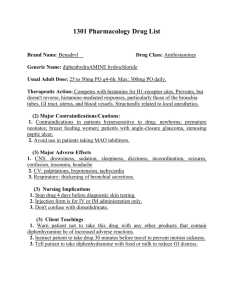
supraventricular dysrhythmias
advertisement

Source: http://www.rnceus.com/ekg/ekghowto.html Dysrhythmias • Identified by pattern and origin • Supraventricular • Atrial • Junctional • Ventricular • Manifestations? Fast Channel Action Potential Slow Channel Action Potential Goals of Dysrhythmic Therapies • Decrease symptoms • Prolong survival Achieved by Slowing rate of conduction Decreasing automaticity Increasing refractory period Classes of Dysrhythmic Drugs • • • • Class I—Sodium Channel Blockers Class II—Beta Blockers Class III—Potassium Channel Blockers Class IV—Calcium Channel Blockers Class I Sodium Channel Blockers • • • • • • Depress phase 0 Block sodium through fast channel Slow conduction velocity (SA to AV nodes) Prolong refractory period Reduce automaticity Subclasses based on action in refractory period Sodium Channel Blocker Procainamide (Procan, Procanbid, Pronestyl) • MOA: blocks sodium channels in myocardial cells, reducing automaticity and slowing conduction • Indications: acute/chronic atrial and ventricular dysrhythmias • Contraindications: AV block, severe CHF, blood dyscrasias, MG; caution in hepatotoxicity • Side Effects: n/v, HA, abdominal/joint pains (lupus-like syndrome); significant anticholinergic effects • Assessment/Monitoring: EKG, VS, drug levels, weight, edema, I/O, CBC, electrolytes, BUN/Cr, LFTs, bowel/bladder status, eye pain • Education: give NSAIDs for joint pains; report weight increase, edema, SOB, fever, syncope, jaundice, eye pain, sxs of stroke, increase fluid/fiber intake; no ETOH or stimulants; don’t skip dose Other Class I Drugs • Ia—Quinidine (Diarrhea, tinnitus) • Ib • Lidocaine* (DOC for ventricular dysrhythmias) • Mexiletine (Mexitil) • Phenytoin (Dilantin)—for Digoxin toxicity • Ic—most likely to CAUSE arrhythmias • Flecanide (Tambocor) • Propafenone (Rhythmol) Can local lidocaine given as an anesthetic affect the heart? Class II Beta Adrenergic Blockers Class II Beta Blockers • Decrease automaticity, HR • Decrease input to sinus node • Block epinephrine, NE in CNS • Decrease polarization through Purkinge fibers • Increase refractory period • Decrease risk of sudden cardiac death • Primarily supraventricular dysrhythmias Beta Blocker Propranolol (Inderal) • MOA: blocks epi, NE at beta-1 & 2 receptors, reducing HR, conduction, velocity; lowers BP • Indications: primarily SVT, or stress-induced, HTN, angina, prevention of MI, hypermetabolic states; glaucoma, migraines • Contraindications: cardiogenic shock, bradycardia, heart blocks, heart failure, asthma, COPD; caution in DM • Side Effects: hypotension, bradycardia, fatigue, depression, sexual dysfunction, hypoglycemia (DM) • Assessment/Monitoring: VS, EKG, weight, I/O, mood, glucose, lungs, safety • Education: check HR, BP, weight, report SOB, chest pain, weight gain, edema, syncope (safety), sxs of stroke, depression or ED, DO NOT DISCONTINUE Class III Potassium Channel Blockers Class III Potassium Channel Blockers • • • • • • Prolongs phase 3 of FA potential Slows repolarization Reduce automaticity Used in life-threatening arrhythmias Most likely to cause arrhythmias Less ventricular fibrillation than Class I Potassium Channel Blocker Amiodarone (Cordarone) • MOA: block potassium channels, prolongs refractory period, slows repolarization; also blocks sodium channels • Indications: resistant, life-threatening V tach • Contraindications: severe bradycardia, cardiogenic shock, heart blocks; caution in heart failure, hepatic disease • Side Effects: ARDS, thyroid disorders, blurred vision, n/v, anorexia, fatigue, syncope; skin discoloration • Assessment/Monitoring: VS, EKG, lungs/CXR/PFTs, TFTs, digoxin and warfarin levels • Education: hold for HR < 60; report chest pain, palpitations, syncope, SOB, sxs of thyroid dx: monitor weight, I/O, edema, sxs of hepatotoxicity; take with food; wear sun-screen Additional Class III • • • • Bretyllium (Bertylol) Dofetilide (Tikosyn) Ibutilide (Covert) Sotolol (Betapace) Class IV Calcium Channel Blockers Class IV Calcium Channel Blockers • Slow automaticity in SA node • Slowed impulse conduction through AV node • Prolonged refractory period • Only for supraventricular dysrhythmias Calcium Channel Blocker Verapamil (Calan) • MOA: slows calcium ions in myocardial cells and vascular smooth muscle; slows conduction velocity • • • • Indications: HTN, angina, supraventricular dysrhythmias Contraindications: hypotension, heart block, bradycardia Side Effects: hypotension, bradycardia, HA, constipation Assessment/Monitoring: VS, BP, EKG, weight, I/O, sxs of HF, bowel status • Education: hold for syncope or HR < 60; report SOB, chest pain, weight gain, edema, syncope (safety), sxs of stroke; don’t take with GF juice; do not break/chew SR tablets, increase fiber, DO NOT DISCONTINUE Additional Calcium Channel Blockers • Diltiazem (Cardizem) • Adenosine (Adenocard)—PSVT • Nifedipine (Procardia)—selective for vasculature Nursing Implications with Antidysrhythmic Drugs • Any drug that prevents or corrects a dysrhythmia is capable of causing a dysrhythmia. • Patients, especially on Class I and Class III need to be closely monitored. RB is a 74 yo male with recent CABG x 3. During the post-op period he developed PVCs and A fib. He is started on a lidocaine drip to control PVCs. What should you monitor? While receiving IV lidocaine, RB’s HR decreases to 52 with continued PVCs. What should you do? RB is now in NSR. The MD prescribes amiodarone 200 mg po daily. Why is he getting this drug and what should be monitored? RB needs more instruction regarding amiodarone when stating 1. “I will take 2 tablets, if I miss a dose.” 2. “I will report fatigue.” 