Slide 1 - Calgary Emergency Medicine
advertisement

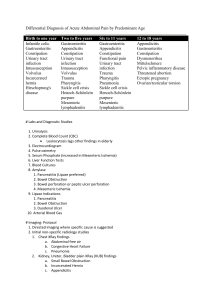
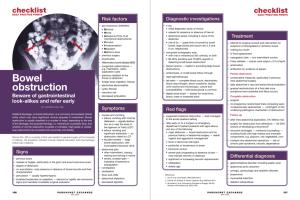
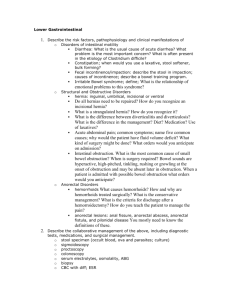
Bowel! Puja Chopra PGY-1 Emergency Medicine Case History: • 50 yo male complains of periumbilical and left lower quadrant abdominal pain that began earlier that day. • Intermittent and crampy pain, accompanied by anorexia and vomiting • Normal BM yesterday • No History of this pain has had prior abdominal surgery …continued Physical Exam: • Afebrile • Moderate distress due to his abdominal pain • Bowel sounds present • Abdomen: mildly distended with periumbilical tenderness but no rebound DDx Small Bowel Obstruction Definitions: • Mechanical obstruction: – Physical barrier to the flow of intestinal contents • Simple Obstruction: – Partial or complete occlusion, proximal intestinal distention, no compromise to blood flow • Closed Loop Obstruction: – Obstruction at two sequential sites, twisting around an adhesion or hernia, higher risk of ischemia • Strangulation: – Vascular compromise to the obstructed area • Adynamic Illeus – Disturbance in gut motility leading to a failure in flow of intestinal contents. Etiologies: abdominal trauma, infection (retroperitoneal, pelvic, intrathoracic), laparotomy, narcotics and other meds, metabolic disease (hypoK), renal colic, MSK inury Etiology • Extraluminal Causes (Most common) – Adhesions • Post pelvic surgery, appendectomy, colorectal surgery – Hernia – Cancer • Intrinsic Causes: – – – – Congenital (stenosis, atresia) Neoplasm Infection from chrones/colitis Intuscception • Intraluminal Causes: – – – – Gallstones Foreign body Barium Cancer • Most common cause: – Adhesions • Most likely to lead to strangulation: – Hernia Pathophysiology Obstruction to intestinal contents occurs: proximal bowel distention, accumulation of fluid and intestinal contents Distention triggers peristalsis above and below the obstruction: early you may have diarrhea Distention triggers fluid release from epithelial secreatory cells perpetuating dilation Loss of ability to reabsorb fluid and electrolytes: dehydration Increased intraluminal pressure, obstruction of lymphatics and capillary flow: edema with eventual loss of mucosal blood supply Increased bacterial proliferation in the small intestine (e coli, streptococcus faecalis, klebsiella) Clinically • History: – Colicky abdominal pain q4-5minutes – Abdominal pain is worse with a proximal obstruction – Nausea and vomiting – Later: obstipation and constipation – Be aware of the pain that changes from intermittent and colicky to constant and severe: intestinal ischemia and perforation • Physical Exam: – Inspection: surgical scars, distended hernia, distended abdomen, peristalsis – Auscultation: early: you may hear high pitched bowel sounds, later you may hear no bowel sounds – Percussion: Tympany – Palpation: Masses – Look for any peritoneal signs Complications of SBO • • • • • • • • Hypovolemia Intestinal ischemia and infarction Peritonitis Sepsis Respiratory distress (due to diaphragm elevation) Reoccurrence Aspiration pneumonia Perforation Imaging Plain Films • 1. Normal small bowel gas pattern: – Absence of small bowel gas or small amounts of gas with up to four variably shaped non-distended loops of small bowel (less than 2.5 cm in diameter) • 2. Abnormal but non-specific gas: – One loop of borderline or mildly distended small bowel (2.5 to 3 cm), with three or more air-fluid levels. – Normal colonic gas pattern • 3. Probable SBO: – Multiple gas or fluid filled loops of dilated small bowel with a moderate amount of colonic gas • 4. Definite SBO: – Dilated gas or fluid filled loops of small bowel in the setting of a gasless colon Supine Limitations to Abdominal Radiography • Negative and non-specific illeus patterns do not exclude the diagnosis – Can be too early thus the colon size and small bowel size are similar – Can be too proximal and thus only a small segment is dilated – Can be too fluid filled to see dilation CT • Recommended when abdo xrays are non diagnostic • Detecting signs of ischemia and closed loop obstruction • When patients have failed conservative treatment • Can detect etiology – thus useful in patients that have not had previous surgery CT for Ischemia Ultrasound ?Strangulation • Fevang et al. Early operation or conservative management of patients with small bowel