number of attendees - AIDS Education and Training Centers
advertisement

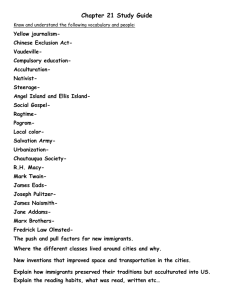
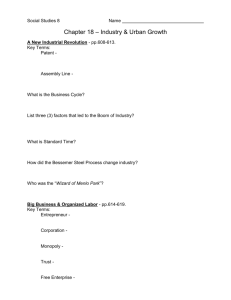
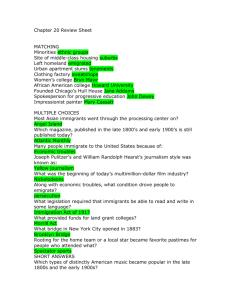
The Impact of HIV in East Africans Living in the United States Meti Duressa, MSW David Lee, MSW, MPH Sponsoring Organizations African American Reach & Teach Health Ministry (AARTH) Northwest AIDS Education & Training Center (NW AETC) PIFs and Evaluation Forms ■ Please complete the Participant Information Form (PIF) which is used to track educational events conducted by AARTH & NW AETC. ■ Funding grants are based upon the type and quantity of educational events and the number of attendees! Learning Objectives ■ ■ ■ Understand how HIV impacts East African Immigrants in King County. Explore cultural differences among East African immigrants. Discuss barriers to care for African immigrants. State and County Census Washington 2000 King County 2005 2000 2005 Population Change (Est.) Ethiopian 5, 966 16,647 +52% 18,693 29,868 +60% Somali 2,486 +71% 2,459 4,231 +72% Kenyan 556 2,010 +262% 380 1,216 +220% 4,261 2000 numbers from Decennial Census 2005 Numbers from American Community Survey King County HIV Statistics US –born Foreign –born No. (%) No. (%) White 3,924 (98) 89 (2) Black 627 (67) 305 (33) Male 503 (75) 167 (25) Female 124 (47) 138 (53) Hispanic 215 (43) 289 (57) Asian/PI 48 (34) 95 (66) NA/AN 78 (95) 4 (5) Other 51 (88) 7 (12) Total 4,943 (86) 789 (14) Public Health Seattle King County, 12/31/2006 Summary of the Data ■ ■ ■ HIV cases increasing among African immigrants but level among African Americans. Most HIV transmission among African immigrants is heterosexual, while most African Americans with HIV are men who have sex with men. About 1.8% of African immigrants are infected, vs. about 1.1% of native-born Blacks. Jim Kent, Public Health Seattle King County Cultural Considerations Religion ■ ■ ■ ■ ■ ■ More than 99% of Somalis are Sunni Moslem. Many Somalis are much more religious now than they were at home before the civil war. Allah’s will determines life and death, health and illness. Prayer is done 5 times a day, wherever you are, preceded by ablutions. Fasting during Ramadan is a tenet of the faith. This alteration of eating schedule needs to be factored into assessment and treatment. Many Somali women in Seattle wear hijab and almost all Somali women in Seattle cover their heads. Health care workers need to support Somalis who wish to maintain modesty. Family ■ ■ ■ ■ ■ Islam allows up to four wives, if a man is able to provide well and justly for four families. Divorce is common in Somalia and here. The US government only allows one wife to immigrate with one husband. Children who emigrated with their father may be living in a family where the woman is not their mother. Family is defined as extended family. Patient Identification ■ ■ ■ ■ Somali names have 3 parts: the first name is the given name, the middle is the father’s surname, and the last is the grandfather’s surname. Back home it was rare to use the last name, but common in the U.S. and a potential source of confusion. Women do not change their last names when they marry. Birthdates are not important in Somalia. Many Somalis were assigned January 1st birthdates when they entered the U.S. Etiquette ■ ■ ■ ■ The right hand is the correct and polite hand to use in daily life (eating, greeting, etc.). Greeting is with a handshake and Salam Alechem, but traditionally hand shakes do not occur across gender. Women hug and kiss (on both sides or on the hand) when they meet each other. It is considered impolite to not ask, “how are you and how is your family?” Dying ■ ■ ■ It is considered uncaring for a physician to tell a patient or their family that they are dying. It is acceptable to describe the extreme seriousness of an illness. A special portion of the Qur’an, Yasin, is read at bedside when a patient is dying. Relationship Building and Communications ■ ■ ■ ■ Time spent establishing a relationship will pay off for the patient and the provider. Somalis are traditionally oral