Slide set 5 - Childhood obesity
advertisement

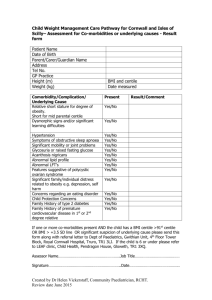
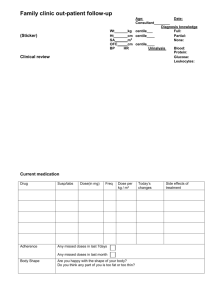
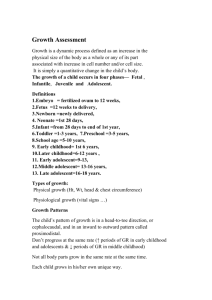
Slide set for Workshop 5 Child obesity challenges and opportunities Acknowledgments R Pryke WORKBOOK PAGES 39 - 47 Workshop 5 Child obesity challenges and opportunities Aims Look at growth charts and how they can be useful in everyday practice • Use BMI look-up table – no calculator required • Interpreting growth through puberty Look at suitable themes to bring into discussion with families Role play and cases – small group work Growth trends shine a light on health Growth is best indicator of health Charts demonstrate normal growth by age and stage of puberty - and in relation to parental height Identify disorders of growth Assess obesity Isolated readings of weight height or BMI are inadequate – they must relate to the appropriate age/sex reference ranges which change throughout childhood RCPCH UK 2-18 Growth chart Parent height comparator UK90 reference after age 4 Mid parental centile scale WHO standards until age 4 Birth centiles Predicted adult height scale Breast-fed baby population trends WHO produced charts that set breastfeeding as the norm and described optimal rather than average growth, that can be used worldwide. Swap over from ‘breast-fed baby’ charts to UK90 chart at age 4. (note the centile lines alter slightly at age 4) There is a wider weight range in breast fed baby populations indicating that lower weight ranges can be normal Body Mass Index (BMI) lookup • Read weight and height centiles from the growth chart. • Plot weight centile (left axis) against the height centile (bottom axis) • Read off the corresponding BMI centile from the slanting lines • Record centile on grid at top of chart • Accurate to ¼ centile space BMI = 91st centile BMI Interpretation A child whose weight is average for their height will have a BMI between the 25th and 75th centiles ‘Growth’ continues into early 20s e.g. bone and muscle mass. Caution re restrictive dieting For children yet to reach adult height:‘Growing into one’s weight’ means slowing down the rate of weight gain whilst further increase in height helps to normalise BMI Children at full height will require weight loss in order for BMI to normalise BMI centile grid: plotting example >91st centile suggests overweight >98th centile is very overweight (clinically obese) Pre-puberty ONLY Puberty starting before 8♀or 9 ♂ is precocious Growth during Puberty Plotting pubertal children on the UK 2-18 Growth charts The 3 Phases of Puberty: from history Girls Pre-puberty (Tanner stage 1) In Puberty (Tanner stage 2-3) Completing Puberty (Tanner stage 4-5) If all of the following: No signs of pubertal If any of the following: Any breast enlargement pubic or axillary hair If all of the following Started periods with signs of pubertal development If any of the following: Slight deepening of the voice Early pubic or axillary hair growth Enlargement of testes or penis If any of the following: Voice fully broken Facial hair Adult size of penis with pubic and axillary hair development Boys If all of the following: High voice and No signs of pubertal development Talking child obesity It’s not only puppy fat... ‘Growing out’ of a weight problem requires altering ‘energy in/out’ balance Advising ‘eat less and exercise more’ should work - but it doesn’t… Avoid simplistic advice Obesity does not mean gluttony:- A small but prolonged energy imbalance can lead to obesity Tools required Time Rapport Entry point into the conversation …NCMP letter? Method for data recording on GP systems that relates to UK/WHO reference ranges – note the centiles Guidance on what to say in a short consultation Promote positives - 'do's' rather than 'don'ts’ Focus on families not individuals - Encourage parents and carers to model a healthy lifestyle Explore feelings to test water non-judgmentally Test kids on what they already know - build on this Relate lifestyle to a variety of health factors dental care, fitness, bone and muscle strength, not just weight Teach concepts Eat together as whole family - siblings and friends influence food preferences too ‘Do as I do rather than Do as I say’ - Children gradually learn to copy parent behaviours – diet and activity Manage expectation of energy dense foods – ‘save for special times’ Reduce sugary drinks and increase consumption of water and milk Developing a ‘taste’ – varied diet Children learn to accept new foods by repeated exposure and seeing others enjoy them It may take many calm exposures to a new food for it to become ‘normal’ – food we eat and choose without giving much thought Never force food – it creates strong dislikes and behaviour battles. Why do so many children dislike ‘greens!’ Use unusual settings, games and appealing presentation to generate positive associations Tuning in to appetite Abandon ‘clear your plate’ concept – it teaches children to ignore appetite signals and risks eating whatever portion is served or simply to please others. Parent guides – child decides Involve children in choosing appropriate portion size – they know best how hungry they are and need practice choosing right amount Think of ‘portions’ as handfuls – little hands, little portions Screen time Avoiding being sedentary (reducing screen time) is strongly linked to preventing obesity – due to both the relation to activity and to exposure to advertising 4 hours a day screen time doubles the risk of overweight cf <1 hour Having a TV in the bedroom is linked with overweight in young children Workshop 5 Cases – p 39 Divide into small groups 1. Plot the height and weight centile examples then use the BMI Look up chart 2. Using ‘Bea’ as a case for role play, explain the concept ‘growing into one’s weight’ to Bea’s parent Choose a case Try the opening few sentences as role play to test out how phrases can come across. Discuss the other questions as a group Resources • Growth charts http://www.rcpch.ac.uk/childhealth/research-projects/uk-who-growthcharts/uk-who-growth-chart-faqs/uk-whogrowth-chart-faq • Tackling obesity through the Healthy Child Programme http://www.noo.org.uk/Mary_Rudolf