Clinical Pharmacokinetics and Pharmacodynamics
advertisement

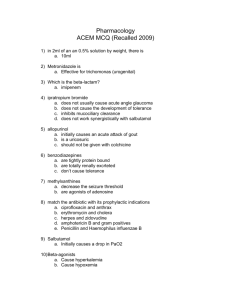
Clinical Pharmacokinetics and Pharmacodynamics Janice E. Sullivan, M.D. Brian Yarberry, Pharm.D. Why Study Pharmacokinetics (PK) and Pharmacodynamics (PD)? • Individualize patient drug therapy • Monitor medications with a narrow therapeutic index • Decrease the risk of adverse effects while maximizing pharmacologic response of medications • Evaluate PK/PD as a diagnostic tool for underlying disease states Clinical Pharmacokinetics • The science of the rate of movement of drugs within biological systems, as affected by the absorption, distribution, metabolism, and elimination of medications Absorption • Must be able to get medications into the patient’s body • Drug characteristics that affect absorption: – Molecular weight, ionization, solubility, & formulation • Factors affecting drug absorption related to patients: – Route of administration, gastric pH, contents of GI tract Absorption in the Pediatric Patient • • • • • • Gastrointestinal pH changes Gastric emptying Gastric enzymes Bile acids & biliary function Gastrointestinal flora Formula/food interaction concentration Time to Peak Concentration 100 90 80 70 60 50 40 30 20 10 0 IV Oral Rectal 0 5 10 20 30 minutes 60 120 180 Distribution • Membrane permeability – cross membranes to site of action • Plasma protein binding – bound drugs do not cross membranes – malnutrition = albumin = free drug • Lipophilicity of drug – lipophilic drugs accumulate in adipose tissue • Volume of distribution Pediatric Distribution • Body Composition – total body water & extracellular fluid – adipose tissue & skeletal muscle • Protein Binding – albumin, bilirubin, 1-acid glycoprotein • Tissue Binding – compositional changes Metabolism • Drugs and toxins are seen as foreign to patients bodies • Drugs can undergo metabolism in the lungs, blood, and liver • Body works to convert drugs to less active forms and increase water solubility to enhance elimination Metabolism • Liver - primary route of drug metabolism • Liver may be used to convert pro-drugs (inactive) to an active state • Types of reactions – Phase I (Cytochrome P450 system) – Phase II Phase I reactions • Cytochrome P450 system • Located within the endoplasmic reticulum of hepatocytes • Through electron transport chain, a drug bound to the CYP450 system undergoes oxidation or reduction • Enzyme induction • Drug interactions Phase I reactions types • • • • • • Hydrolysis Oxidation Reduction Demethylation Methylation Alcohol dehydrogenase metabolism Phase II reactions • Polar group is conjugated to the drug • Results in increased polarity of the drug • Types of reactions – Glycine conjugation – Glucuronide conjugation – Sulfate conjugation Elimination • Pulmonary = expired in the air • Bile = excreted in feces – enterohepatic circulation • Renal – glomerular filtration – tubular reabsorption – tubular secretion Pediatric Elimination • Glomerular filtration matures in relation to age, adult values reached by 3 yrs of age • Neonate = decreased renal blood flow, glomerular filtration, & tubular function yields prolonged elimination of medications • Aminoglycosides, cephalosporins, penicillins = longer dosing interval Pharmacokinetic Principles • Steady State: the amount of drug administered is equal to the amount of drug eliminated within one dosing interval resulting in a plateau or constant serum drug level • Drugs with short half-life reach steady state rapidly; drugs with long half-life take days to weeks to reach steady state Steady State Pharmacokinetics • Half-life = time required for serum plasma concentrations to decrease by onehalf (50%) • 4-5 half-lives to reach steady state 100 90 80 70 % 60 steady 50 state 40 30 20 10 0 1 2 3 Half-life 4 5 Loading Doses • Loading doses allow rapid achievement of therapeutic serum levels • Same loading dose used regardless of metabolism/elimination dysfunction 40 35 30 25 20 15 10 5 0 w/ bolus w/o bolus Linear Pharmacokinetics 120 100 concentration • Linear = rate of elimination is proportional to amount of drug present • Dosage increases result in proportional increase in plasma drug levels 80 60 40 20 0 dose • Nonlinear = rate of elimination is constant regardless of amount of drug present • Dosage increases saturate binding sites and result in nonproportional increase/decrease in drug levels concentration Nonlinear Pharmacokinetics 50 45 40 35 30 25 20 15 10 5 0 dose Michaelis-Menten Kinetics 30 concentration • Follows linear kinetics until enzymes become saturated • Enzymes responsible for metabolism /elimination become saturated resulting in non-proportional increase in drug levels 25 20 15 10 5 0 dose phenytoin Special Patient Populations • Renal Disease: same hepatic metabolism, same/increased volume of distribution and prolonged elimination dosing interval • Hepatic Disease: same renal elimination, same/increased volume of distribution, slower rate of enzyme metabolism dosage, dosing interval • Cystic Fibrosis Patients: increased metabolism/ elimination, and larger volume of distribution dosage, dosage interval Pharmacogenetics • Science of assessing