Urinary System
advertisement

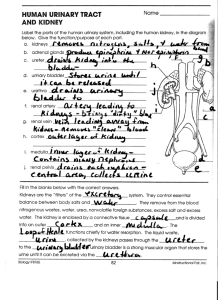
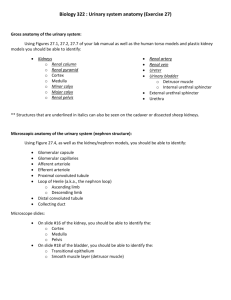
Human Anatomy, First Edition McKinley & O'Loughlin Chapter 27 Lecture Outline: Urinary System 27-1 2 3 4 General Structure and Functions of the Urinary System The kidneys filter waste products from the bloodstream and convert the filtrate into urine. The ureters, urinary bladder, and urethra are collectively known as the urinary tract because they transport the urine out of the body. 27-5 Functions of the Urinary System Removing waste products from the bloodstream. Storage of urine. the urinary bladder is an expandable, muscular sac that can store as much as 1 liter of urine Excretion of urine. Blood volume regulation. the kidneys control the volume of interstitial fluid and blood under the direction of certain hormones Regulation of erythrocyte production. as the kidneys filter the blood, they are also indirectly measuring the oxygen level in the blood 27-6 7 8 9 10 Blood Supply to the Kidney Blood plasma is filtered across the glomerulus into the glomerular space. Once the blood plasma is filtered, blood leaves the glomerulus and enters an efferent arteriole. Note that the efferent arteriole is still carrying oxygenated blood because a gas and nutrient exchange with the kidney tissues has not yet occurred. 27-11 Blood Supply to the Kidney The efferent arterioles branch into one of two types of capillary networks: peritubular capillaries or vasa recta these capillary networks are responsible for the actual exchange of gases and nutrients Peritubular capillaries primarily reside in the cortex of the kidney. Vasa recta surround the thin tubes that project into the medulla. 27-12 13 Nephrons The functional filtration unit in the kidney. Consists of the following components: a renal corpuscle, a proximal convoluted tubule, a nephron loop, and a distal convoluted tubule and are collectively known as the renal tubule Together, both kidneys house approximately 2.5 million nephrons. These microscopic structures measure less than 5 centimeters in total length. 27-14 15 16 17 18 Proximal Convoluted Tubule The proximal convoluted tubule originates at the tubular pole of the renal corpuscle. The cells of the proximal convoluted tubule actively reabsorb almost all nutrients (glucose and amino acids), electrolytes, and any plasma proteins from the tubular fluid. Approximately 60% to 65% of the water in the tubular fluid is reabsorbed by osmosis. The solutes and water are returned to the vascular system via the peritubular capillaries. 27-19 Nephron Loop The nephron loop (loop of Henle) originates at a sharp bend in the proximal convoluted tubule and projects internally toward and into the medulla. Each loop has two limbs. descending limb extending from the cortex toward and into the medulla ascending limb returns back to the renal cortex 27-20 21 22 Distal Convoluted Tubule The distal convoluted tubule originates in the renal cortex at the end of the thick ascending limb of the nephron loop adjacent to the afferent arteriole. The primary function of the distal convoluted tubule is secretion. Its cells secrete ions such as potassium (K+) and acid (H+) into the tubular fluid. Reabsorption of water also occurs here under the influence of two hormones, aldosterone and antidiuretic hormone. 27-23 Collecting Tubules and Collecting Ducts If an individual is well hydrated, the collecting ducts simply transport the tubular fluid into the papillary duct and then into the minor calyx. However, if an individual is dehydrated, water conservation must occur, and more-concentrated urine is produced. ADH may act on the collecting duct epithelium, making it more able to absorb water from the tubular fluid. 27-24 Innervation of the Kidney Each kidney is innervated by a mass of autonomic nervous system fibers collectively called the renal plexus. The renal plexus accompanies each renal artery and enters the kidney through the hilum into the renal sinus. 27-25 Urinary Tract The ureters are long, fibromuscular tubes that conduct urine from the kidneys to the urinary bladder. Each tube averages 25 centimeters in length and is retroperitoneal. The ureters originate at the renal pelvis as it exits the hilum of the kidney, and then extend inferiorly to enter the posterolateral wall of the base of the urinary bladder. The wall of the ureter is composed of three concentric tunics. From innermost to outermost, these tunics are the mucosa, muscularis, and adventitia. 