HISTORY TAKING AND CNS EXAMINATION

Neurological History Taking and Physical Examination
Dr. M. A. Sofi MD; FRCP (London);
FRCPEdin; FRCSEdin
Neurological History: Taking the patient's history is traditionally the first step in virtually every clinical encounter.
• The history of the presenting illness or chief complaint should include the following:
• Symptom onset (eg, acute, subacute, chronic, insidious)
• Duration
• Course of the condition (eg, static, progressive, or relapsing and remitting)
• Associated symptoms, such as pain, headache, nausea, vomiting, vertigo, numbness, weakness, and seizures
Pain should be further defined:
• Location (Ask the patient to point with one finger, if possible.)
• Radiation (Pay attention to any dermatomal relationship.)
• Quality (stabbing, stinging, lightning like, pounding, etc)
• Severity or quantity
• Precipitating factors (stress, periods, allergens, sleep deprivation, etc)
• Relieving factors (sleep, stress management, etc)
• Diurnal or seasonal variation
Fainting
Also called syncope, is a sudden, brief loss of consciousness and posture caused by decreased blood flow to the brain.
Fainting can be triggered by a number of factors, including:
• Fear or other emotional trauma.
• Severe pain.
• A sudden drop in blood pressure.
• Low blood sugar due to diabetes or from going too long without eating.
• Hyperventilation (rapid, shallow breathing)
• Dehydration.
• Standing in one position for too long.
A seizure
Also known as a fit, is caused by a disturbance in the electrical activity of the brain, which can be due to conditions such as epilepsy. There are 2 main types of seizure:
I.
Generalised seizures involve both sides of the brain from the start of the attack. Common subtypes include
• Tonic-clonic and
• Absence seizures.
II. Partial (or focal) seizures begin in a specific area of the brain and may be contained there. Or they may spread to the entire brain.
• Simple partial seizures, the person remains conscious.
• Complex partial seizures involve impaired consciousness
S
S
M
E
S
E
A
S
N
T
O
P
I
A
P
L
D
I
Ataxia is a neurological sign consisting of lack of voluntary coordination of muscle movements that includes gait abnormality.
1.
Types
Cerebellar
Sensory
Vestibular
2.
Causes
Focal lesions
Exogenous substances
(metabolic ataxia)
Radiation poisoning
Vitamin B
12 deficiency
Hypothyroidism
Causes of isolated sensory ataxia
Non-hereditary cerebellar degeneration
Hereditary ataxias
Arnold-Chiari malformation (congenital ataxia)
Wilson's disease
Gluten ataxia
Sodium-potassium pump
Steps in the neurologic examination
In examining a patient, abnormalities of function lead to localization and, eventually, to the pathophysiology.
These steps include the following:
I.
General Appearance, including posture, motor activity, vital signs and perhaps meningeal signs if indicated.
II. Mini Mental Status Exam, including speech observation.
III. Cranial Nerves, I through XII.
IV. Motor System, including muscle atrophy, tone and power.
V. Sensory System, including vibration, position, pin prick, temperature, light touch and higher sensory functions.
VI. Reflexes, including deep tendon reflexes, clonus,
Hoffman'sresponse and plantar reflex.
VII.Coordination, gait and Rhomberg's Test
Examining the comatose patient
Examination of the Higher Functions
Components of Higher Functions
• Higher functions include gait, speech, and mental status.
• Gait is the attitude of a person in the upright position. Abnormal types are described below.
• Hemiparetic gait: The shoulder is adducted; the elbow is flexed; the forearm is pronated, and the wrist and fingers are flexed.
• Ataxic gait: Patient spreads his or her legs apart to widen the base of support to compensate for the imbalance while standing or walking
• The heel-to-toe or tandem walking maneuvers and standing on 1 leg uncover subtle forms of ataxia
• Shuffling gait: The individual takes short steps and appears to shuffle his or her legs rather than put them forward.
• Steppage gait: Individual takes high steps as if climbing a flight of stairs while walking on a level surface.
• Spastic or scissor gait: The legs are held in adduction at the hip and the thighs rub against each other as the patient walks.
• Antalgic gait: Patient favors the affected painful (usually lower) extremity and walks, putting weight on the normal leg. The hand held over hip on the affected side is typical in patients with radicular pain.
Examination of the Higher Functions
Speech
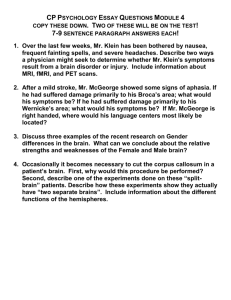
• Speech is communication between individuals. Abnormalities include dysphonia, dysarthria, and dysphasia or aphasia.
Dysphonia or aphonia
• Dysphonia is the impairment or inability to phonate. The voice becomes hoarse. In extreme cases, it is absent, and the patient is mute.
Dysarthria or anarthria
• Dysarthria is the inability to articulate spoken words. The quality of oration is impaired, but the content remains intact (e.g., slurred speech).
• Ability to understand and synthesize speech remains intact.
Dysphasia or aphasia: In dysphasia, the ability to process language is impaired, resulting in
• Inability to understand or comprehend Wernicke aphasia
• Transfer signals from the
Wernicke to the Broca area conduction aphasia
• Properly execute speech
expressive, motor, or Broca
aphasia).
