File
advertisement

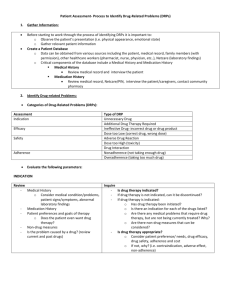
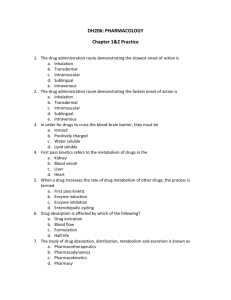
Learning Objective: Pharmacology 1. Outline the factors that influence the mechanisms of drug action In the majority of cases, drug work by interacting with specific molecules involved with regulatory functions (i.e. they interact/bind with receptors or active sites on a specific enzyme). Specificity of the binding site (target) and the drug is reciprocal – individual classes of drugs bind only with certain targets and individual targets recognise only certain classes of drugs. The major influencing factors on the mechanisms for drug action are; Affinity: The tendency of a drug to bind to the receptors Efficacy: the tendency of the drug to activate the receptor (once bound) Therefore Agonists would have a high efficacy, whilst antagonists should have an efficacy of 0. To a much lesser extend, drugs can also work in the following ways; Interaction as a chemical antagonist directly with other drugs (i.e. chelating agents) Interaction with water molecules (i.e. osmotic diuretics) 2. Outline the characteristics of dose-response relationship Dose-response curves are plotted to track the biological response of a subject by dose of a drug administered. For example, this could include a rise in blood pressure, contraction or relaxation of a strip of smooth muscle, or the activation of an enzyme. Concentration-effect or dose-response curves are often plotted in order to estimate maximal response a drug can produce (Emax) and the concentration or dose needed to produce 50% of the maximal response (EC50 or ED50). Binding can be measured directly, however, this is a more common method of charting a drugs binding effectiveness. These parameters are useful for comparing the potencies of different drugs that produce similar effects. An example of a comparative Dose-Response Curve: Drug X has greater biologic activity per dosing equivalent and is thus more potent than drug Y or Z. Drugs X and Z have equal efficacy, indicated by their maximal attainable response (ceiling effect). Drug Y is more potent than drug Z, but its maximal efficacy is lower. N.B. there is no justification that the more potent of the two drugs is clinically superior – toxicity of drugs must also be taken into account. 3. Understand the concepts of drug toxicity including therapeutic index Therapeutic Index is designed to indicate a margin of safety for the use of a drug. It takes into account the minimum effective dose and the maximum tolerated dose (or lethal dose) of a drug. However, in order to recognise that individuals may vary widely in their tolerance for a drug, it works on calculating the median of each of these values to work out the drugs relative safety. Therefore, the definition of the Therapeutic Index is as follows; Therapeutic Index = LD50/ED50 (LD = Lethal Dose, ED = Effective Dose) Therefore, the greater the ratio between LD50 and ED50, the safer the drug. Drugs must be >1.0 to be a therapeutic agent, whilst <2.0 is typically a toxic substance at the therapeutic dose. The limitations of the therapeutic index are; LD50 does not reflect toxicity and unwanted side effects that do not lead to death ED50 is often not definable as it would depend on what measure of effectiveness is used. For example, would the effectiveness of aspirin be measured according to its affect on a mild headache or as its use as an antirheumatic drug? Neither of the terms take into account individual attributes –for example, some relatively “harmless” drugs would be extremely toxic for an asthmatic. 4. Understand the terms agonist and antagonist in relation to pharmacodynamics Pharmacodynamics: the study of how a drug acts on a living organism, including the pharmacologic response and the duration and magnitude of response observed relative to the concentration of the drug at an active site in the organism, (Mosby’s Dictionary of Medicine, Nursing & Health Professionals) There are two main types of drug classifications in terms of its activation (or lack of) of the drug receptors; o Agonist: activate the ‘receptor’ and elicits a biological effect. The magnitude of the effect will depend on the number of receptors occupies and/or rate of formation of the drug/receptor complexes o Antagonist: May combine at the same site without causing activation and thereby blocks (or reverses) the effect of an agonist on that receptor Therefore Agonists would have a high efficacy (as they are initiating a chain of reactions), whilst antagonists should have an efficacy of 0. Others: Partial Agonist: can produce only a submaximal response, even at 100% occupancy of the receptors Spare Receptors: This just indicates that the pool of receptors is larger than the number needed to evoke a full response and that a given number of agonistreceptor complexes, corresponding to a given level of biological response, can be reached with a lower concentration of hormone or neurotransmitter than would be the case if fewer receptors were provided economy of hormone or transmitter secretion is therefore achieved at the expense of providing more receptors Constitutive Activation: activation in the absence of any ligand (can be in a disease state or experimentally created) Inverse Agonist: a drug capable of reducing the constitutive activation (have negative efficacy)