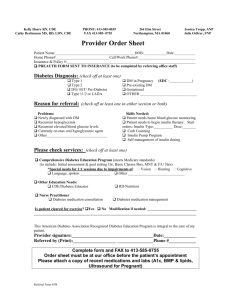
Screening for type 2 diabetes
advertisement

what’s new in type 2? We are in a diabesity epidemic! Prevalence of type 2 diabetes and metabolic syndrome is increasing in children and their parents Risk of complications of type 2 are higher in type 2 with onset 18-45 than in older adults Most children with diabetes are cared for by their primary doctors JCEM 88:1417,2003, Goran Obesity Visceral Adiposity Androgens Adipocytokines Puberty Inflammation Insulin Resistance Hypertension Dyslipidemia Cardiovascular Disease Prevalence of obesity is increasing Prevalence of overweight in US children doubled from 1980-1994 Overweight 50% higher in poor US teens 17%US children and teens overweight (BMI >95%ile) 2004 NHANES 4% US children BMI>99%ile 1:17,741 pedi endos to obese kids in US Waist circumference increased 3.7 cm in teens 1994-2004 NHANES Factors contributing to the obesity epidemic Increase in intake of regular soda (high fructose corn syrup), fast foods, increase in portion size of fast foods, Increase in high carb snacks Decrease in physical activity Increase in physical inactivity (TV, video, computer time) each hour TV time=+167 kcal/day, Wiecha,Arch Ped Adol Med 160:436,2006 The metabolic syndrome Insulin resistance Hypertension Dyslipidemia Ford et al, Diabetes Care 31:587,2008 Metabolic syndrome prevalence by IDF definition 4.5% US teens National health and nutrition examination survey 1999-2004 of 2014 teens age 12-17 Type 1 diabetes beta cell destruction leading to absolute insulin deficiency Autoimmune idiopathic Type 2 diabetes mellitus: Both insulin resistance and relative insulin insufficiency: Secretory defect with insulin resistance Insulin resistance and insufficient compensatory increase in insulin production Other specific types of diabetes Genetic defects in beta cell function (MODY, mitochondrial DM) Genetic defects in insulin action (type A) Diseases of exocrine pancreas (CF etc) Endocrinopathies (Cushing’s etc) Drug induced (steroids etc) Immune mediated ( insulin receptor antibodies ) Genetic syndromes associated with DM Gestational diabetes Definition of impaired fasting glucose/ glucose intolerance Fasting plasma glucose 100-125 mg/dl (5.6-6.9 mmol/l) 2 h plasma glucose 140 mg/dl-199 mg/dl (7.8-11 mmol/l) on OGTT Prevalence of diabetes in children under 18 years Overall 1/300 (all types) (incidence 15/100,000) Type 2 diabetes 4-30% depending on ethnic mix of population Prevalence of Type 2 diabetes is rapidly increasing with increase of obesity and inactive lifestyle Risk factors for type 2 diabetes Obesity with signs of insulin resistance (acanthosis nigricans, polycystic ovary syndrome) usually post pubertal Ethnic heritage (African American, Native American, Asian, Latino, pacific islander) Family history of type 2 history of SGA or LGA Screening for type 2 diabetes BMI of 85%ile or weight > 120% above ideal body weight, age 10 or above or pubertal and: Family history of type 2 diabetes At risk ethnic group Signs or conditions associated with insulin resistance (acanthosis nigricans, hypertension, hyperlipidemia, PCOS) Screening obese children for diabetes Fasting blood sugar consider fasting lipids consider insulin level : fasting glucose/insulin > 4.5 normal (insulin not always accurate in commercial labs) Glucose 2 hour post 75 gm (1.75 gm/kg) glucose load (not yet the official recommendation of the AAP, ADA) Impaired glucose tolerance in children with marked obesity Impaired glucose tolerance in 25% of very obese children ages 4-10 years Impaired glucose tolerance in 21% very obese adolescents, 4% silent diabetes Fasting blood glucose screening would miss many individuals with impaired glucose tolerance (N Eng J Med 2002;346:802) Teen diabetes and the pediatrician Coordinate care with an endocrinologist Address adolescent health issues Acute infections (including STDs) Contraceptive needs Smoking cessation Depression Family support issues Diabetes Specialty visits At least every 3 months for education, review of blood sugars, med adjustment Monitor growth, blood pressure (<130/80) Glucose control goals (individualize): Hemoglobin A1c<7% (ideal) (lower in type 2): Preprandial plasma glucose 90-130 mg/dl Post prandial <180 mg/dl Yearly microalbumin, lipids, retinopathy screen Treatment goals for diabetes Hemoglobin A1c <7% Preprandial blood glucose 