Mechanism of action - Nursing Pharmacology
advertisement

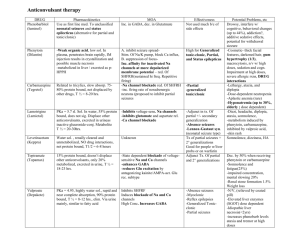
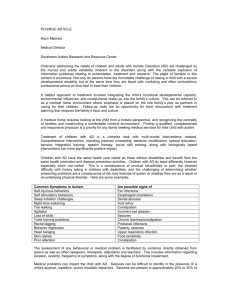
15 Drugs for Seizures Chapter 15 (“analeptics”) OVERVIEW: Neuro System Opioids Salicylates NSAIDs Non-Opioid Antidepressant / Anxiolytic Benzodiazepines lorazepam (Ativan) diazepam (Valium) GABA A Antagonist zolpidem (Ambien) aspirin (ASA) ibuprofen (Motrin) acetaminophen (Tylenol) tramadol (Ultram) Anti-Migraine ergotamine (Cafergot) Sumatriptan (Imitrex) escitalopram (Lexapro) MAOIs morphine (Infumorph) Central Acting Tri-Cyclic Antidepressa nt Opioid Antagonists naloxone (Narcan) Phenytoin-Like Drugs phenytoin (Dilantin) valproic acid (Depakote) Succinimides ethosuximide (Zarontin) Barbiturates phenobarbital (Luminal) Phenothiazines chlorpromazine (Thorazine) NonPhenothiazines halperidol (Haldol) Atypical Antipsychotics risperidone (Risperdal) Learning Outcomes • 1. Describe the nurse’s role in the pharmacologic management of seizures of an acute nature and epilepsy. • 2. Categorize drugs used in the treatment of seizures based on their classification and mechanism of action. • 3. Use the nursing process to care for patients receiving drug therapy for epilepsy and seizures. • 4. For each of the drug classes, know representative drug examples and explain their mechanism of drug action, primary actions, and important adverse effects. Anti-seizure Pharmacotherapy • Goal: suppress neuronal activity enough to prevent abnormal or repetitive firing • Drugs act through three mechanisms: • Stimulating an influx of chloride ions • Delaying an influx of sodium • Delaying an influx of calcium • Directed at controlling movement of electrolytes across neuronal membranes or affecting neurotransmitter balance • Some drugs act by more than one mechanism Pharmacotherapy Illustrated: Model of the GABA Receptor–Chloride Channel Molecules in Relationship to Antiseizure Pharmacotherapy Barbiturates and GABA Agents • Monitor Patient’s condition • Liver and kidney function • Pregnancy Category D • Common side effects Patient Teaching • Use reliable contraception • Immediately report pregnancy • Report excessive signs of bleeding • Report drowsiness and bone pain Drugs that Potentiate GABA Action • Act by changing the action of gamma-aminobutyric acid (GABA), the primary inhibitory neurotransmitter in the brain • Predominate effect of GABA potentiation is CNS depression Benzodiazepines— Schedule IV Drug • Monitor for drug-abuse potential • Pregnancy risk—Pregnancy Category D • Contraindicated in narrow-angle glaucoma • Respiratory depression may result with other CNS depressants. • Common side effects include dizziness, drowsiness • Overdose—give flumazenil (Romazicon) Patient Teaching • Avoid alcohol, OTC drugs, and herbal medications • Avoid nicotine • Avoid driving and hazardous activities • Rebound seizures if discontinued abruptly • Take with food • Drug often used illegally Hydantoin and Phenytoin-like Drugs • Monitor serum-drug levels • Monitor for signs of toxicity • Monitor for blood dyscrasias and bleeding disorders • Monitor liver and kidney function • Fatal hepatotoxicity can occur Hydantoin and Phenytoin-like Drugs Contraindications • Patients with hypersensitivity to hydantoin products should be cautious. • Rash, seizures due to hypoglycemia, sinus bradycardia, and heart block Patient Teaching • Routine labs for serum level • Routine labs for liver and kidney function • Immediately report signs of toxicity • Immediately report unusual bleeding • Immediately report liver or brain disease • Immediately report heart block, hypoglycemia, or pregnancy Succinimides • Do not abruptly withdraw medication • Use with caution with antiseizure medications, phenothiazines, and antidepressants • Pregnancy risk—pregnancy Category C Common Adverse Reactions • Drowsiness, headache, fatigue, dizziness • Depression or euphoria • Nausea, vomiting, weight loss • Abdominal pain Life-Threatening Reactions • Severe mental depression with suicide intent • Stevens-Johnson syndrome • Blood dyscrasias Patient Teaching • Immediately report mood changes or suicidal thoughts • Avoid driving and hazardous activities • Do not suddenly stop taking • Take with food • Report symptoms of fever or sore throat • Report weight loss and anorexia Dosage Procedure • Start with smallest initial dose • Add additional drugs, if necessary • Ensure compatibility with other