27-26 Urinary Tract – Urinary Bladder The urinary bladder is an expandable, muscular container that serves as a reservoir for urine. It is positioned immediately superior and posterior to the pubic symphysis. In females, the urinary bladder is in contact with the uterus posterosuperiorly and with the vagina posteroinferiorly. In males, it is in contact with the rectum posterosuperiorly and is immediately superior to the prostate gland. The urinary bladder is a retroperitoneal organ. When empty, the urinary bladder exhibits an upside-down pyramidal shape. Filling with urine distends it superiorly until it assumes an oval shape. 27-27 Urinary Tract – Urinary Bladder A posteroinferior triangular area of the urinary bladder wall, called the trigone is formed by imaginary lines connecting the two posterior ureteral openings and the anterior urethral opening. The trigone remains immovable as the urinary bladder fills and evacuates. It functions as a funnel to direct urine into the urethra as the bladder wall contracts to evacuate the stored urine. The four tunics that form the wall of the bladder are the mucosa, submucosa, muscularis, and adventitia. 27-28 29 30 31 Micturition (Urination) The expulsion of urine from the bladder. Initiated by a complex sequence of events called the micturition reflex. The bladder is supplied by both parasympathetic and sympathetic nerve fibers of the autonomic nervous system. 27-32 Urethra Fibromuscular tube that exits the urinary bladder through the urethral opening from its anteroinferior surface and conducts urine to the exterior of the body. The luminal lining of the urethra is a protective mucous membrane that houses clusters of mucin-producing cells called urethral glands. Bundles of primarily smooth muscle fibers surround the mucosa and help propel urine to the outside of the body. Two urethral sphincters restrict the release of urine until the pressure within the urinary bladder is high enough and voluntary activities needed to release the urine are activated. 27-33 Urethra The internal urethral sphincter is the involuntary, superior sphincter surrounding the neck of the bladder, where the urethra originates. a circular thickening of the detrusor muscle and is controlled by the autonomic nervous system The external urethral sphincter is inferior to the internal urethral sphincter and is formed by skeletal muscle fibers of the urogenital diaphragm. a voluntary sphincter controlled by the somatic nervous system this is the muscle children learn to control when they become “toilet-trained” 27-34 35 36 Female Urethra Has a single function: to transport urine from the urinary bladder to the vestibule, an external space immediately internal to the labia minora 3 to 5 centimeters long, and opens to the outside of the body at the external urethral orifice located in the female perineum. 27-37 Male Urethra Urinary and reproductive functions: passageway for both urine and semen Approximately 18 to 20 centimeters long. Partitioned into three segments: prostatic urethra is approximately 3 to 4 centimeters long and is the most dilatable portion of the urethra extends through the prostate gland, immediately inferior to the male bladder, where multiple small prostatic ducts enter it membranous urethra is the shortest and least dilatable portion extends from the inferior surface of the prostate gland through the urogenital diaphragm spongy urethra is the longest part (15 centimeters) encased within a cylinder of erectile tissue in the penis called the corpus spongiosum extends to the external urethral orifice 27-38 Aging and the Urinary System Changes in the size and functioning of the kidneys begin at 30. Gradual reduction in kidney size. Reduced blood flow to the kidneys. Decrease in the number of functional nephrons. Reabsorption and secretion are reduced. Diminished ability to filter and cleanse the blood. Less aldosterone or antidiuretic hormone. Ability to control blood volume and blood pressure is reduced. Bladder decreases in size. More frequent urination. Control of the urethral sphincters—and micturition—may be lost. 27-39 40