90-130 mg/dl Postprandial blood glucose < 180 mg/dl Blood pressure < 130/80 LDL cholesterol < 100 mg/dl Triglycerides < 150 mg/dl HDL cholesterol > 40 mg/dl Management of hyperlipidemia Dietary counseling, repeat lipids in 3 months LDL 130-159 mg/dl consider medication (family history, blood pressure, smoking) LDL> 160 mg/dl : begin statin at low dose, monitor LFTs, watch for persistent muscle pains, use with extreme caution in sexually active females (Diabetes Care 26:2194,2003) Barriers to good diabetes control Expense of blood glucose monitoring, medications Cultural bias against insulin or medical intervention: fatalistic attitude toward illness Insufficient parental supervision of medications and monitoring Normal adolescent development (denial) Depression Increasing obesity Encouraging optimum diabetes control Give credit for honesty and effort Diabetes visit should build self esteem Support parental involvement Set realistic goals with teen and family Keep it interesting (new technologies) Encourage regular visits and contact Group programs for teens (camps) Presentation of type 2 diabetes most teens with type 2 diabetes are identified by screening Polyuria/ polydipsia/ nocturia common symptoms but not always complaints Girls may present with recurrent yeast infections 5-25% present in DKA or hyperosmolar dehydration up to 33% have ketones at presentation Is it type 1 or type 2? More likely type 2 if overweight and: Pubertal Milder symptoms Acanthosis nigricans Family history of type 2 High risk ethnic group Features of type 2 diabetes Insulin /C peptide over upper limit of normal for assay Negative pancreatic antibody panel Initial insulin requirements 1.3-1.5 units/kg/day falling to little or no insulin requirement over 1-2 months Ketosis seldom occurs spontaneously 14 year old male with ? diabetes 2 weeks ago, vomiting, diarrhea,fatigue Glucosuria, random blood sugar in 180s Repeat BG=286 mg/dl occasional nocturia, no thirst, 6 lb weight loss BW 7 lb, MGM, MGGM type 2 diabetes Maternal aunt low thyroid BMI 35, 99%ile, 101kg ht 170 cm SMR 3, acanthosis, psoriasis Idiopathic diabetes African American / Asian teens with negative antibodies Insulinopenia: ketosis prone (episodic ketosis) Family history positive for early onset of diabetes in multiple generations Absolute requirement for insulin replacement may come and go between episodes of ketosis Control is usually poor without insulin Healthy eating and activity Avoid regular soda/ large amounts of fruit juice Encourage whole fruits, vegetables, low fat milk, (? low glycemic index choices, increased fiber) Have healthy foods for all at home Limit inactivity (TV off), encourage activity (30 minutes per day, 5+ days /week) ?discuss cigarette smoking Management of type 2 diabetes in teens If presenting in DKA or severe hyper osmolar state, start with insulin (be aware of cultural biases against insulin) Teach blood sugar monitoring from the beginning (pre and some post meal) Teach healthy eating and exercise Begin metformin at low dose increasing over several weeks if no contraindications Address lipid issues Use of metformin in type 2 diabetes Start low (500 mg with meal, go slow) Increase slowly to max 1000 mg bid, 850 mg tid with meals (or Glucophage XR) GI side effects common (nausea, diarrhea, abdominal discomfort) in first two weeks Avoid dehydration (stop if vomiting) Home BG monitoring premeal and some 2 h post meal Yearly CBC, BUN, creat, ALT,AST ? multivitamin Advantages of metformin Mild weight loss (teens love this) Decreased insulin requirement/ decreased insulin resistance Not associated with hypoglycemia Beneficial effects on cardiovascular disease shown in adults When to begin insulin rather than oral agent in type 2: Ketones present Marked hyperglycemia with dehydration Contraindications to metformin (significantly abnormal LFTs, elevated BUN/ creatinine, pregnancy) When metformin is not enough: Add insulin (NPH, glargine,detemir, or short acting insulin with meals or combinations) Add a second oral agent Take a look at lifestyle again (food and beverage choices, activity) Enlist more adult support Prevention of type 2 diabetes Lifestyle modification (exercise, healthy eating) Treatment of prediabetic conditions with metformin or other insulin sensitizing agents? Glucose intolerance Extreme obesity with insulin resistance Polycystic ovary syndrome