Type 2 Diabetes Guidelines: AAP - American Academy of Pediatrics
advertisement

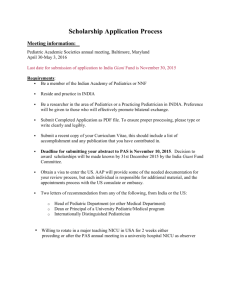
TM TM Prepared for your next patient. AAP Clinical Practice Guideline: Management of Newly Diagnosed Type 2 Diabetes Mellitus in Children and Adolescents Janet Silverstein, MD University of Florida Kenneth C. Copeland, MD University of Oklahoma TM AAP Resources on Diabetes Enjoy a 20% DISCOUNT through April 12, 2013 on new orders of the following AAP resources! Go to the AAP Bookstore at www.aap.org/bookstore and use promo code T2WEB. Pediatric Clinical Practice Guidelines & Policies, 13th Edition [MA0663] AM:STARS – Asthma and Diabetes in the Adolescent [MA0523] Type 2 Diabetes: Tips for Healthy Living [HE50527] Pediatric Care Online [PCO] Patient Education Online [ONPE] TM Disclaimers Statements and opinions expressed are those of the authors and not necessarily those of the American Academy of Pediatrics. All clinical practice guidelines from the American Academy of Pediatrics automatically expire five years after publication unless reaffirmed, revised, or retired at or before that time. TM Disclaimers (continued) The guidelines discussed today emerged through the work of the AAP Subcommittee on Type 2 Diabetes (with oversight provided by the Steering Committee on Quality Improvement and Management, 2008–2012). The recommendations reviewed in this webinar were recently published in the February issue of Pediatrics (2013;131[2]:364–382). The online version can be accessed at http://pediatrics.aappublications.org/content/131/2/364.full. The recommendations do not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate. o Co-chair Copeland, KC — AAP Endocrinology and Pediatric Endocrine Society Liaison (Individual disclaimers: Novo Nordisk, Genentech, Endo, and Daichi Sankyo [National Advisory Groups]; published research related to type 2 diabetes) o Co-Chair Silverstein, J — AAP Endocrinology and American Diabetes Association Liaison (Individual disclaimers: small grants with Pfizer, Novo Nordisk, Sanofi-Aventis, Daichi Sankyo, and Lilly; grant review committee for Genentech; advisory committees for Sanofi-Aventis, and Abbott; published research related to type 2 diabetes) The authors do not intend to discuss an unapproved or investigative use of a commercial product or device in this presentation. TM Case #1 A 12-year-old obese Mexican American female has a 3month history of polyuria, polydipsia, and has noted a 3pound weight loss. Her blood glucose (BG) level is 282 mg/dl and she has large ketones on urinalysis. Her A1c level is 9.2%. Her father and maternal grandmother have type 2 diabetes (T2DM). TM Point of Care Laboratory Studies Urine ketones via strip and vial Blood glucose level via meter TM Questions What type of diabetes does she have? Does she need any additional testing? What is the proper initial therapy for her? After BG levels return to normal, what would you treat her with? TM Barriers to Accurate Classification 20–25% of patients newly diagnosed with type 1 diabetes mellitus (T1DM) are obese. ≥15% of minority populations have a family history (FH) of a T2DM baseline. 3X increase FH of T2DM in patients with T1DM. Overlap of C-Peptide measurements at onset and first year. 10–30% of typical pediatric T2DM have diabetes-specific autoimmunity markers. >30% T2DM have ketosis at disease onset. Classification of Diabetes Type 1 Type 2 Not usually overweight Proportionate to obesity in general population 85% are overweight Short course Indolent course 35–40% present with ketoacidosis 33% with ketonuria 5–25% may have ketoacidosis Caucasians predominate Native American; African American; Latino; Asian; Pacific Islander Increased incidence of other Increases in polycystic ovary syndrome, autoimmune diagnoses: hypertension, triglyceride (TG), low thyroid; adrenal; vitiligo; high-density lipoprotein (HDL) celiac disease Acanthosis nigricans (up to 90%) Does she need any additional testing? Laboratory Evaluation Islet autoantibodies o o o o Islet cell antibodies (ICA) Insulin autoantibodies (IAA) Glutamic acid decarboxylase (GAD) Insulin-associated protein-2 (IA-2) C-Peptide / insulin levels o After 1st year Lipid profile What is the proper initial therapy for her? TM AAP Key Action Statement #1 Clinicians must ensure that insulin therapy is initiated for children and adolescents with T2DM o o o o Who are ketotic or in diabetic ketoacidosis Who have venous or plasma BG levels >250 mg/dl Who have hemoglobin A1c >9%; or In whom the distinction between type 1 and type 2 diabetes is unclear TM Case #2 A 16-year-old obese Native American female has a 6-month history of polyuria and polydipsia, coincident with a 56pound weight gain over the last year and profound darkening of skin beneath her neck and under her arms. Her weight is 228 pounds. Her BG is 226 mg/dl and her A1c is 7.4%. She has no ketones on urinalysis. Questions: o Does she have diabetes? o What type of diabetes does she have? o What is the proper initial therapy for her? TM AAP Key Action Statement #2 In all other instances, clinicians should Initiate a lifestyle modification program, including nutrition and physical activity. AND Start metformin as first-line therapy for children and adolescents at the time of diagnosis with T2DM. TM TODAY* Data on the Limitations of Metformin Rx Main TODAY results: o Among metformin (met) alone versus met + rosiglitazone (rosi) versus met + lifestyle, met alone was inferior to met + rosi, and especially inferior in African Americans. Among those on met alone who failed to maintain glycemic control, approximately 50% failed within one year of treatment (almost 70% of African Americans on met alone failed within three years of treatment). o Failure rates of the three treatment arms included: • 51.7% met alone • 46.6% met + lifestyle • 38.6% met + rosi Take home message: Start on metformin, but be alert to the need to intensify therapy early. *TODAY Study Group, Zeitler P, Hirst K, Pyle L, et.al. A clinical trial to maintain glycemic control in youth with type 2 diabetes. N Engl J Med. 2012;366(24):2247–2256. TM TODAY Data (continued) The TODAY cohort was comprised of youth with significant barriers to good health. o 41.5% household annual income <$25,000 o 26.3% highest education level of parent/guardian less than a high school degree o 38.8% living with both biological parents o 41.1% Hispanic and 31.5% African American Other take home messages: o Lifestyle changes are exceedingly difficult to effect in youth of this socio-economic demographic. o Despite the extraordinary resources and efforts devoted to lifestyle change, as noted above, weight loss was only modest and short-lived, even in the met + lifestyle group. TM AAP Key Action Statement #3 The committee suggests that clinicians monitor A1c levels every three months and intensify* treatment if treatment goals for BG and A1c levels are not being met. *Intensification is defined as: Increase the frequency of BG monitoring and adjust dose and type of medication in an attempt to decrease BG. TM A1c and BG Targets A1c o Ideal <7% o Must individualize with realistic goals BG o Fasting blood glucose 70–130 mg/dL TM Intensification Activities Increase frequency of clinic visits. Engage in more frequent BG monitoring. Add one or more “anti-diabetic” medications. Meet with dietitian or diabetes educators. Meet with psychologist or social worker. Increase attention to diet and exercise regimens. TM AAP Key Action Statement #4 The committee suggests that clinicians advise patients to monitor finger-stick BG levels in those who: o Are taking insulin or other medications with a risk of hypoglycemia; or o Are initiating or changing their diabetes treatment regimen; or o Have not met treatment goals; or o Have intercurrent illnesses. Monitoring frequency may be modified once BG levels are at target for patients who are not on insulin and whose A1c is <7%. TM AAP Key Action Statement #5 The committee suggests that clinicians incorporate the Academy of Nutrition and Dietetics’ Pediatric Weight Management Evidence-Based Nutrition Practice Guidelines in their dietary or nutrition counseling: o At the time of diagnosis o As part of on-going management • 900–1200 kcal/day for 6- to 12-year-olds if >120% ideal