Blood Pressure Control - American College of Cardiology
advertisement

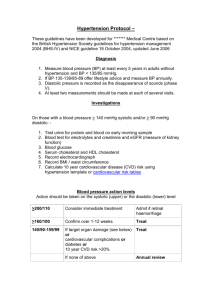
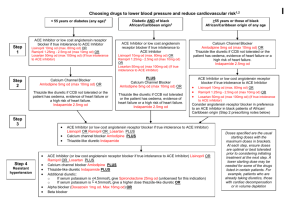
The Evidence for Current Cardiovascular Disease Prevention Guidelines: Blood Pressure Control Evidence and Guidelines American College of Cardiology Best Practice Quality Initiative Subcommittee and Prevention Committee Classification of Recommendations and Levels of Evidence *Data available from clinical trials or registries about the usefulness/efficacy in different subpopulations, such as gender, age, history of diabetes, history of prior myocardial infarction, history of heart failure, and prior aspirin use. A recommendation with Level of Evidence B or C does not imply that the recommendation is weak. Many important clinical questions addressed in the guidelines do not lend themselves to clinical trials. Even though randomized trials are not available, there may be a very clear clinical consensus that a particular test or therapy is useful or effective. †In 2003, the ACC/AHA Task Force on Practice Guidelines developed a list of suggested phrases to use when writing recommendations. All guideline recommendations have been written in full sentences that express a complete thought, such that a recommendation, even if separated and presented apart from the rest of the document (including headings above sets of recommendations), would still convey the full intent of the recommendation. It is hoped that this will increase readers’ comprehension of the guidelines and will allow queries at the individual recommendation level. Icons Representing the Classification and Evidence Levels for Recommendations I IIa IIb III I IIa IIb III I IIa IIb III I IIa IIb III I IIa IIb III I IIa IIb III I IIa IIb III I IIa IIb III I IIa IIb III I IIa IIb III I IIa IIb III I IIa IIb III Evidence for Current Cardiovascular Disease Prevention Guidelines Blood Pressure Evidence High Blood Pressure*: Prevalence Increases with Age Hypertension* Prevalence (%) National Health and Nutrition Examination Survey (NHANES) III 66% 72% 51% 38% 18% 3% 18-29 9% 30-39 40-49 50-59 60-69 70-79 80+ Age The prevalence of high blood pressure increases with age *Hypertension defined as blood pressure >140/90 mmHg or treatment Source: JNC-VI. Arch Intern Med 1997;157:2413-2446 High Blood Pressure*: Prevalence in Different Patient Groups National Health and Nutrition Examination Survey (NHANES) *High blood pressure defined as blood pressure 140/90 mmHg or treatment Source: Yoon SS et al. NCHS Data Brief 2012;107:1-7 High Blood Pressure: Lifetime Risk* Risk of hypertension (%) Framingham Heart Study Men Women Years *Residual lifetime risk of developing hypertension among people with blood pressure <140/90 mmHg starting at age 55-65 years Source: Vasan RS et al. JAMA 2002; 287:1003-1010 Change in Blood Pressure Levels in the United States Over Time Blood pressure age-adjusted percentage National Health and Nutrition Examination Survey (NHANES) Source: Ford ES et al. Figure 2b, Circulation 2009;120:1181-1188 Evidence for Current Cardiovascular Disease Prevention Guidelines Blood Pressure Treatment Evidence and Guidelines JNC VII Guidelines: Measurement of Blood Pressure Method In-office Brief Description Two readings, 5 minutes apart, sitting in chair Confirm elevated reading in contralateral arm Ambulatory BP monitoring Indicated for evaluation of “white-coat” HTN. Absence of 10–20% BP decrease during sleep indicates increased CVD risk Self-measurement Provides information on response to treatment. May help improve adherence to treatment and evaluate “white-coat” HTN BP=Blood pressure, CVD=Cardiovascular disease, HTN=Hypertension Source: Chobanian AV et al. JAMA 2003;289:2560-2572 JNC VII Guidelines: Causes of Secondary Hypertension Medical Conditions Drugs Chronic kidney disease NSAIDs Primary hyperaldosteronism Oral contraceptives Renovascular disease Adrenal steroids Chronic steroid therapy Sympathomimetics Cushing’s syndrome Cyclosporine or tacrolimus