historians and are not prone to brevity. The evil eye and “Mashallah”. A loud and serious tone of voice is not unusual for a Somali speaker and doesn’t necessarily imply anger. Ethiopia ■ ■ ■ There are 80 languages and 200 dialects among Ethiopians. The predominant language among Ethiopians in Seattle is predominantly Amharic, Tigrigna, Oromiffa. The predominant religions are Ethiopian Orthodox, Moslem, Pentecostalism, and Catholicism. Greetings ■ ■ ■ ■ Women, and women & men who know each other, hug and kiss on the cheeks three or four times. Handshakes are exchanged between people who do not know each other. Observant Moslems do not touch across genders. Modesty is highly valued. Eritrea Achieved independence from Ethiopia in 1991 after a protracted armed struggle Religion: Coptic Christian Orthodox, Islam, Catholic, Pentecostal Languages: Tigrigna,Arabic Under Ethiopian rule people were forced to learn/speak Amharic Eritrean Immigration Began in the 70s, peaked in late 80’s and early 90’s Refugees, asylees, before 1991, then as visitors, sponsored by residents, lottery winners Etiquette Greeting: Women and women and men who know each other hug and kiss on the cheeks three or four times. Handshakes are exchanged between people who don’t know each other. Observant Moslems will not touch across genders. Modesty is highly valued. Elders Are held in high regard and are traditionally cared for at home by the family. Death and Dying “In Ethiopia, we have burial societies that operate when there is a death in a neighborhood community. Members of a burial society pitch in money every month for membership. Delivery of news about death is one of the largest issues of difference for the Ethiopian community as compared with other communities. Back home when there is a death, the immediate family usually isn't told right away. An elder is called upon to deliver the news. The Ethiopian CCM explained, "If a death happened in my family back home, my husband or my husband's family would be informed first, and they would tell me at the right time, early in the morning before I left the house." (www.ethnomed.org) Back home, the news of death is orchestrated very carefully. If someone dies late in the day, the news is kept quiet, because there is not enough time left in the day to organize the burial. The announcement of the death is made the next morning when there is enough time for people to prepare for the burial. Sometimes, family members may know of a loved one's death but remain quiet if it happens late in the day, in order to give enough time for people to organize. Burials don't happen after 4:00 PM, so a person who dies later in the day will be buried the next day. A burial may happen on the same day as death when the death happens early in the day. The services may last all night long. When there is a death, the society is responsible for making the announcement and for taking care of all the organizational details of the funeral. In this way, death is a community responsibility. For three days after a death, a family doesn't have to do anything except to mourn. The society members prepare food. Here in the United States, this news-telling tradition is not quite the same. A close friend or family relation, other than an immediate family member, is still told first. Often, this person is an elder. Back home, the family will wash the body. Here, the funeral home washes the body and the family brings the clothing.” (www.ethnomed.org) Pearls Hospitality is offered to visitors. Relationships will be by accepting the offer to drink tea or coffee. Time spent establishing a relationship will pay off. The answer to “ How are you?” will likely be “Thank God, I am fine.” This may not be an accurate statement concerning the patients state of being. A numeric assessment of pain is not usually helpful. What are the barriers to accessing care? Lack of HIV/AIDS Information ■ ■ ■ ■ ■ Prevention v. treatment. Ignorance. Some cannot read. Lack of trust. It cannot happen to me. Women are strong support System for those exposed to HIV/AIDS Responsibility