Drugs for treating arrhythmias - Suny-perfusion
advertisement
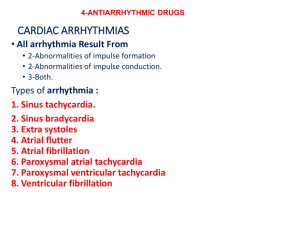
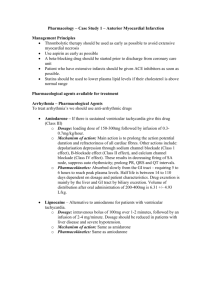
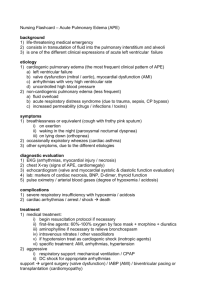
Drugs for Arrhythmias A. Pathophysiology of arrhythmias • Arrhythmias are a group of conditions in which the muscle contraction of the heart is irregular, and they occur in both healthy and diseased hearts. • Many arrhythmias are associated with other cardiovascular conditions: CAD, HT, and MI. B. Arrhythmia therapy • Antiarrhythmic drugs do not cure the underlying causes of an arrhythmia. Instead, they attempt to restore the normal cardiac rhythm. • Drugs are classified according to the phase of the action potential that they affect. 1. Class I antiarrhythmic drugs (Na1+ channel blockers) • This class of drugs reduces the excitability of the heart by slowing the spread of impulse conduction across the heart. • Sodium channel blockers are similar in structure and action to the local anesthetics. • This is the largest class of antiarrhythmic drugs. • They are subclassified according to the effects they have on the cardiac action potential. Phase 4: The resting membrane potential, when the cell is not being stimulated (represented by baseline on the ECG). Phase 0: This is the rapid depolarization phase and occurs with the opening of the Na1+ channels and the rapid influx of Na1+ into the cell. Phase 1: This phase of the action potential occurs with the closure of the Na1+ channels. There is a transient net outward current due to the movement of K1+ and Cl1- ions. Phase 0 and 1 together correspond to the QRS complex of the ECG. Phase 2: This is the plateau phase of the action potential and occurs because of the balanced inward movement of Ca2+ ions through calcium channels, and outward movement of K1+ ions through potassium channels. It corresponds to the ST segment of the ECG. Phase 3: In this phase of the action potential, the K1+ channel is still open, allowing more K1+ to leave the cell, resulting in a net loss of positive charge, which causes the cell to repolarize. Phase 3 corresponds to the T wave of the ECG. a. Class IA They slow the rate of rise of phase 0 and lengthen the action potential and are indicated for managing a variety of atrial and ventricular arrhythmias. • Quinidine, procainamide and disopyramide are drugs in this subclass. quinidine gluconate (62% quinidine): • Quinidine is indicated for a wide variety of both atrial and ventricular arrhythmias. The off label use of this is the treatment of malaria. • Dosage: • IV: infuse at 16 mg/min until arrhythmia is resolved; • PO: 325 – 650 mg every 6 hours. quinidine sulfate (83% quinidine): • Dosage: PO: 400 – 600 mg every 2 – 3 hours until arrhythmia is resolved, for supraventricular tachycardia; • 200 mg every 2 – 3 hours for 5 – 8 doses for atrial fibrillation • Quinidine is related to quinine, originally derived from the bark of the cinchona tree. • It’s side effects include a syndrome called "cinchonism" consisting of various sound and visual disturbances (hallucinations, ringing in the ears), salivation, GI disturbances, weakness, fatigue, rashes, headache, and confusion. • It can cause/aggravate Torsades de pointes (an uncommon variant of ventricular tachycardia), as can all class IA drugs procainamide (Procanbid, Promine, Pronestyl) • procainamide first approved for use in the United States in 1950, is indicated for a wide variety of both atrial and ventricular arrhythmias. • Dosage: IV: 100 mg every 5 minutes until arrhythmia is resolved, or 500 – 600 mg every 25 – 30 minutes followed by maintenance infusion of 2 – 6 mg/min. • It’s most serious adverse effects include seizures, asystole, heart block, ventricular arrhythmias and agranulocytosis. • It’s most common adverse effects are GI disturbances. Some individuals experience lupus-like symptoms (rash, muscle pain). disopyramide (Norpace, Rythmodan) • disopyramide is usually only used after quinidine and procainamide have been ruled out as possibilities. It is indicated for the treatment of ventricular tachycardia. • Dosage: PO: 150 mg every 6 hours, not to exceed 800 mg/day • Disopyramide can aggravate or precipitate severe CHF. • Other adverse effects associated with disopyramide include dry mouth, blurred vision, urinary retention, and constipation. b. Class IB They shorten the action potential and are indicated for the treatment of ventricular tachycardia and prevention of ventricular fibrillation • Lidocaine and mexilitine are drugs in this subclass. lidocaine (Xylocaine) • lidocaine is indicated for the treatment of ventricular arrhythmias. • Dosage: IV: 50 – 100 mg bolus over 2 minutes, then 1 – 4 mg/min infusion • It’s most serious adverse effects include cardiac