Pheochromocytoma Erythropoietin Aortic coarctation Ephedra, mu huang, bitter orange Thyroid or parathyroid disease Cocaine or amphetamines Sleep apnea Alcohol NSAIDs=Non-steroidal anti-inflammatory drugs Source: Chobanian AV et al. JAMA 2003;289:2560-2572 Resistant Hypertension Diagnostic and Treatment Algorithm Confirm Treatment Resistance Office BP >140/90 or 130/80 mm Hg in patients with DM or chronic kidney disease and Patient prescribed 3 or more antihypertensive medications at optimal doses, including if possible a diuretic or Office BP at goal but patient requiring 4 or more antihypertensive medications Exclude Pseudoresistance Identify/Reverse Contributing Lifestyle Factors Obesity Physical inactivity Excessive alcohol ingestion High salt, low fiber diet Discontinue/Minimize Interfering Substances Non-steroidal anti-inflammatory agents Sympathomimetics (diet pills, decongestants) Stimulants Oral contraceptives Licorice Ephedra Is patient adherent with prescribed reigmen? Obtain home, work, or ambulatory BP readings to exclude white coat effect BP=Blood pressure, DM=Diabetes mellitus Source: Calhoun DA et al. Circulation 2008;117:e510-526 Resistant Hypertension (Continued) Diagnostic and Treatment Algorithm Screen for Secondary Causes of Hypertension Obstructive sleep apnea (snoring, witnessed apena, excessive daytime sleepiness) Primary aldosteronism (elevated aldosterone/renin ratio) Chronic kidney disease (CrCl <30 ml/min) Renal artery stenosis (young female, known atherosclerotic disease, worsening renal function) Pheochromocytoma (episodic hypertension, palpitations, diaphoresis, headache) Cushing’s syndrome (moon facies, central obesity, abdominal striae, inter-scapular fat deposition) Aortic coarctation (differential in brachial or femoral pulses, systolic bruit) Pharmacologic Treatment Maximize diuretic therapy, including possible addition of mineralocorticoid receptor antagonist Combine agents with different mechanisms of action Use loop diuretics in patients with chronic kidney disease and/or those receiving potent vasodilators (e.g., minoxidil) Refer to Specialist Refer to appropriate specialist for known or suspected secondary cause(s) of hypertension Refer to hypertension specialist if blood pressure remains uncontrolled after 6 months of treatment CrCl=Creatinine clearance Source: Calhoun DA et al. Circulation 2008;117:e510-526 High Blood Pressure Evidence: Increased Risk with Increased Levels 256 Age at Risk (Y) 80-89 128 70-79 64 60-69 32 50-59 16 40-49 8 4 2 1 0 120 140 160 180 Usual Systolic BP (mm Hg) 256 Ischemic Heart Disease Mortality (Floating absolute risk) Ischemic Heart Disease Mortality (Floating absolute risk) Ischemic heart disease mortality and blood pressure Age at Risk (Y) 80-89 128 70-79 64 60-69 32 50-59 16 40-49 8 4 2 1 0 70 80 90 100 110 Usual Diastolic BP (mm Hg) BP=Blood pressure Source: Prospective Studies Collaboration. Lancet 2002;360:1903-1913 High Blood Pressure Evidence: Risk of CHD with Treatment Veterans Administration, 1967 Veterans Administration, 1970 Hypertension Stroke Study, 1974 USPHS Study, 1977 EWPHE Study, 1985 Coope and Warrender, 1986 SHEP Study, 1991 STOP-Hypertension Study, 1991 MRC Study, 1992 Syst-Eur Study, 1997 0.79 (0.69 to 0.90) Total 0 2.0 0.5 1.5 1.0 Better than placebo Worse than placebo CHD=Coronary heart disease Source: He J et al. Am Heart J 1999;138:211-219 High Blood Pressure Evidence: Number of Medications Needed Trial (SBP Achieved) UKPDS (144 mm Hg) ABCD (127 mm Hg) MDRD (132 mm Hg) HOT (138 mm Hg) AASK (127 mm Hg) 1 1.5 2 2.5 3 3.5 4 Number of BP Meds AASK=African American Study of Kidney Disease and Hypertension, ABCD=Appropriate Blood Pressure Control in Diabetes, BP=Blood pressure, HOT=Hypertension Optimal Treatment, MDRD=Modification of Dietary Protein in Renal Disease, SBP=Systolic blood pressure, UKPDS=UK Prospective Diabetes Study Source: Abbott K et al. J Clin Pharmacology 2004;44:431-438 Blood Pressure Lowering Therapy Evidence: Primary