• The combination of Broca and
Wernicke aphasias is referred to as global aphasia.
Essential Features of Common Dysphasias
Type of
Dysplasia
Broca
Wernicke
Fluency
Non-fluent Intact
Fluent Impaired
Conduction Fluent
Comprehension Naming
Intact
Impaired
Impaired
Impaired
Global Nonfluent Impaired Impaired
Localization
Broca area
Wernicke area
Arcuate fasciculus
Broca and
Wernicke areas
Category
Orientation to time
Orientation to place
Registration
Mini–mental state examination
Possible points
Description
5
From broadest to most narrow. Orientation to time has been correlated with future decline.
5
3
From broadest to most narrow. This is sometimes narrowed down to streets, and sometimes to floor.
Repeating named prompts
Attention and calculation
Recall
Language
Repetition
5
3
1
2
Serial sevens, or spelling "world" backwards. It is more appropriate in a population where English is not the first language.
Registration recall
Naming a pencil and a watch
Speaking back a phrase
Complex commands 6 Varies. Can involve drawing figure shown
Total score
Category
Cranial nerve examination
Motor system
Tests
Example of writeup
Cranial nerves (I-XII): sense of smell (I), visual fields and acuity (II), eye movements
(III, IV, VI) and pupils (III, sympathetic and parasympathetic), sensory function of face
(V), strength of facial (VII) and shoulder girdle muscles (XI), hearing (VII, VIII), taste
(VII, IX, X), pharyngeal movement and reflex (IX, X), tongue movements (XII). These are tested by their individual purposes (e.g. the visual acuity can be tested by a
Snellen chart
• Muscle strength, often graded on the MRC scale 0 to 5 (i.e., 0 = Complete Paralysis to 5 = Normal Power).
• grades 4−, 4 and 4+ maybe used to indicate movement against slight, moderate and strong resistance respectively.
• Muscle tone and signs of rigidity.
• Examination of posture
• Decerebrate
• Decorticate
• Hemiparetic
• Resting tremors
• Abnormal movements
• Seizure
• Fasciculations
• Tone
• Spasticity
• Pronator drift
• Rigidity
• Cogwheeling (abnormal tone suggestive of Parkinson's disease)
• Gegenhalten – is resistance to passive change, where the strength of antagonist muscles increases with increasing examiner force. More common in dementia
CNII-XII grossly intact
"strength 5/5 throughout, tone
WNL"
Category
Deep tendon reflexes
Sensation
Cerebellum
Tests
Example of writeup
Reflexes: masseter, biceps and triceps tendon, knee tendon, ankle jerk and plantar
(i.e., Babinski sign). Globally, brisk reflexes suggest an abnormality of the UMN or pyramidal tract, while decreased reflexes suggest abnormality in the anterior horn,
LMN, nerve or motor end plate A reflex hammer is used for this testing.
Sensory system testing involves provoking sensations of fine touch, pain and temperature. Fine touch can be evaluated with a monofilament test, touching various dermatomes with a nylon monofilament to detect any subjective absence of touch perception.
• Sensory
• Light touch
• Pain
• Temperature
• Vibration
• Position sense
• Graphesthesia
• Stereognosis, and
• Two-point discrimination (for discriminative sense)
• Extinction
• Romberg test – 2 out of the following 3 must be intact to maintain balance: i. vision ii. vestibulocochlear system iii. epicritic sensation
• Cerebellar testing
• Dysmetria Dysdiadochokinesis
• Finger-to-nose test Rapid pronation-supination
• Ankle-over-tibia test
• Ataxia
• Assessment of gait
• Nystagmus
• Intention tremor
• Staccato speech
"2+ symmetric, downgoing plantar reflex"
"intact to sharp and dull throughout
"intact finger-tonose, gait WNL
Interpretation
The results of the examination are taken together to anatomically identify the lesion. This may be diffuse (e.g., neuromuscular diseases, encephalopathy) or highly specific (e.g., abnormal sensation in one dermatome due to compression of a specific spinal nerve by a tumor deposit).
General principles
• Looking for side to side symmetry:
• Determining if there is focal asymmetry.
Determining whether the
process involves:
• (PNS),(CNS), or both.
• If the finding can be explained by a single lesion or whether it requires a multifocal process.
Lesion's location.
• If the process involves the CNS, clarifying if it is cortical, subcortical, or multifocal.
•
• Subcortical, clarifying whether it is white matter, basal ganglia, brainstem, or spinal cord.
• PNS then determining whether it localizes to the nerve root, plexus, peripheral nerve, neuromuscular junction, muscle or whether it is multifocal.
Differential diagnosis may then be constructed that takes into account the patient's background
Muscles and Spinal Roots
Muscle
Biceps
Brachioradialis
Triceps
Patellar
Achilles
Muscle
Spinal Roots
C5, 6
C6
C7
L2-4
S1
Spinal Roots
4
5
Reflex-Grading System
1
2
Score Reflexes
0 Absent
3
Hypoactive or present only with reinforcement
Readily elicited with a normal response
Brisk with or without evidence of spread to the neighboring roots
Associated with a few beats of unsustained clonus
Sustained clonus
1
4
5
2
3
Muscle-Strength Scale
Score
0
Description
Absent voluntary contraction
Feeble contractions that are unable to move a joint
Movement with gravity eliminated
Movement against gravity
Movement against partial resistance
Full strength