Chronic Lymphocytic Leukemia (CLL) Presentation
advertisement

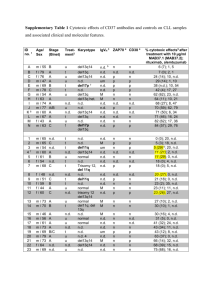
Chronic Lymphocytic Leukemia (CLL) DEFINITION CLL is a neoplastic disease characterized by proliferation and accumulation (blood, marrow and lymphoid organs) of morphologically mature but immunologically dysfunctional lymphocytes CLL - characteristic • Disease of elderly (50-60 years) • 2:1 ratio of male to female • Most common adult leukemia in Europe and USA (USA: 3/100.000 population) • In 98% of cases leukemic cells are monoclonal population of immature B lymphocytes with low-density surface immunoglobulin • Etiology unknown CLL – clinical features • Most of patients: fatigue, reduced exercises tolerance, weight loss, fever, recurrent infections, sweats, bleeding • 25% of patients: asymptomatic • 80% of patients : nontender lymphadenopaty • 50% of patients: splenomegaly • Hepatomegaly CLL - diagnostic features a) Blood test lymphocytosis ≥ 5G/l (4 weeks) b) Morphology monoconal population of small mature lymphocyte c) B-cell CLL phenotype clonal CD5+/CD19+ population of lymphocyte d) Markers of clonality κ/λ light chain restriction; cytogenetical abnormalities e) Bone marrow infiltrate > 30% of nuceated cells on aspirate f) Lymph node diffuse infiltrate of small lymphocye CLL – diagnosis (2) • Blood test – anaemia – trombocytopenia – smudge cells in peripheral blood film • Lymh node histology: diffuse infiltrate of small lymphocyte • Bone marrow histology – interstitial infiltration (30% - good prognosis) – diffuse involvement (25% - poor prognosis) – nodular involvement • Hypogammaglobulinemia • Cytogenetic abnormalities (FISH – 90%) – 13q-; 11q-; +12q; 17p-; 6q- • Molecular abnormalities – p53; bcl2 CLL – clinical staging (1) RAI CLINICAL STAGING SYSTEM • Stage Clinical Features at Diagnosis Median Survival (m) ________________________________________________________________________ • Low risk • 0 Blood (> 5.000/ul. monoclonal lymphocytes) >150 • and marrow (>30%) lymphocytosis • Intermediate risk • I Lymphocytosis and enlarged lymph nodes > 101 • II Lymphocytosis and enlarged spleen and/or liver > 71 • High risk • III Lymphocytosis and anemia (Hgb < 11g/dL) > 19 • IV Lymphocytosis and thrombocytopenia (Plt < 100.000/ul.) > 19 CLL – Rai stages CLL – clinical staging (2) BINET CLINICAL STAGING SYSTEM • Stage Clinical Features at Diagnosis Median Survival (m) ____________________________________________________________________ • A Blood (> 5.000/ul. monoclonal lymphocytes) > 84 • and marrow (>30%) lymphocytosis and less • than 3 areas of palpable lymphoid-tissue enlargement • B Lymphocytosis and 3 and more areas of palpable < 60 • lymphoid-tissue enlargement • C Lymphocytosis with anemia (Hgb <11g/dL; < 24 • women <10g/dL) • or thrombocytopenia (Plt <100.000/uL) • ___________________________________________________________________ An area: cervical, axillary, inguinal/femoral, spleen, liver CLL – Binet stages CLL – prognostic factors • clinical stage • marrow histology (diffuse marrow involvement - poor prognosis) • leukemia cell doubling time • • • • CD38 expression IgVH mutational status ZAP-70 expression FISH cytogenetic – low-risk: normal kariotype; isolated del(13q) – high-risk: del(17p0, del(11q), trisomy 12 • serum markers: 2-microglobulin; thymidine- kinase, sCD23 CLL : ZAP-70 CLL – treatment (1) • Watch and wait • Monotherapy – glucocorticoids – alkylating agents (Chlorambucil, Cyclophosphamide) – purine analogues (Fludarabine, Cladribine, Pentostatin) • Combination chemotherapy – Chlorambucil/ Cyclophosphamide + Prednisone – Fludarabine + Cyclophosphamide +/- Mitoxantrone – CVP, CHOP • Monoclonal antibodies (monotherapy and in combination) – Alemtuzumab (anti-CD52) – Rituximab (anti-CD20) • Splenectomy • Radiotherapy CLL – treatment (2) • Hematopoietic stem cell transplantation – allogeneic with reduced intesity conditioning – autologous • New and novel agents – – – – – Oblimersen – bcl2-directed antisense oligonucleotide Lenalidomide Flavopiridol Anti-CD23 Anti-CD40 • Vaccine strategies • Supportive therapy (allopurinol, G-CSF, blood and platelet transfusion, immunoglobulins, antibiotics)