Prevention Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) 33,357 patients with HTN and >1 CHD risk factor randomized to chlorthalidone, amlodipine, or lisinopril for 5 years Rate of MI or fatal CHD .20 Chlorthalidone Amlodipine Lisinopril .16 .12 .08 RR .04 0 0 1 2 (95% CI) P-value A/C 0.98 (0.90-1.07) 0.65 L/C (0.91-1.08) 0.81 3 4 Years to CHD Event 0.99 5 6 7 All three BP lowering agents provide similar efficacy BP=Blood pressure, CHD=Coronary heart disease, HTN=Hypertension, MI=Myocardial infarction Source: ALLHAT Investigators. JAMA 2002;288:2981-2997 Blood Pressure Lowering Therapy Evidence: Primary Prevention Losartan Intervention for Endpoint (LIFE) Reduction in Hypertension Study Proportion with CV death, MI, or stroke (%) 9,193 high-risk hypertensive* patients with LVH randomized to losartan (100 mg) or atenolol (100 mg) for 5 years 16 12 Atenolol Losartan 8 4 13% RRR, P=0.021 0 0 6 12 18 24 30 36 42 48 54 60 66 Study Month An ARB provides greater efficacy in patients with LVH *Defined by SBP=160-200 mmHg or DBP=95-115 mmHg ARB=Angiotensin receptor blocker, CV=Cardiovascular, DBP=Diastolic blood pressure, LVH=Left ventricular hypertrophy, MI=Myocardial infarction, SBP=Systolic blood pressure Source: Dahlöf B et al. Lancet 2002;359:995-1003 Blood Pressure Lowering Therapy Evidence: Primary Prevention Anglo-Scandinavian Cardiac Outcomes Trial—Blood Pressure Lowering Arm (ASCOT-BPLA) Nonfatal MI and fatal CHD (%) 19,342 high-risk hypertensive patients with 3 additional CV risk factors randomized to amlodipine (10 mg) & perindopril (8 mg) or atenolol (100 mg) & bendroflumethiazide (2.5 mg) for 5.5 years 6 Atenolol-based regimen 4 Amlodipine-based regimen 2 RRR=10%, P=0.1052 0 0 1 2 3 4 5 Time since randomization (years) 6 Both BP lowering regimens provide similar efficacy BP=Blood pressure, CV=Cardiovascular, CHD=Coronary heart disease, MI=Myocardial infarction Source: Dahlöf B et al. Lancet 2005;366:895-906 Blood Pressure Lowering Therapy Evidence: Primary Prevention Anglo-Scandinavian Cardiac Outcomes Trial—Blood Pressure Lowering Arm (ASCOT-BPLA) Secondary endpoints Nonfatal MI + fatal CHD Total coronary endpoint Total CV events/procedures All-cause mortality CV mortality Fatal/nonfatal stroke Fatal/nonfatal HF Amlodipinebased rate/1000 patient years 7.4 14.6 27.4 13.9 4.9 6.2 2.5 Atenolol-based rate/1000 patient years Amlodipinebased better Atenololbased better 8.5 16.8 32.8 15.5 6.5 8.1 3.0 P <0.05 <0.01 <0.0001 <0.05 0.001 <0.001 NS 0.50 0.70 1.00 1.45 2.00 An amlodopine-based regimen appears to reduce the rate of other CV events CHD=Coronary heart disease, CV=Cardiovascular, HF=Heart failure, MI=Myocardial infarction Source: Dahlöf B et al. Lancet 2005;366:895-906 Blood Pressure Lowering Therapy Evidence: Primary Prevention Avoiding Cardiovascular Events Through Combination Therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) 11,506 high-risk hypertensive patients randomized to benazepril (40 mg) and amlodipine (10 mg) or benazepril (40 mg) and HCTZ (25 mg) for 36 months* Composite of CV death, MI, stroke, hospitalization for angina, sudden cardiac arrest, and coronary revascularization (%) 0.16 0.14 0.12 Benazepril/HCTZ 0.10 0.08 Benazepril/Amlodipine 0.06 0.04 0.02 20% RRR, HR=0.80, P=0.0002 0.00 0 200 400 600 800 1000 1200 1400 An amlodipine-based regimen provides greater benefit *The study was prematurely stopped CV=Cardiovascular, MI=Myocardial infarction Source: Jamerson K et al. NEJM 2008;359:2417-2428 Blood Pressure Lowering Therapy Evidence: Primary Prevention Hypertension in the Very Elderly (HYVET) Trial Rate/1000 patient years (%) 3,845 patients >80 years with SBP >160 mm Hg randomized to treatment to indapamide (1.5 mg) and perindopril (2-4 mg if needed) vs. placebo for 2 years P=0.02 P<0.001 Indapamide + perindopril Placebo P=0.06 P=0.05 P<0.001 (Primary end point) Blood pressure control in patients >80 years of age provides benefit CV=Cardiovascular, CVA=Cerebrovascular accident Source: Beckett NS et al. NEJM 2008;358:1887-1898 Blood Pressure