medications • Monitor serum-drug levels Withdrawal of Antiseizure Medications • Should be seizure free at least three years • Withdraw gradually over several months • Resume medications if seizures return • Be aware of rebound seizures Drugs That Potentiate GABA Action • Barbiturates • Benzodiazepines • Miscellaneous GABA agents Barbiturates phenobarbital (Luminal) • Mechanism of action: changing the action of GABA • Primary use: controlling seizures • Adverse effects: dependence, drowsiness, vitamin deficiencies, laryngospasm • Prototype drug: Prototype Drug: Phenobarbital (Luminal) Benzodiazepines • Prototype drug: diazepam (Valium) • Mechanism of action: similar to that of barbiturates but safer • Primary use: for short-term seizure control • Adverse effects: drowsiness and dizziness Prototype Drug: Diazepam (Valium) Diazepam Animation Click here to view an animation on the topic of diazepam. Hydantoins • Prototype drug: phenytoin (Dilantin) • Mechanism of action: to densitize sodium channels • Primary use: treating all types of epilepsy except absence seizures • Adverse effects: CNS depression, gingival hyperplasia, skin rash, cardiac dysrhythmias, and hypotension Prototype Drug: Phenytoin (Dilantin) Prototype Drug: Phenytoin (Dilantin) Phenytoin-Like Drugs Valproic acid (Depakene) • Mechanism of action: to desensitize sodium channels • Primary use: for absence seizures • Adverse effects: limited CNS depression, visual disturbances, ataxia, vertigo, headache • Prototype drug: • Additional adverse reactions: gastrointestinal effects, hepatotoxicity, pancreatitis Valproic Acid Animation Click here to view an animation on the topic of valproic acid. Prototype Drug: Valproic Acid (Depakene, Depakote) Succinimides ethosuximide (Zarontin) • Mechanism of action: suppress calcium influx • Primary use: for absence seizures • Adverse effects: rare but include drowsiness, dizziness, lethargy • Very rare but serious side effects: systemic lupus erythematosis, leukopenia, aplastic anemia, Stevens-Johnson syndrome • Prototype drug: Prototype Drug: Ethosuximide (Zarontin) Drugs That Potentiate GABA Action • Include barbiturates, benzodiazepines, and miscellaneous GABA agents • Suppress the firing ability of neurons Treating Seizures with Barbituates • Low margin for safety • High potential for dependence, and they cause • Profound CNS depression • Overall effective against all major seizure types except absence seizures Examples of Barbiturates • Phenobarbital (Luminal) • Amobarbital (Amytal) • Secobarbital (Seconal) • Pentobarbital (Nembutal) Treating Seizures with Benzodiazepines • Indications include absence seizures and myoclonic seizures • Tolerance may develop quickly • one of most widely prescribed classes, used also for anxiety, skeletal muscle spasms, and alcohol withdrawal symptoms Examples of Benzodiazepines • Clonazepam (Klonopin) • Clorazepate (Tranxene) • Lorazepam (Ativan) • Diazepam (Valium) Newer GABA-related Drugs • Gabapentin (Neurontin) • Pregabalin (Lyrica) • Tiagabine (Gabitril) • Topiramate (Topamax) Hydantoin and Newer Drugs • Delay an influx of sodium ions across neuronal membranes • Sodium movement is factor that determines whether neuron will undergo an action potential • Sodium channels are not blocked; they are just desensitized Treating Seizures With Hydantoins and Related Drugs • Useful in treating all types of epilepsy except absence seizures • Provides effective seizure suppression, without the abuse potential or CNS depression associated with barbiturates • Phenytoin-related drugs used less frequently Examples of Hydantoins • Phenytoin (Dilantin)—most common • Fosphenytoin (Cerebyx) Examples of Phenytoin-like Drugs • Carbamazepine (Tegretol)—tonic-clonic and • • • • partial seizures Felbamate (Felbatol) Lamotrigine (Lamictal) Valproic acid (Depakene, Depakote)—absence seizures Zonisamide (Zonegran) Treating Seizures with Succinimides • Suppress seizures by delaying calcium influx into neurons • Generally only effective against absence seizures • Ethosuximide (Zarontin) is the most commonly prescribed drug in this class Succinimides • Examples of succinimides • Ethosuximide (Zarontin) • Methsuximide (Celontin) • Phensuximide (Milontin) NCLEX-RN Review Question 1 The nurse evaluates patient teaching related to causes of seizures. Further teaching is needed if the patient makes which of the following statements? 1. 2. 3. 