obstruction – Strangulation diagnosed by physical signs and symptoms including fever, leukocytosis, peritonitis, tachycardia or metabolic acidosis is correct only 45% of the time Strangulation vs Simple • On univariate analysis other factors that made one think of strangulation were: • Hypotension • Acidosis • Elevated BUN • But when put in multivariate analysis this was not proven Management Reoccurrence • There is about a 50% reoccurrence rate after the first small bowel obstruction – Gowen GF, 2003 • There is an 81% reoccurrence rate after 4 obstructive episodes – Fevang et al., 2004 Case 2 Facts • 7% lifetime risk of developing appendicitis • In the ED, 25% of patients younger than 60 yo with acute abdominal pain have appendicitis • In the ED, 4% patients older than 60 yo with acute abdominal pain have appendicitis • Incidence of perforation: 20% • 15 to 35% negative laparotomy rate, rises to 45% in females. Etiology: Acute obstruction (usually secondary to an appendicolith but also can be due to calculus, tumor, parasite or enlarged lmyph node) Acute obstruction will lead to a rise in intraluminal pressure, and mucosal secreations become such that they cannot be drained. This resulting distention will stimulate the visceral affernt pathways and results in a dull poorly localized pain Abdominal cramping may also occur as a result of hyperperistalisi As the intraluminal pressure exceeds the venous pressure leading to necrosis and ischemia of the appendiz Bacteria and polymorphic cells will then invade the appendiceal wall With time the appenix will swell and pain becomes localized to RLQ Typical Presentation Occurs in ????% of cases • Three Findings With a high positive likelihood ratio – RLQ pain: • Sensitivity: 81% • Specificity: 53% • LR+: 7.31, LR-: 0.20 – Rigidity: • Sensitivity: 27% • Specificity: 83% • LR+: 3.76, LR-: 0.82 - Migration: Sensitivity: 64% Specificity: 82% LR+: 3.18, LR-: 0.50 …Ruling out appendicitis? • Signs with Powerful Negative Likelihood Ratios: – Absence of RLQ pain • LR-: 0.20 – Presence of similar previous pain • LR-: 0.50 – Lack of migration of pain • LR-: 0.50 Other Symptoms Symptom Sensitivity Specificity LR+ Pain before vomiting 100% 64% 2.76 Fever 67% 79% 1.94 Anorexia 68% 36% 1.27 Vomiting 51% 45% 0.92 Nausea 58% 37% 0.69-1.20 Other Signs… Sign Sensitivity Specificity LR+ Rebound tenderness 63% 69% 1.10 to 6.30 Guarding 74% 57% 1.65 to 1.78 Rectal tenderness 41% 77% 0.83 to 5.34 Psoas sign 16% 95% 2.38 McBurney’s Point Rovsing Sign Psoas Sign Obturator Sign Suspected Appendicitis Alvarado Score Sensitivity: 92.77% Specificity: 58.18% 1-4 Discharge PPV = 61.82%, NPV = 79.21%; 5-6 Observation/ Investigation 7-10 Surgical consult PPV = 89.16%, NPV = 41.33% The use of the Alvarado score in the management of right lower quadrant abdominal pain in the adult Y. Pouget-Baudry et al. 2010 …but the WBC is normal…they can’t have appendicitis? Imaging • In 50 to 60% of patients the diagnosis of appendicitis can be made clinically • Alvarado score 4-6 ….you can wait and watch, or image Plain X-ray Sensitivity of 28% Specificity of 76% Ultrasound • Used to help confirm the diagnosis of suspected appendicitis • Sensitivity: 86% • Specificity: 81% CT • Used to help confirm the diagnosis of suspected appendicitis • Sensitivity: 95% • Specificity: 94% Benefit of imaging Perforation Treatment • Analgesia – Opioid: • The use of opioid analgesics in the therapeutic diagnosis of patients with AAP does not increase the risk of diagnosis error or the risk of error in making decisions regarding treatment. » Manterola et al. Systematic Review: Analgesia in patients with acute abdominal pain. 2010 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd – NSAIDs: • Retrospective chart review case controlled suggesting that NSAIDs delays treatment » Frei et al. Is early analgesia associated with delayed treatment of appendicitis? American Journal of Emergency Medicine (2008) • IV Fluid • Perioperative Antibiotics: High Index of suspicion required Clinical • Need a high index of suspicion • Ischemia of the viscera: leading to pain out of proportion with findings – – – – Abdominal pain: 83% Vomiting: 44% Diarrhea: 19.3% GI bleeding: 20.1% • Infarction Huang et al. Clinical Factors and Outcomes in Patients with Acute Mesenteric Ischemia in the Emergency Department. July 2003: Acad Emerg Med. Laboratory: • Non-specific • Aid in diagnosis when suspicious • Normal labs do not exclude ischemia Other Tests… • LDH – Sensitivity 70%, Specificity 42%, LR+ 1.2, LR- 0.7 • Lactate – Sensitivity 90%, Specificity 44%, NPV 96%, PPV 70 • Alpha-GST – Sensitivity 72%, Specificity 77%, NPV 86%, PPV 58% • ALP (marker of intestinal mucosal ischemia) – Sensitivity: 80%, Specificity: 64%, LR+ 2.2, LR – 0.3 Predictors of mortality • • • • Bandemia 68.9% sensitive, 74.2% specific Elevated AST 62.1% sensitive, 78.9.