Lowering Therapy Evidence: Secondary Prevention International Verapamil-Trandolapril Study (INVEST) Incidence of all cause death, nonfatal MI, or nonfatal stroke 22,576 patients with HTN and CAD randomized to a BP lowering strategy with verapamil SR (240 mg) or atenolol (50 mg) for 2.7 years Calcium antagonist strategy (CAS)* Non-calcium antagonist strategy (NCAS)* 20 15 10 5 RR=0.98, P=0.57 0 0 6 12 18 24 30 36 42 48 54 60 Months Both a CAS and NCAS provide similar efficacy *Trandolapril (up to 4 mg) was added in those with diabetes mellitus, chronic kidney disease, or heart failure BP=Blood pressure, CAS=Calcium antagonist strategy, HTN=Hypertension, MI=Myocardial infarction, NCAS=Non-calcium antagonist strategy Source: Pepine CJ et al. JAMA 2003;290:2805-2816 Blood Pressure Lowering Therapy Evidence: Secondary Prevention Valsartan Antihypertensive Long-Term Use Evaluation (VALUE) Trial 15,245 patients with untreated HTN and high CV risk randomized to a BP lowering strategy with valsartan (160 mg) or amlodipine (10 mg) for 4.2 years Primary cardiac composite endpoint Cardiac mortality Cardiac morbidity All myocardial infarction All congestive heart failure All stroke All-cause death New-onset diabetes 0.5 1 2 Favors valsartan Favors amlodipine Both blood pressure lowering regimens provide similar efficacy BP=Blood pressure, CV=Cardiovascular, HTN=Hypertension Source: Julius S et al. Lancet 2004;363:2022-2031 Blood Pressure Lowering Therapy Evidence: Secondary Prevention Comparison of Amlodipine vs Enalapril to Limit Occurrences of Thrombosis (CAMELOT) Trial CV event rate* 1,991 patients with CAD and a DBP <100 mmHg randomized to amlodipine (10 mg), enalapril (20 mg), or placebo for 2 years 0.25 130/78 124/77 125/77 Placebo Enalapril Amlodipine 0.20 0.15 Follow-up BP (mmHg) 0.10 0.05 0 0 6 12 18 24 Months Treatment with amlodipine results in reduced CV events *Includes CV death, myocardial infarction, cardiac arrest, coronary revascularization, hospitalization for heart failure or angina pectoris, stroke, transient ischemic attack, development of peripheral arterial disease BP=Blood pressure, CAD=Coronary artery disease, CV=Cardiovascular, DBP=Diastolic blood pressure Source: Nissen S et al. JAMA 2004;292:2217-2226 Blood Pressure Lowering Therapy Evidence: Effect of Intensive Blood Pressure Control Hypertension Optimal Treatment (HOT) Study Major CV events per 1000 patient-years 18,790 patients with a baseline diastolic BP of 100-115 mm Hg randomized to a target diastolic BP of <90 mm Hg, <85 mm Hg, or <80 mm Hg Patients with Diabetes Patients without Diabetes Diastolic BP goal Diastolic BP goal More intensive blood pressure control provides greater benefit in diabetics BP=Blood pressure, CV=Cardiovascular Source: Hansson L et al. Lancet 1998;351:1755-1762 Blood Pressure Lowering Therapy Evidence: Effect of Intensive Blood Pressure Control Cardio-SIS Trial 1,111 patients >55 years with SBP >150 mm Hg randomized to treatment to achieve usual BP control (SBP <140 mm Hg) or intensive BP control (SBP <130 mm Hg) 21 14 11.4 7 0 Usual Control P=0.003 15 17.0 Composite of CV events* (%) Incidence of LVH (%) P=0.013 Tight Control 10 9.4 4.8 5 0 Usual Control Tight Control More intensive blood pressure control provides greater benefit *Composite of death, MI, CVA, TIA, CHF, angina, new AF, revascularization, aortic dissection, PAD, and ESRD AF=Atrial fibrillation, ESRD=End stage renal disease, CHF=Congestive heart failure, CVA=Cerebrovascular accident, LVH=Left ventricular hypertrophy, MI=Myocardial infarction, PAD=Peripheral artery disease, SBP=Systolic blood pressure, TIA=Transient ischemic attack Source: Verdecchia P et al. Lancet 2009;374:525-533 Blood Pressure Lowering Therapy Evidence: Effect of Intensive Blood Pressure Control International Verapamil-Trandolapril Study (INVEST)—DM Substudy 6,400 diabetic patients from the INVEST study grouped by tight (<130 mm Hg), usual (>130 to <140 mm Hg), or uncontrolled (>140 mm Hg) blood pressure HR=1.15, p=0.036 Tight BP