4. “Seizures can be caused by inflammation of the brain.” “Seizures can be caused by low blood sugar.” “My relative had seizures because of a large tumor growing in his muscles.” “Seizures may occur after a head injury.” NCLEX-RN Review Question 1 – Answer 1. 2. 3. 4. “Seizures can be caused by inflammation of the brain.” “Seizures can be caused by low blood sugar.” “My relative had seizures because of a large tumor growing in his muscles.” “Seizures may occur after a head injury.” NCLEX-RN Review Question 1 – Rationale Rationale: Seizures may be caused by inflammation, head injuries, or low blood sugar levels. Rapid-growing, space-occupying lesions in the brain, which increase intracranial pressure, may cause seizures, but not tumors, within the muscles. NCLEX-RN Review Question 2 The nursing student asks the nurse to explain the action of the antiseizure medication, phenytoin. The nurse explains the mechanism of action as: 1. 2. 3. 4. Suppression of the influx of chloride into the neuron Stimulation of the influx of calcium into the neuron Suppression of the influx of sodium into the neuron Stimulation of calcium and sodium needed to suppress seizure activity NCLEX-RN Review Question 2 – Answer 1. 2. 3. 4. Suppression of the influx of chloride into the neuron Stimulation of the influx of calcium into the neuron Suppression of the influx of sodium into the neuron Stimulation of calcium and sodium needed to suppress seizure activity NCLEX-RN Review Question 2 – Rationale Rationale: The influx of sodium into a neuron enhances neuronal activity. The delay of an influx suppresses neurotransmitter frequency. NCLEX-RN Review Question 3 The nurse recognizes that several chemicals inhibit neurotransmitter function in the brain. The primary inhibitory transmitter in the brain is: 1. 2. 3. 4. Sodium GABA Chloride Calcium NCLEX-RN Review Question 3 – Answer 1. 2. 3. 4. Sodium GABA Chloride Calcium NCLEX-RN Review Question 3 – Rationale Rationale: GABA drugs mimic GABA by stimulating the influx of chloride ions into the neuron, leading to the suppression of neuron firing. NCLEX-RN Review Question 4 The patient, age 8, is prescribed valproic acid (Depakene) for treatment of a seizure disorder. The nurse should monitor the patient closely for: 1. 2. 3. 4. Hyperthermia Vitamin B deficiency Restlessness and agitation Respiratory distress NCLEX-RN Review Question 4 – Answer 1. 2. 3. 4. Hyperthermia Vitamin B deficiency Restlessness and agitation Respiratory distress NCLEX-RN Review Question 4 – Rationale Rationale: Valproic acid may produce an idiosyncratic response in children, including restlessness and psychomotor agitation. NCLEX-RN Review Question 5 Discharge teaching for a patient receiving carbamazepine (Tegretol) should include: 1. 2. 3. 4. Monitoring blood glucose and reporting decreased levels Expecting a discoloration of contact lenses Immediately reporting unusual bleeding or bruises to the health care provider Expecting a green discoloration of urine NCLEX-RN Review Question 5 – Answer 1. 2. 3. 4. Monitoring blood glucose and reporting decreased levels Expecting a discoloration of contact lenses Immediately reporting unusual bleeding or bruises to the health care provider Expecting a green discoloration of urine NCLEX-RN Review Question 5 – Rationale Rationale: Carbamazepine affects vitamin K metabolism and may lead to blood dyscrasias and bleeding. Pathophysiology Of Seizures / Discussion Seizures • Abnormal or uncontrolled neuronal discharges in the brain • Affect • Consciousness • Motor activity • Sensation • Symptom of an underlying disorder Convulsion • Involuntary violent spasm of large muscles of face, neck, arms, and legs • Not synonymous with seizure Different etiologies of seizure activity • Most common serious neurologic problem affecting children • May present as an acute situation, or they may occur on a chronic basis Known Causes of Seizures • Infectious diseases • Trauma • Metabolic disorders • Vascular diseases • Pediatric disorders • Neoplastic disease Additional Known Causes of Seizures • Medications • High doses of local anesthetics • Eclampsia • Drug abuse • Withdrawal syndromes from alcohol or sedative-hypnotic drugs Pregnancy and Epilepsy • Several antiseizure drugs decrease effectiveness of oral contraceptives • Most antiseizure drugs are pregnancy category D • Eclampsia - severe hypertensive disorder of pregnancy, characterized by seizures, coma, and perinatal