% specific Elevated BUN 88.5% sensitive, 39.3% specific Metabolic acidosis: 53.6% sensitive, 85.5.% specific Huang et al. Clinical Factors and Outcomes in Patients with Acute Mesenteric Ischemia in the Emergency Department. July 2003: Acad Emerg Med. Management • 1. Stabilize the patient • 2. Antibiotics – Evidence that survival improved • 3. Heparin • 4. Vasodilators – ? Glucagon • 5. Papaverine • 6. Surgery Glucagon • Vasodilator • Intestinal vasodilator and hypotonicity to reduce oxygen demand • Used if no evidence of peritonitis • Studies in rat’s and dogs have shown improved survival • No studies in humans Papaverine • Phosphodiesterase inhibitor • Improves mesenteric blood flow • Arterial embolic disease or non-occlusive disease • Intra-arterial (60 mg bolus and then 60mg/h infusion) • Survival improvement by 20 to 50% Asymptomatic Diverticulosis • CT scan finds incidental diverculosis • Should we do anything? – Inverse association between dietary fiber intake and the risk of subsequently developing clinically evident diverticular disease Symptomatic Uncomplicated Diverticulitis • History: – LLQ abdominal pain – Better with defecation – Worse with eating – No rebound – No guarding Symptomatic Diverticuli • History: – Low grade fever – Left lower quadrant pain – Colonic dysfunction (bloating, constipation, diarrhea, mucous per rectum) – Signs of obstruction – Signs of colovescial fistula • Physical Exam: – Localized tenderness in the LLQ – Guarding and reboud – Palpable mss Diagnosis • History and Physical Exam • Laboratory: – WBC: can be elevated – Prospective analysis of 226 cases demonstrated that 46% of patients with confirmed diverticulitis had no elevated WBC – Urinanalysis • Rule out UTI or fistula CT • Sensitivity: 93-98% • Specificity: 77% • Water soluble contrast orally and IV • Pro’s: – Therapeutic: percutaneous drainage of abscess (if >4cm) – Determine alternate pathology – Identify complicated diverticulitis Ultrasonography • Sensitivity: 84% to 98% • Specificity: 90 to 93% • Pros: – Avoids radiation – Gyne structures are seen • Cons: – Patients often acutely tender here compression by probe is uncomfortable – Cannot identify perforation/air – Obese patient or overlying gas Endoscopy and MRI: • Not in the ER Complicated Diverticulitis • • • • Abscess (15%) Obstruction (10%) Free Perforation (1%) Fistula (2%) • Diverticular hemorrhage Management • Symptomatic uncomplicated diverticulitis Versus…no antibiotics • Controversy • Most studies showing symptomatic and complication rates benefit from antibiotics versus just bran Acute Diverticulitis • Outpatient – Mild symptoms – No peritonitis – Able to tolerate a clear liquid diet – Close follow-up – Return to ED: increasing pain, fever, inability to tolerate oral fluids Acute Diverticulitis • Inpatients: – Elderly – Immunocompromised – Severe comorbidities – High fever – Significant leukocytosis Antibiotics Rosen’s BOX 93-5 INTRAVENOUS ANTIBIOTIC COVERAGE FOR BOWEL FLORA Mild to Moderate Infection – Ticarcillin-clavulanate, 3.1 g IV q6h – Ampicillin-sulbactam, 3 g IV q6h or – Ciprofloxacin, 400 mg IV q12h, and metronidazole, 1 g IV q12h Severe Infection • Ampicillin, 2 g IV q6h, and metronidazole, 500 mg IV q6h, and (gentamicin, 7 mg/kg q24h, or ciprofloxacin) 400 mg IV q12h or • Imipenem, 500 mg IV q6h Surgery • Emergency: perforation with peritonitis • Non-emergency: fistula, stricture, • Elective: – Recurrent episodes (greater than 2) – Younger than 40 yo (more likely to have severe disease) – Initial attack and immunocompromised Reoccurrence Risk • Reoccurrence rate varies from 7 to 45% and reoccur within a year Sigmoid Volvulus • 859 patients with sigmoid volvulus – – – – 83% were males 17% were females (of which 6.3% were pregnant) Mean symptom duration of 39.4 hours Clinical Triad highly suggestive of SV: Abdominal pain (98.7%), asymmetric abdominal distention (96%), obstipation (92.3%)