control is not associated with reduced adverse CV events BP=Blood pressure, CV=Cardiovascular Source: Cooper-DeHoff RM et al. JAMA 2010;304:61-68 Blood Pressure Lowering Therapy Evidence: Effect of Intensive Blood Pressure Control Action to Control Cardiovascular Risk in Diabetes (ACCORD) Blood Pressure Trial 4,733 diabetic patients randomized to intensive BP control (target SBP <120 mm Hg) or standard BP control (target SBP <140 mm Hg) for 4.7 years HR=0.88 95% CI (0.73-1.06) HR=0.59 95% CI (0.39-0.89) 15 10 5 0 Patients with Events (%) 20 Total stroke Patients with Events (%) Nonfatal MI, nonfatal stroke, or CV death 20 15 10 5 0 0 1 2 3 4 5 6 7 Years Post-Randomization 8 0 1 2 3 4 5 6 7 8 Years Post-Randomization Intensive BP control in DM does not reduce a composite of adverse CV events, but does reduce the rate of stroke BP=Blood pressure, DM=Diabetes mellitus, HR=Hazard ratio, SBP=Systolic blood pressure ACCORD study group. NEJM 2010;362:1575-1585 JNC VII Guidelines: Management and Treatment Initial drug therapy BP classification SBP* mmHg DBP* mmHg Lifestyle modification Without compelling indications With compelling indications <120 and <80 Encourage Prehypertension 120–139 or 80–89 Yes No antihypertensive drug indicated. Drug(s) for compelling indications.‡ Stage 1 Hypertension 140–159 or 90–99 Yes Thiazide-type diuretics for most. May consider ACE-I, ARB, BB, CCB, or combination of these. 2-drug combination for most† (usually thiazide-type diuretic and ACE-I or ARB or BB or CCB). Drug(s) for compelling indications.‡ Other antihypertensive drugs (as needed). Normal Stage 2 Hypertension >160 or >100 Yes *Treatment determined by highest blood pressure category †Initial combined therapy should be used cautiously in those at risk for orthostatic hypotension ‡Treat patients with chronic kidney disease or diabetes mellitus to blood pressure goal of <130/80 mmHg ACE-I=Angiotensin converting enzyme inhibitor, ARB=Angiotensin receptor blocker, BB=Beta-blocker, BP=Blood pressure, CCB=Calcium channel blocker, DBP=Diastolic blood pressure, SBP=Systolic blood pressure Source: Chobanian AV et al. JAMA 2003;289:2560-2572 JNC VII Guidelines: Lifestyle Modifications for BP Control Modification Recommendation Approximate SBP Reduction Range Weight reduction Maintain normal body weight (BMI=18.525) 5-20 mmHg/10 kg weight lost DASH eating plan Diet rich in fruits, vegetables, low fat dairy and reduced in fat 8-14 mmHg Restrict sodium intake <2.4 grams of sodium per day 2-8 mmHg Physical activity Regular aerobic exercise for at least 30 minutes most days of the week 4-10 mmHg Moderate alcohol <2 drinks/day for men and <1 drink/day for women 2-4 mmHg BMI=Body mass index, BP=Blood pressure, SBP=Systolic blood pressure Source: Chobanian AV et al. JAMA 2003;289:2560-2572 JNC VII Guidelines: Compelling Indications for Drug Classes Compelling Indication Initial Therapy Options Clinical-Trial Basis Heart Failure Diuretic, BB, ACE-I, ARB, Aldo ANT MERIT-HF, COPERNICUS, CIBIS, SOLVD, AIRE, TRACE, Val-HeFT, RALES Post-MI BB, ACE-I, Aldo ANT ACC/AHA Post-MI Guidelines, BHAT, SAVE, Capricorn, EPHESUS High CAD Risk Diuretic, BB, ACE-I, CCB ALLHAT, HOPE, ANBP2, LIFE, CONVINCE Diabetes Mellitus Diuretic, BB, ACE-I, ARB, CCB NKF-ADA Guideline, UKPDS, ALLHAT Chronic Kidney Disease ACE-I, ARB NKF Guidelines, Captopril Trial, RENAAL, IDNT, REIN, AASK Recurrent Stroke Prevention Diuretic, ACE-I PROGRESS ACE-I=Angiotensin converting enzyme inhibitor, Aldo ANT=Aldosterone antagonist, ARB=Angiotensin receptor blocker, BB=Beta-blocker, CAD=Coronary artery disease, CCB=Calcium channel blocker, MI=Myocardial infarction Source: Chobanian AV et al. JAMA 2003;289:2560-2572 JNC VII Guidelines: Blood Pressure Treatment Algorithm Lifestyle modifications Not at goal BP (<140/90 mm Hg) (<130/80 mm Hg for those with diabetes mellitus or chronic kidney disease) Initial drug choices WITHOUT compelling indications Stage 1 hypertension (SBP 140–159 mm Hg or DBP 90–99 mm Hg): Thiazide-type diuretic for most. May