mortality Epilepsy • Seizures occurring chronically • International Classification of Epileptic Seizures • Partial (focal) • Generalized • Special epileptic syndromes Seizures in Neonates, Infants, and Children • Congenital abnormalities of CNS • Perinatal brain injury • Metabolic imbalances Later-Childhood Etiology • CNS infections • Neurological degenerative disorders • Inherited epilepsies Adult Etiology • Cerebral trauma • Cerebrovascular disorders • Neoplastic disease Signs and Symptoms of Seizures • Related to area of brain with abnormal activity • International Classification of Epileptic Seizures: classifies seizures Simple Partial Seizures • Olfactory, auditory, and visual hallucinations • Intense emotions • Twitching of arms, legs, and face Complex Partial (psychomotor) Seizures • Aura (preceding) • Brief period of confusion or sleepiness afterward with no memory of seizure (postictal confusion) • Fumbling with or attempting to remove clothing • No response to verbal commands Generalized Seizures • Absence (petit mal) • Atonic (drop attacks) • Tonic-clonic (grand mal) Absence Seizures • Lasting a few seconds • Seen most often in children (child stares into space, does not respond to verbal stimulation, may have fluttering eyelids or jerking) • Misdiagnosed often (especially in child) as ADD or daydreaming Atonic Seizures • Falling or stumbling for no reason • Lasting a few seconds Tonic-Clonic Seizures • Preceeded by aura • Intense muscle contraction (tonic phase) followed by alternating contraction and relaxation of muscles (clonic phase) • Crying at beginning as air leaves lungs; loss of bowel/bladder control; shallow breathing with periods of apnea; usually lasting 1–2 minutes • Disorientation and deep sleep after seizure (postictal state) Special Syndromes • Febrile seizures • Myoclonic seizures • Status epilepticus Febrile Seizures • Tonic–clonic activity lasting 1–2 minutes • Rapid return to consciousness • Occurs in children usually between 3 months and 5 years of age Myoclonic Seizures • Large jerking movements of a major muscle group, such as an arm • Falling from a sitting position or dropping what is held Status Epilepticus • Considered a medical emergency • Continuous seizure activity, which can lead to coma and death Choice of Drug Depends Upon • Type of seizure • Patient’s history and diagnostic studies • Associated pathologies Once Medication is Selected • Patient placed on low initial dose • Amount gradually increased • If seizure activity remains, different medication added in small increments • Newer antiseizure drugs have less adverse side effects than older drugs • Most cases require only a single drug New FDA Warnings • Study included patients with epilepsy, bipolar disorder, psychoses, migraines, and neuropathic pain • Popular antiseizure examples found to almost double risk of suicidal behavior and ideation Drug Therapy for Epilepsy • Assessment • History of seizure activity • Allergies and drug history • Knowledge of disease process • Knowledge of drug therapy • Patient lifestyle Drug Therapy for Epilepsy (cont'd) • Nursing Diagnoses • Low Self-Esteem (situational or chronic; related to disease effects) • Impaired Social Interaction (related to disease, lack of seizure control) • Deficient Knowledge (drug therapy) Risk for Injury (related to seizures or adverse drug effects) • Drug Therapy for Epilepsy (cont'd) • Planning • Experience therapeutic effects dependent on the reason the drug is given • Be free from, or experience minimal, adverse effects. • Understanding of disease and drug regimen and purpose • Understanding of drug regimen • Demonstrate proper self-administration Drug Therapy for Epilepsy (cont'd) • Implementation • Monitoring neurological status • Ensuring lab values in normal range • Patient/family teaching about disease • Patient/family teaching about drugs • Patient/family teaching about care during seizure activity Drug Therapy for Epilepsy (cont'd) • Evaluation • Effectiveness of drug therapy • Patient goals Nursing Process Focus: Patients Receiving Antiseizure Drug Therapy Nursing Process Focus: Patients Receiving Antiseizure Drug Therapy Nursing Process Focus: Patients Receiving Antiseizure Drug Therapy Nursing Process Focus: Patients Receiving Antiseizure Drug Therapy Nursing Process Focus: Patients Receiving Antiseizure Drug Therapy Nursing Process Focus: Patients Receiving Antiseizure Drug Therapy