body weight • Restrictions of no less than 1200 kcal/day for 13- to 18-yearolds TM AAP Key Action Statement #6 The committee suggests that clinicians encourage children with T2DM to: o Engage in moderate to vigorous activity for at least 60 minutes daily. AND o Limit non-academic screen time to less than two hours a day. TM American Diabetes Association (ADA) Recommendations for Co-morbidity Screening At diagnosis: o o o o Blood pressure (BP) Fasting lipids Urine microalbumin / creatinine Dilated eye examination Follow-up: o BP at each visit o Fasting lipids annually (if abnormal) or every five years (if lowdensity lipoprotein cholesterol [LDL-C] <100) o Urine microalbumin / creatinine annually • Need two confirmatory specimens if >30 mg/gm creatinine o Dilated eye examination annually TM Prevalence of Cardiovascular Risk Factors: SEARCH for Diabetes in Youth Population-based study of 2096 diabetic youth 0 to 19 years old. Cardiovascular (CV) disease risk factors: HDL-C <40 mg/dL; TG >110 mg/d; waist circumference >90%; systolic BP (sBP) or diastolic BP (dBP) >90 percentile N ↑TG % ↓HDL % ↑WC % HTN % ≥2 CV risk factors T1DM 1376 14 9 15 22 14% T2DM 63 65 60 95 73 92% Rodriguez BL, Fujimoto WY, Mayer-Davis EJ, et al. Prevalence of cardiovascular disease risk factors in U.S. children and adolescents with diabetes: the SEARCH for diabetes in youth study. Diabetes Care. 2006;29(8):1891–1896. TM ADA Recommendations for Management of Co-morbidities Hypertension / microalbuminuria o If sBP or dBP >90 percentile • Diet and exercise to attempt weight control o If sBP or dBP >90 percentile persistently for three to six months despite diet/exercise, consider angiotensinconverting enzyme (ACE) inhibitor. o If sBP or dBP >95 percentile persistently, treat with an ACE inhibitor. Treatment with ACE inhibitor helps reverse microalbuminuria (>30 mg/gm creatinine on three occasions). TM ADA Recommendations for Management of Co-morbidities (continued) Dyslipidemia o Medical nutrition therapy with step 2 American Heart Association diet and optimization of BG o Add statin if: • LDL-C >160 mg/dL; or • LDL-C >130 mg/dL if ≥1 CV risk factor • If LDL-C 130–160 mg/dL after three to six months lifestyle modification TM Clinical Management of Statins Measure baseline aspartate transaminase (AST) / alanine transaminase (ALT) before statin use. o Can continue statins if ALT / AST are <3X upper limits of normal if monitored closely. o Discontinue statin if muscle symptoms appear, and measure creatine phosphokinase (CPK). o If CPK is within normal limits or <3X normal, can continue statin and monitor symptoms. • Consider dose reduction. o Statin must be discontinued if CPK is >10X normal. Pasternak RC, Smith SC, Bairey-Merz CN, et al. ACC/AHA/NHLBI clinical advisory on the use and safety of statins12. J Amer Coll Cardiol. 2002;40(3):573–572. TM Additional AAP Resources on Diabetes Enjoy a 20% DISCOUNT through April 12, 2013 on new orders of the following AAP resources! Go to the AAP Bookstore at www.aap.org/bookstore and use promo code T2WEB. Pediatric Clinical Practice Guidelines & Policies, 13th Edition [MA0663] AM:STARS – Asthma and Diabetes in the Adolescent [MA0523] Type 2 Diabetes: Tips for Healthy Living [HE50527] Pediatric Care Online [PCO] Patient Education Online [ONPE] TM Free PCO Trial Visit Pediatric Care Online today for additional information on this and other topics. www.pediatriccareonline.org Pediatric Care Online is a convenient electronic resource for immediate expert help with virtually every pediatric clinical information need with must-have resources that are included in a comprehensive reference library and time-saving clinical tools. Don’t have a subscription to PCO? Then take advantage of a free trial today! Call 888/363-2362 or, for more information, go to https://www.pediatriccareonline.org/prepared/freetrial.html. TM Coming Soon! AAP Essentials: Type 2 Diabetes App Available April 2013 iTunes App Store ($19.99) Quick, on-the-go access to o Treatment algorithm o Key Action Statements o Monitoring and lifestyle management plan tools For all AAP app information, visit www.aap.org/mobile.