consider ACEI, ARB, BB, CCB, or combo. WITH compelling indications Stage 2 hypertension (SBP 160 or DBP 100 mm Hg): Two-drug combination for most (usually thiazide-type diuretic and ACEI or ARB or BB or CCB). Drugs for compelling indications: Other antihypertensive drugs (diuretic, ACEI, ARB, BB, CCB) as needed. Not at goal BP Optimize dosages or add additional drugs until goal BP is achieved. Consider consultation with hypertension specialist. ACEI=Angiotensin converting enzyme inhibitor, ARB=Angiotensin receptor blocker, BB=Beta-blocker, BP=Blood pressure, CCB=Calcium channel blocker, DBP=Diastolic blood pressure, SBP=Systolic blood pressure Source: Chobanian AV et al. JAMA 2003;289:2560-2572 Blood Pressure Recommendations Primary and Secondary Prevention I IIa IIb III Counsel regarding the need for lifestyle modification: weight control; increased physical activity; alcohol moderation; sodium reduction; and emphasis on increased consumption of fresh fruits, vegetables, and low-fat dairy products. Source: Smith SC Jr. et al. JACC 2011;58:2432-2446 AHA Primary Prevention of CV Disease in DM Blood Pressure Recommendations Primary Prevention • BP should be measured at every routine visit. Patients with a SBP >130 mm Hg or DBP >80 mm Hg should have BP confirmed on a separate day. • Patients should be treated to a SBP <130 mm Hg and a DBP <80 mm Hg. • Patients with a SBP of 130-139 mm Hg or a DBP of 80-89 mm Hg should initiate lifestyle modification* alone for a maximum of 3 months. If, after these efforts, targets are not achieved, treatment with pharmacological agents should be initiated. *Includes weight control, increased physical activity, alcohol moderation, sodium reduction, and emphasis on increased consumption of fresh fruits, vegetables, and low-fat dairy products AHA=American Heart Association, BP=Blood pressure, CV=Cardiovascular, DBP=Diastolic blood pressure, DM=Diabetes mellitus, SBP=Systolic blood pressure Source: Buse JB et al. Circulation 2007;115:114-126 AHA Primary Prevention of CV Disease in DM Blood Pressure Recommendations (Continued) Primary Prevention • Multiple-drug therapy is generally required to achieve BP targets. • In elderly hypertensive patients, BP should be lowered gradually to avoid complications. • Orthostatic measurement of BP should be performed when clinically indicated. • Patients not achieving target BP despite multiple-drug therapy should be referred to a physician specializing in the care of patients with hypertension. AHA=American Heart Association, BP=Blood pressure, CV=Cardiovascular, DM=Diabetes Mellitus Source: Buse JB et al. Circulation 2007;115:114-126 ADA Blood Pressure Recommendations for Patients with Diabetes Mellitus Primary Prevention • BP should be measured at every routine DM visit. Patients found to have a SBP >130 mm Hg or a DBP >80 mm Hg should have BP confirmed on a separate day. A repeat SBP >130 mm Hg or a repeat DBP >80 mm Hg confirms a diagnosis of hypertension. • Patients with DM should be treated to a SBP <130 mm Hg. • Patients with DM should be treated to a DBP <80 mm Hg. • Patients with a SBP 130-139 mm Hg or a DBP 80-89 mm Hg may be given lifestyle therapy alone for a maximum of 3 months, and then if targets are not achieved, patients should have pharmacologic agents added. ADA=American Diabetes Association, BP=Blood pressure, DBP=Diastolic blood pressure, DM=Diabetes mellitus, SBP=Systolic blood pressure Source: American Diabetes Association. Diabetes Care 2010;33:S11-61 ADA Blood Pressure Recommendations for Patients with Diabetes Mellitus (Continued) Primary Prevention • Patients with more severe hypertension (SBP >140 mm Hg or DBP >90 mm Hg) at diagnosis or follow-up should receive pharmacologic therapy in addition to lifestyle therapy. • Lifestyle therapy for hypertension consists of weight loss if overweight, DASH-style dietary pattern including reducing sodium and increasing potassium intake, moderation of alcohol intake, and increased physical activity. ACE=Angiotensin converting