3. “I will check my pulse before taking the pills.” 4. “I should use decaffeinated coffee.” Additional Dysrhythmic Drugs • Digoxin (Lanoxin) • Decreases automaticity in SA node • Slows conduction through AV node • Supraventricular dysrhythmias • Phenytoin (Dilantin); for Digoxin toxicity • Magnesium sulfate (torsades de pointes) How do we know these drugs are working? How do we know if they aren’t? Nursing Intervention • • • • • • • • • Screening? What will will monitor? Monitor which organs? Monitor which electrolytes? Interactions? Signs of success? Signs of failure? Side-effects? Safety? All of the following indicate improvement in cardiac status, except 1. Decreased pulse deficit 2. Syncope 3. Weight loss 4. Lungs CTA Causes of Shock • • • • • Hypovolemic Neurogenic Cardiogenic Anaphylactic Septic Initial Key Steps • • • • • • • Lay flat with feet elevated Keep warm Get help Call physician Initiate IVFs Oxygen Prepare for code IV Fluid Replacement • Crystalloids • Normal Saline (NS) • Lactated Ringer’s Solution (LR) • Plasmalyte • Colloids • • • • Albumin Hetastarch Dextran Plasma Protein Fraction Colloidal Fluid Replacement Albumin (Albuinar, Albutein, Buminate, Plasbumin) • MOA: maintains plasma oncotic pressure in vasculature • Indications: restore plasma volume in hypovolemic shock or restore proteins in hypoproteinemia • Contraindications: severe heart failure • Side Effects: allergy, fluid overload • Assessment/Monitoring: VS/PO, lungs, I/O, weight, edema, sxs of anaphylaxis • Education: report SOB, wheezing, palpitations, edema Additional Colloids • Plasma Protein Fraction (Plasmanate) • Dextran 40 (Gentran, Macrodex) • Hetastarch (Hespan) The client at greatest risk from fluid overload is... 1. 2. 3. 4. 36 yo with sepsis 68 yo with CHF 70 yo with HTN 70 yo with CRF Vasoconstrictor (Sympathomimetic) Norepinephrine (Levarterenol, Levophed) • MOA: alpha-1* and beta-1 agonist • Indications: acute shock (septic) and cardiac arrest • Contraindications: hypovolemic shock; caution in ischemic disease • Side Effects: HTN, reflex bradycardia, dysrhythmias, organ ischemia • Assessment/Monitoring: VS, EKG, organ fx, glaucoma, IV patency, HA, CRT • Education: report chest pain, palpitations, SOB, eye pain, IV pain, HA Other Vasoconstrictors • Isoproterenol (Isuprel); alpha & beta* • Phenylephrine (Neosynephrine); alpha • Mephentermine (Wyamine); alpha & beta The priority nursing action for a client about to receive Levophed for hypovolemic shock is... 1. Evaluate IV access 2. Measure baseline HR & BP 3. Measure urine output 4. Obtain weight Perfusion can be evaluated by all, except 1. 2. 3. 4. Vital signs Weight Output CRT The nurse knows that all are true, relating to NE, except 1. NE should be stopped immediately after BP stabilizes 2. NE may cause organ failure 3. NE requires telemetry 4. NE may aggravate glaucoma Inotropic Agent Dopamine (Dopastat, Inotropin) • MOA: stimulates dopamine receptors in kidney (activates renin/angiotensin); beta 1 agonist at moderate doses; alpha 1 at high doses • • • • Indications: maintain renal perfusion, increase CO, shock Contraindications: pheochromocytoma, ventricular fibrillation Side Effects: dysrhythmia, HTN, tissue necrosis at IV site Assessment/Monitoring: VS, EKG, I/O, weight, edema, sxs of HF, CRT, HA, IV site • Education: report chest pain, palpitations, SOB, pain at IV site, cold/numb extremeties, HA; ICU protocols Other Inotropic Agents • Digoxin (Lanoxin) • Dobutamine (Dobutrex); beta 1 The treatment for dopamine extravasation is... 1. 2. 3. 4. Atropine Narcan Neostigmine Regitine Anaphylaxis Drug (Sympathomimetic) Epinephrine (Adrenalin) • MOA: non-selective sympathomimetic • Indications: anaphylaxis • Contraindications: caution in HTN, CVA, CAD, glaucoma, dysrhythmias, organ ischemia, hyperthyroidism • Side Effects: HTN, dysrhythmias, organ ischemia • Assessment/Monitoring: VS, EKG, lungs, I/O, CRT, organ perfusion, MS • Education: report SOB, chest pain, palpitations, cold/numb extremities, anxiety; ICU protocols; injection techniques, reasons for test doses Additional Drugs for Anaphylaxis • Antihistamines (-amines) • Beta 2 agonists (-terols) • Steroids (-sones) Key Points for Shock • Correct hypovolemia before using • • • • • vasoconstrictors or inotropics All drugs given on infusion pumps Telemetry required Almost all drugs have short ½ life (x digoxin) Most have potential to cause tissue damage if extravasation occurs All can compromise organ function