genetically determined variations in patients and the resulting affect on drug pharmacokinetics and pharmacodynamics • Useful to identify therapeutic failures and unanticipated toxicity Pharmacodynamics • Study of the biochemical and physiologic processes underlying drug action – Mechanism of drug action • Drug-receptor interaction – Efficacy – Safety profile Pharmacodynamics • “What the drug does to the body” – Cellular level – General Pharmacodynamics Cellular Level Drug Actions • Most drugs bind to cellular receptors – Initiate biochemical reactions – Pharmacological effect is due to the alteration of an intrinsic physiologic process and not the creation of a new process Drug Receptors • Proteins or glycoproteins – Present on cell surface, on an organelle within the cell, or in the cytoplasm – Finite number of receptors in a given cell • Receptor mediated responses plateau upon saturation of all receptors Drug Receptors • Action occurs when drug binds to receptor and this action may be: – Ion channel is opened or closed – Second messenger is activated • cAMP, cGMP, Ca++, inositol phosphates, etc. • Initiates a series of chemical reactions – Normal cellular function is physically inhibited – Cellular function is “turned on” Drug Receptor • Affinity – Refers to the strength of binding between a drug and receptor – Number of occupied receptors is a function of a balance between bound and free drug Drug Receptor • Dissociation constant (KD) – Measure of a drug’s affinity for a given receptor – Defined as the concentration of drug required in solution to achieve 50% occupancy of its receptors Drug Receptors • Agonist – Drugs which alter the physiology of a cell by binding to plasma membrane or intracellular receptors • Partial agonist – A drug which does not produce maximal effect even when all of the receptors are occupied Drug Receptors • Antagonists – Inhibit or block responses caused by agonists • Competitive antagonist – Competes with an agonist for receptors – High doses of an agonist can generally overcome antagonist Drug Receptors • Noncompetitive antagonist – Binds to a site other than the agonist-binding domain – Induces a conformation change in the receptor such that the agonist no longer “recognizes” the agonist binding site. – High doses of an agonist do not overcome the antagonist in this situation Drug Receptors • Irreversible Antagonist – Bind permanently to the receptor binding site therefore they can not be overcome with agonist Pharmacodynamics Definitions Definitions • Efficacy – Degree to which a drug is able to produce the desired response • Potency – Amount of drug required to produce 50% of the maximal response the drug is capable of inducing – Used to compare compounds within classes of drugs Definitions • Effective Concentration 50% (ED50) – Concentration of the drug which induces a specified clinical effect in 50% of subjects • Lethal Dose 50% (LD50) – Concentration of the drug which induces death in 50% of subjects Definitions • Therapeutic Index – Measure of the safety of a drug – Calculation: LD50/ED50 • Margin of Safety – Margin between the therapeutic and lethal doses of a drug Dose-Response Relationship • Drug induced responses are not an “all or none” phenomenon • Increase in dose may: – Increase therapeutic response – Increase risk of toxicity Clinical Practice What must one consider when one is prescribing drugs to a critically ill infant or child??? Clinical Practice • Select appropriate drug for clinical indication • Select appropriate dose – Consider pathophysiologic processes in patient such as hepatic or renal dysfunction – Consider developmental and maturational changes in organ systems and the subsequent effect on PK and PD Clinical Practice • Select appropriate formulation and route of administration • Determine anticipated length of therapy • Monitor for efficacy and toxicity • Pharmacogenetics – Will play a larger role in the future Clinical Practice • Other factors – Drug-drug interaction • • • • • Altered absorption Inhibition of metabolism Enhanced metabolism Protein binding competition Altered excretion Clinical Practice • Other factors (con’t) – Drug-food interaction • NG or NJ feeds – Continuous vs. intermittent – Site of optimal drug absorption in GI tract must be considered Effect of Disease on Drug Disposition • Absorption – PO/NG administered drugs may have altered absorption due to: • • • • • • Alterations in pH Edema of GI mucosa Delayed or enhanced gastric emptying Alterations in blood flow Presence of an ileus Coadministration with formulas (I.e. Phenytoin) Effect of Disease on Drug Disposition • Drug distribution may be affected: – Altered organ perfusion due to hemodynamic changes • May effect delivery to site of action, site of metabolism and site of elimination • Inflammation and changes in capillary permeability may enhance delivery of drug to a site – Hypoxemia affecting organ function • Altered hepatic function and drug metabolism Effect of Disease on Drug Disposition – Alterations in protein synthesis • If serum albumin and other protein levels are low, there is altered Vd of free fraction of drugs that typically are highly protein