enzyme, ADA=American Diabetes Association, BP=Blood pressure, DBP=Diastolic blood pressure, DM=Diabetes mellitus, GFR=Glomerular filtration rate, SBP=Systolic blood pressure Source: American Diabetes Association. Diabetes Care 2010;33:S11-61 ADA Blood Pressure Recommendations for Patients with Diabetes Mellitus (Continued) Primary Prevention • Pharmacologic therapy for patients with DM and hypertension should be paired with a regimen that includes either an ACE inhibitor or an ARB. If one class is not tolerated, the other should be substituted. If needed to achieve BP targets, a thiazide diuretic should be added to those with an estimated GFR >30 ml/min and a loop diuretic with an estimated GFR <30 ml/min. • Multiple drug therapy (two or more agents at maximal doses) is generally required to achieve BP targets. ACE=Angiotensin converting enzyme, ADA=American Diabetes Association, ARB=Angiotensin receptor blocker, BP=Blood pressure, DM=Diabetes mellitus, GFR=Glomerular filtrate rate Source: American Diabetes Association. Diabetes Care 2010;33:S11-61 Blood Pressure Recommendations Secondary Prevention I IIa IIb III Use of an ACE inhibitor and/or beta-blocker in those with BP >140/90 mmHg*. Other drugs should be added in order to achieve the desired BP. *A BP >130/80 mmHg should be used for individuals with CKD or DM ACE=Angiotensin converting enzyme, BP=Blood pressure, CKD=Chronic kidney disease, DM=Diabetes mellitus Source: Smith SC Jr. et al. JACC 2011;58:2432-2446 Evidence for Current Cardiovascular Disease Prevention Guidelines Angiotensin Converting Enzyme Inhibitor Evidence and Guidelines ACE Inhibitor: Mechanism of Action Angiotensin II ACE Inactive Fragments Inhibitor Angiotensin I Bradykinin Renin Angiotensinogen Sympathetic Vasopressin Aldosterone Vasoconstriction Kininase II Kininogen Kallikrein tPA Vasodilation Prostaglandins ACE=Angiotensin converting enzyme ACE Inhibitor Evidence: Secondary Prevention Heart Outcomes Prevention and Evaluation (HOPE) Study CV death, MI, or stroke (%) 9,297 patients with DM or vascular disease plus an additional CV risk factor, but without HF or known LVSD randomized to ramipril (10 mg) or placebo for 5 years 0.20 Placebo 0.15 Ramipril 0.10 0.05 22% RRR, P<0.001 0.00 0 500 1000 1500 Days of Follow-Up An ACE inhibitor provides benefit in high-risk individuals ACE=Angiotensin converting enzyme, DM=Diabetes mellitus, CV=Cardiovascular, HF=Heart failure, LVSD=Left ventricular systolic dysfunction, MI=Myocardial infarction Source: HOPE Investigators. NEJM 2000;342:145-153 ACE Inhibitor Evidence: Secondary Prevention European Trial on Reduction of Cardiac Events with Perindopril in Stable Coronary Artery Disease (EUROPA) 12,218 patients with CAD and presumed normal LV function randomized to perindopril (8 mg) or placebo for 4 years Cardiovascular death (0.86; 0.72-1.03) Non-fatal MI (0.78; 0.20-0.90) Cardiac arrest (0.54; 0.20-1.47) Combined endpoint (0.80; 0.71-0.91) 0 0.5 Favors Perindopril 1 2 1.5 Favors Placebo An ACE inhibitor provides benefit in intermediate-risk individuals ACE=Angiotensin converting enzyme, CAD=Coronary artery disease, CV=Cardiovascular, MI=Myocardial infarction Source: EUROPA Investigators. Lancet 2003;362:782-788 ACE Inhibitor Evidence: Secondary Prevention Prevention of Events with Angiotensin Converting Enzyme Inhibition (PEACE) Trial 8,290 patients with stable CAD and normal LV function randomized to trandolapril (4 mg) or placebo for 5 years Primary End Point (%)* 30 Placebo Trandolapril 25 20 15 10 5 0 0 1 2 3 4 5 6 Years After Randomization An ACE inhibitor does not provide benefit in lower-risk individuals *Includes death from cardiovascular causes, myocardial infarction, or coronary revascularization ACE=Angiotensin converting enzyme, CAD=Coronary artery disease, LV=Left ventricular Source: The PEACE Trial Investigators. NEJM 2004;351:2058-2068 ACE Inhibitor Evidence: Secondary Prevention Comparison between the HOPE and PEACE trials MI, Cardiac death, or Stroke (%) HOPE, placebo