of raising grandchildren for those lost their parents to AIDS Stigma ■ Stigma perpetuates denial and silence. ■ Stigma prevents acknowledgment of problem and care-seeking. ■ Stigma is associated with shame. ■ Stigma prevents dissemination of accurate information. Concerns ■ ■ ■ ■ ■ ■ Fear that prevents them from testing or disclosure. Fear of Stigma. Isolation. Hopelessness. Relationship between men and women (and the cultural context for that relationship). Women’s Rights Issues. • • Rapes occur without legal attention Shame Harmful traditions Female genital circumcision Abduction Forced marriage Underage marriage exposes to HIV/AIDS Respecting Women’s rights one of the consequences of AIDS prevention Immigration Issues ■ Concern that as part of the application they would be required to take an HIV test. • • ■ FALSE for citizenship status If in asylum program… Fear of deportation. • Especially for those who are in the asylum process Western v. Traditional Medicine ■ ■ It differs from culture to culture. It has to be visible to the patient. • • • • • Must have symptoms Weakness Losing weight Unable to work or move To be bed ridden Meanings Related to Having HIV/AIDS ■ ■ ■ ■ Getting Thinner Death Sentence It is a punishment It is unfair • ■ ■ I am not that kind of person Guilt -- it should not happen to me Only one time relationship • • • I only dated one person in my life! Waited long time to have a sexual relationship and this is what happened I am not promiscuous Financial Concerns ■ ■ ■ Will not seek HIV-testing because they believe that they cannot afford it. Some immigrants will not seek medical care or take medications because they that they will not be able to afford it. Sending money back home is a priority and will cause immigrants to neglect their own health needs. Belief of Bad Spirit/Witchcraft ■ ■ ■ ■ I am under a spell-some witchcraft that was done to me. My girlfriend/boyfriend, wife/husband is negative so that means it is a bad spirit or witchcraftwouldn’t my sexual partner have it too? People wanting to make money put this spell/witchcraft on me. Looking for “traditional” medicine; meaning traditional religious cure to exorcise or cure the bad spirit. To Take Meds or Not ■ ■ Once past the original denial they are now ready and eager to take medications as soon as possible Confusion • • • If I have it then give me the medications-do not want to wait, cannot understand the “wait” until the CD4 drops and the Viral Load increases… Undetectable Viral Load vs. Detectable-what does this mean? Either I have it or I do not have it… Important to stress that Undetectable does not mean Cured! Language Issues ■ No providers that speak native tongue. ■ Translators are usually from same community. ■ Medical words do not translate or have different meaning once translated. Confidentiality ■ ■ ■ Given the size of the community people are VERY concerned regarding confidentiality. Avoid as much as possible to be seen at the clinic, especially if they see someone from the same country or their same origin. They suffer due to lack of cultural and or emotional support. Health Care Decisions and Family ■ Some choose to move away from their family to avoid the constant interference on their health care decisions. Examples: • 23 y/o female moved back to home country. 38 y/o female moved to another state. Coping with Illness & Living Well ■ Denial. • ■ Once they get past the denial process and established in care they are very engaged in medical care. Patients gain hope (and weight!) and think of family and of having children once they start feeling well. Strengths Perspective ■ ■ ■ ■ ■ ■ Family Children Future plan Hope Copying skills Religious belief Summary ■ ■ ■ HIV in African Immigrants differs from other groups in King County. Cultural considerations are important for building rapport. There are several barriers that prevent African Immigrants from receiving the care that they need. Resources ■ ■ ■ ■ ■ AARTH 206-850-2070 NW AETC 206-543-3319 Community House Calls 206-744-9256 Ethnomed www.ethnomed.org Madison Clinic 206-744-5100