arrest, anaphylaxis, and seizures. It’s most common adverse effects include agitation, confusion, slurred speech, tremors and drowsiness. mexiletine (Mexitil) • mexiletine (Mexitil) is structurally similar to lidocaine, except it can be administered orally. • Mexiletine is usually the class IB agent used when there is a history of MI. • Dosage mexiletine: • PO: 400 mg loading dose, then 200 mg more in 8 hours, then 200 – 400 mg every 8 hours c. Class IC They have no effect on the length of the action potential, but reduce the rate of rise of phase 0. These drugs are indicated for the treatment of ventricular tachycardia and supraventricular tachycardia. • Flecainide and propafenone are drugs in this class flecainide (Tambocor) • flecainide (Tambocor) is used in the treatment of supraventricular tachycardia. • Dosage: • PO: 100 mg every 12 hours, increased by 50 mg bid until arrhythmia is resolved (maximum daily dose of 400 mg). • It’s most serious adverse effects are CHF and arrhythmias (V-tach). • It’s most common adverse effects are dizziness and blurred vision. propafenone (Rythmol) • propafenone (Rythmol) is used in the treatment of both ventricular tachycardia and supraventricular tachycardia • Dosage: • PO: 150 mg every 8 hours, may be increased up to 300 mg every 8 – 12 hours. • It’s most serious adverse effects are the events that it is indicated for, ventricular tachycardia and supraventricular tachycardia • It’s most common adverse effects include dizziness, altered taste, nausea, vomiting and constipation. 2. Class II antiarrhythmic drugs (beta blockers) • This class of drugs are the beta blockers which block the effects of catecholamines at the β receptors, thereby decreasing sympathetic activity and resulting in a decrease in the heart rate. • They are indicated for the treatment of atrial fibrillation and atrial flutter. • These class II drugs include acebutolol, esmolol, propanolol, and sotalol. 3. Class III antiarrhythmic drugs (K1+ channel blockers) • By blocking K1+ channels, these drugs lengthen the action potential (by lengthening the refractory period/resting stage). • This tends to decrease the frequency of arrhythmias. They are indicated for the treatment of atrial fibrillation, atrial flutter, • as well as V-tach, and V-fib. • amiodarone, dofetilide and ibutilide are drugs in this class. amiodarone (Cordarone, Pacerone) • amiodarone is indicated for the treatment of life threatening ventricular arrhythmias, but only when the patient is unresponsive to less toxic agents (i.e. dofetilide or ibutilide) • Dosage: • PO: 800 – 1600 mg/day in 1 – 2 doses for 1 – 3 weeks, then 600 – 800 mg/day in 1 – 2 doses for 1 month, then 400 mg/day for maintenance • IV: 150 mg over 10 minutes, then 360 mg over 6 hours, then 540 mg over 18 hours. Maintenance infusion of 0.5 mg/minute until PO therapy is initiated. • Amiodarone has a very large number of adverse effects, affecting almost every part of the body: • ARDS • pulmonary fibrosis • CHF • worsening of arrhythmias • • • • • • inflammation of the liver nausea vomiting constipation dizziness fatigue • • • • • thyroid dysfunction photosensitivity involuntary movement tremors bradycardia • • • • hypotension visual problems discoloration of the skin decreased libido dofetilide (Tikosyn) • dofetilide (Tikosyn) is indicated for the conversion of atrial fibrillation and atrial flutter to normal sinus rhythm • Dosage: • PO: Initial dose is 500 μg bid; maintenance dose is 250 μg bid • It’s most serious adverse effects are ventricular arrhythmias. It’s most common adverse effects are dizziness, headache and chest pain. ibutilide (Corvert) • ibutilide is indicated for the conversion of atrial fibrillation and atrial flutter to normal sinus rhythm, especially within 1 week of bypass surgery. • Dosage: 1 mg infusion, that may be repeated every 10 minute • Dosage after cardiac surgery: 0.5 mg infusion, may be repeated once. • It’s most serious adverse effects are ventricular arrhythmias. It’s most common adverse effects are headache and nausea. 4. Class IV antiarrhythmic drugs • These drugs prevent the movement of calcium into myocardial cells which slows depolarization and decreases the heart rate. • In addition, these drugs decrease the force of myocardial contractions (they would not be recommended in patients with CHF). • ALL CCB’s produce vasodilation, however, only verapamil and diltiazem have direct actions on the heart. • These drugs are effective in treating a variety of arrhythmias including atrial flutter, atrial fibrillation and supraventricular tachycardia • Verapamil (Calan, Verelan, Isoptin) • Diltiazem (Cardizem, Dilacor, Tiazac) • • • • • Adverse effects include: headache Dizziness GI disturbances orthostatic hypotension