CLL
advertisement

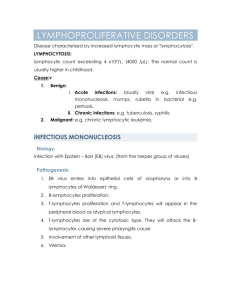
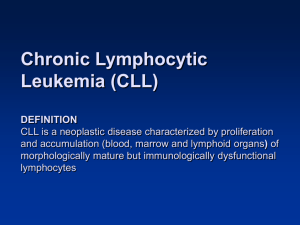
CHRONIC LYMPHOCYTIC LEUKEMIA Amanda Pressman, M.D. July 2005 Background First described in 1924 by Minot and Isaacs, CLL is the most common adult leukemia in North America and Western Europe. The epidemiology varies widely with geography (higher rates in Western Europe, lower in East Asia) Clinical Presentation Asymptomatic Diagnosis made when routine CBC demonstrates significant lymphocytosis (25%) Lymphadenopathy Generalized or localized lymphadenopathy is the most common finding (50-80%) Most commonly affect the cervical, supraclavicular and axillary lymph nodes Typically appear as firm, discrete, nontender, LAD Hepatomegaly/Splenomegaly Likely enlarged secondary to leukemic infiltration, is present in 25-50% at presentation “B” symptoms Fatigue, nightsweats, fevers, weight loss are present in 10-20% Labs Lymphocytosis in most cases, often with smudge cells Anemia and thrombocytopenia are common Autoimmune hemolytic anemia and autoimmune thrombocytopenia may be seen Often elevated LDH, b-2 microglobulin and rarely elevated uric acid, transaminases, Ca Radiography Not required to diagnose CLL CXR may show hilar or mediastinal lymphadenopathy CT may show enlarged lymph nodes, hepatosplenomegaly, or provide a baseline Diagnosis Lymphocytes Absolute lymphocyte count >10,000/uL (normal <2,500) and sustained for 1-6 months Peripheral smear with mature-appearing lymphocytes, 50-100% of leukocytes If absolute lymphocyte count between 5-10,000, phenotyping must be performed Phenotyping Malignant B-CLL has the morphologic appearance of normal, small lymphocytes Reflective of functional and developmental immaturity of lymphocytes Very low levels of surface membrane immunoglobulin (SmIg) Expression of B-cell antigens CD19, CD20, CD24 Expression of T-cell associated antigen CD5 Others: CD23, mouse RBC receptors, common CLL-associated antigen Bone Marrow Normo to hypercellular bone marrow with at least 30% lymphocytes May form nodular, interstitial, or diffuse patterns Chromosomal Abnormalities No specific pattern for CLL, but may see trisomy 12, 3, or 6, translocations of (11;14), (q13;q32), (14:18), and deletions in the long arm of 11, 13 and the short arm of 17 Differential Diagnosis Infection: EBV, pertussis and toxoplasmosis may cause transient lymphocytosis Small lymphocytic lymphoma: identical disease to CLL but represents a different stage in which disease is confined to a lymph node due to differences in adhesion molecules Mantle cell lymphoma: Have irregular or cleaved lymphocyte nuclei and are SmIg (+) Lymphoplasmacytic lymphoma: Maturation towards plasma cell, my be PCA1 and CD38 (+) Hairy cell leukemia: Typical morphologic features, CD5 & CD21(-)/CD25, CD11c, CD 103 (+) Large granular lymphocytic leukemia: Large mononuclear cells, CD3, CD8, CD57 (+)/CD4 (-) Beth Israel Deaconess Medical Center Interns’ Report Mycosis fungoides: cerebriform nuclei and CD4 (+) and CD 8(-)leukemic manifestation of cutaneous T cell lymphoma Adult T cell lymphoma/leukemia: clover leaf nucleus and often patients have HTLV-1 Ab Prolymphocytic leukemia: large, less mature lymphocytes, often presenting with massive splenomegaly and lymphocytosis >100,000/uL. Normal SmIG, CD5 (-) in the B-cell variant. Staging/Prognosis Rai Staging System Low risk: Stage 0 (lymphocytosis) median survival 150 months Intermediate risk: Stages I-II (lymphadenopathy, organomegaly) 71-101 months High risk: Stages III and IV (anemia, thrombocytopenia) 9-24 months Binet Staging System Stage A: Fewer than 3 lymphoid sites involved <120 months Stage B: 3 or more lymphoid sites involved 60 months Stage C: Presence of anemia and/or thrombocytopenia 24 months Treatment Indications Rai stages II or IV and Binet stage C Symptomatic disease (“B” symptoms, bulky lymphadenopathy) Worsening lymphocytosis and rapid doubling time (<6 months) or Richter’s transformation Occasionally for autoimmune hemolytic anemia or thrombocytopenia, Repeated infections Options Alkylating agents: chlorambucil or cyclophosphamide with or without prednisone Purine analogs: fludarabine, cladribine, pentostatin are currently 2 nd line and are still undergoing study to become 1st line. BMT: aimed at cure for young patients, but mortality has been high Immunotherapy: IFN-a an dIL-2 are being investigated Monoclonal antibodies: rituximab and others are being investigated Radiation therapy: palliation of bulky lymphoid tissue Splenectomy: may be indicated in patients with refractory cytopenia Response Complete remission No symptoms, normal physical, absolute lymphocyte count<4,000/uL, ANC>1,500/uL, platelets>100,000, hemoglobin >11g/dL, bone marrow lymphocytosis<30% and no nodules on bone marrow biopsy Partial remission Decrease in LAD, spleno/hepatomegaly of at least 50% and ANC >=1,500, platelets >= 100,000, hemoglobin >= 11, or 50% improvement over previous reduction in hemoglobin or platelet count Complications Infection Largest contributer to morbidity and mortality in patients with CLL Immunosuppressed state generally secondary to hypogammaglobulinemia (usually all 3 classes: IgG, IgA and IgM), but also affected by hypersplenism and chemotherapy Most common infections are bacterial, however patients treated with purine analogs are at risk of developing opportunistic infections and are at risk for fungal and viral infections as well as TB, listeria, PCP In patients with repeated infections, periodic IVIG infusion significantly reduces the incidence of bacterial infections Malignancy Transformations Richter’s transformation: diffuse large cell lymphoma in CLL patients that presents with abrupt fever, asymmetric LAD, and causes rapid patient decline Hodgkin’s, ALL Second malignancies Non-melanoma skin cancer, sarcoma, kidney, lung Beth Israel Deaconess Medical Center Interns’ Report