase in the AG, and the ratio (AG excess/HCO3 deficit) falls below unity (<1). Therefore, in the presence of a high AG acidosis, a “gap-gap” ratio of less than 1 indicated the co-existence of a normal AG metabolic acidosis. What causes a non gap acidosis: just remember too much normal saline, early renal failure, diarrhea, and Renal Tubular Acidosis (RTA). Coexisting Anion Gap Metabolic Acidosis and Alkalosis The opposite is true when alkali is added. When alkali is added in the presence of a high AG acidosis, the decrease in serum bicarb is less than the increase in AG, and the gap:gap ratio is greater than unity (>1). Therefore, a gap-gap greater than 1 indicated the coexistance of a metabolic alkalosis. HERES HOW I APPROACH ACID-BASE PROBLEMS: Step wise approach: Step 1: Identify the primary acid base disorder - If pH and PCO2 change in the same direction=Metabolic - If pH and PCO2 change in the opposite direction=Respiratory - If pH is low acidosis, if pH is high alkalosis - If its respiratory is it acute or chronic, there is no term “Chronic metabolic acidosis or alkalosis” Step 2: Evaluate compensatory response - This requires we get out a book and calculate what the changes in pH (if respiratory) or the changes in PaCO2 (if metabolic) should be. It is very difficult to memorize those numbers so always having the green book is essential. - This will tell you if there is a mixed disorder based on the degree of compensation. - You can never have a concominant respiratory disorder. i.e. You cant have a chronic respiratory acidosis on a chronic respiratory alkalosis. You can have an acute on chronic respiratory pathology. The change in pH and PCO2 will tell you if this is present. Step 3: If metabolic acidosis, use your “Gaps” - Calculate an anion gap and if elevated calculate the gap-gap. Step 4: Name the disorder(s) and fix it Caveats: *If the pH is normal, there is a mixed disorder *Remember that the HCO3 (renal compensatory response) takes hours to start correcting and days to fully correct. So if you get an ABG and do an intervention, if you get another ABG in 1 hour, the HCO3 should not be changed too terrible much.