bound therefore a higher free concentration of drug – Substrate deficiencies • Exhaustion of stores • Metabolic stress Effect of Disease on PD • Up regulation of receptors • Down regulation of receptors – Decreased number of drug receptors • Altered endogenous production of a substance may affect the receptors Effect of Disease on PD • Altered response due to: – – – – Acid-base status Electrolyte abnormalities Altered intravascular volume Tolerance Management of Drug Therapy • “Target-effect” strategy – Pre-determined efficacy endpoint – Titrate drug to desired effect • Monitor for efficacy – If plateau occurs, may need to add additional drug or choose alternative agent • Monitor for toxicity – May require decrease in dose or alternative agent Management of Drug Therapy • “Target-concentration” strategy – Pre-determined concentration goal • Based on population-based PK • Target concentration based on efficacy or toxicity – Know the PK of the drug you are prescribing • Presence of an active metabolite? • Should the level of the active metabolite be measured? • Zero-order or first-order kinetics? – Does it change with increasing serum concentrations? Management of Drug Therapy – Critical aspects of “target-concentration” therapy • Know indications for monitoring serum concentrations – AND when you do not need to monitor levels • Know the appropriate time to measure the concentration • If the serum concentration is low, know how to safely achieve the desired level • Be sure the level is not drawn from the same line in which the drug is administered • Be sure drug is administered over the appropriate time • AND Treat the patient, not the drug level REMEMBER No drug produces a single effect!!! Case #1 JB is a 5 y.o. male with pneumonia. He has a history of renal insufficiency and is followed by the nephrology service. His sputum gram stain from an ETT shows gram negative rods. He needs to be started on an aminoglycoside. Currently, his BUN/SCr are 39/1.5 mg/dL with a urine output of 0.4 cc/kg/hr. You should: a) b) c) d) Start with a normal dose and interval for age Give a normal dose with an extended interval Give a lower dose and keep the interval normal for age Aminoglycosides are contraindicated in renal insufficiency Case #2 MJ is a 3 y.o. female with a history of congenital heart disease. She is maintained on digoxin 10 mcg/kg/day divided bid. She has a dysrhythmia and is started on amiodarone. You should: a) Continue digoxin at the current dose b) c) d) Decrease the digoxin dose by 50% and monitor levels Increase the digoxin dose by 50% and monitor levels Discontinue the digoxin Case #3 AC is a 4 y.o male on a midazolam infusion for sedation in the PICU. He is currently maintained on 0.4 mg/kg/hr. You evaluate the child and notice that he is increasingly agitated. You should: a) Increase the infusion to 0.5 mg/kg/hr b) Bolus with 0.1 mg/kg and increase the infusion to 0.5 mg/kg/hr Bolus with 0.4 mg/kg and increase the infusion to 0.5 mg/kg/hr Bolus with 0.1 mg/kg and maintain the infusion at 0.4 mg/kg/hr c) d) Case #4 JD is a 10 y.o. child on phenytoin NG bid (10 mg/kg/day) for post-traumatic seizures but continues to have seizures. He is on continuous NG feeds. His phenytoin level is 6 mcg/ml. You should: a) b) c) d) Increase his phenytoin dose to 12 mg/kg/day divided bid Load him with phenytoin 5 mg/kg and increase his dose to 12 mg/kg/day Change his feeds so they are held 1 hr before and 2 hrs after each dose, give him a loading dose of 10 mg/kg, continue his current dose of 10 mg/kg/day and recheck a level in 2 days (sooner if seizures persist). Add another anticonvulsant Case #5 LF is a 12 y.o. with sepsis and a serum albumin of 1.2 mg/dL. She has a seizure disorder which has been well controlled with phenytoin (serum concentration on admission was 19 mcg/ml). You notice she is having clonus and seizure-like activity. You should: a) Administer phenytoin 5 mg/kg IV now b) c) d) Order a serum phenytoin level now Obtain an EEG now Order a total and free serum phenytoin level now Case #6 KD is a 12 y.o. child admitted with status asthmaticus who is treated by her primary physician with theophylline (serum concentration is 18 mcg/ml). Based on her CXR and clinical findings, you treat her with erythromycin for presumed Mycoplasma pneumoniae. You should: a) b) c) d) Continue her current dose of theophylline. There is no need to monitor serum concentrations. Lower her dose of theophylline and monitor daily serum concentrations Increase her dose of theophylline by 10% and monitor daily serum concentration Continue her current dose of theophylline and monitor daily serum concentrations Case #7 BJ is a 13 y.o. S/P BMT for ALL. She is admitted to the PICU in septic shock. She has renal insufficiency with a BUN/SCr of 45/2.1 mg/dL and is on fluconazole, cyclosporine, solumedrol, vancomycin, cefepime and acyclovir in addition to vasopressors. a) Identify the drugs which may worsen her renal function b) Identify the drugs which require dosage adjustment due to her renal dysfunction Identify the drugs which require serum concentrations to be monitored and project when you would obtain these levels c)