HOPE, active drug (ramipril) PEACE, placebo Years Patients enrolled in the PEACE trial were lower risk* *Reflects better blood pressure control, revascularization, and use of other risk-reducing medications (i.e., antiplatelet therapy, beta-blocker, lipid-lowering medication) CHD=Coronary heart disease, MI=Myocardial infarction Source: The PEACE Trial Investigators. NEJM 2004;351:2058-2068 ACE Inhibitor Evidence: Secondary Prevention Meta-Analysis of the HOPE, EUROPA, and PEACE Trials* Clinical Trial N HOPE 9,297 Deaths RR of Mortality 1051 HR=0.84 P=0.005 EUROPA 12,218 795 HR=0.89 P=0.10 PEACE 8,290 633 HR=0.89 P=0.13 33,960 >3000 HR=0.86 P<0.001 All Trials 0.4 0.6 0.8 ACE-I Better 1.0 1.2 1.4 1.6 Placebo Better *7 RCTs, 33,960 randomized patients, and 4.4 years of mean follow-up. Other findings include a CV mortality HR=0.81, MI HR=0.82, and stroke HR=0.77 ACE-I=Angiotensin converting enzyme inhihbitor, MI=Myocardial infarction Sources: Danchin N et al. Arch Intern Med 2006;166:787-796 The HOPE Trial Investigators. NEJM 2000;342:145-153 The EUROPA Study. Lancet 2003; 362: 782-788 The PEACE Trial Investigators. NEJM 2004;351:2058-2068 Probability of Event ACE Inhibitor Evidence: Secondary Prevention SAVE AIRE Radionuclide EF <40% Clinical and/or radiographic signs of HF TRACE Echocardiogram EF <35% 0.4 0.35 Placebo 0.3 ACE-I 0.25 0.2 0.15 0.1 OR 0.74 (0.66–0.83) 0.05 0 0 1 2 3 4 Years An ACE-I provides substantial benefit in post-MI LVSD ACE-I=Angiotensin converting enzyme inhibitor, EF=Ejection fraction, LVSD=Left ventricular systolic dysfunction, MI=Myocardial infarction, OR=Odds ratio Source: Flather MD et al. Lancet 2000;355:1575–1581 ACE Inhibitor Recommendations Secondary Prevention I IIa IIb III An ACE inhibitor should be started and continued indefinitely in all patients with left ventricular ejection fraction <40% and in those with hypertension, DM, or CKD, unless contraindicated I IIa IIb III An ACE inhibitor in all other patients ACE=Angiotensin converting enzyme, CKD=Chronic kidney disease, DM=Diabetes mellitus, LVSD=Left ventricular systolic dysfunction Source: Smith SC Jr. et al. JACC 2011;58:2432-2446 AHA Primary Prevention of CV Disease in DM Blood Pressure Recommendations Primary Prevention • Patients with a SBP >140 mm Hg or DBP >90 mm Hg should receive drug therapy in addition to lifestyle and behavioral therapy. • All patients with hypertension should be treated with a regimen that includes an ACE inhibitor or an ARB. If one class is not tolerated, the other should be substituted. Other drug classes* that have been demonstrated to reduce CVD events should be added as needed to achieve BP targets. • If ACE inhibitors, ARBs, or diuretics are used, renal function and serum potassium levels should be monitored within the first 3 months. If stable, follow-up could occur every 6 months. *Includes beta-blockers, thiazide diuretics, and calcium channel blockers ACE=Angiotensin converting enzyme, ARB=Angiotensin receptor blocker, BP=Blood pressure, CV=Cardiovascular, CVD=Cardiovascular disease, DBP=Diastolic blood pressure, DM=Diabetes mellitus, SBP=Systolic blood pressure Source: Buse JB et al. Circulation 2007;115:114-126 ADA Blood Pressure Recommendations for Patients with Diabetes Mellitus (Continued) Primary Prevention • If an ACE inhibitor, ARB, or diuretic is used, kidney function and serum potassium levels should be closely monitored. • In pregnant patients with DM and chronic hypertension, BP target goals of 110-129/65-79 mm Hg are suggested in the interest of long-term maternal health and minimizing impaired fetal growth. • An ACE inhibitor and ARB are contraindicated during pregnancy. ACE=Angiotensin converting enzyme, ADA=American Diabetes Association, ARB=Angiotensin receptor blocker, BP=Blood pressure, DM=Diabetes mellitus Source: American Diabetes Association. Diabetes Care 2010;33:S11-61 Evidence for Current Cardiovascular Disease Prevention Guidelines Angiotensin Receptor Blocker Evidence and Guidelines Angiotensin Receptor Blocker: Mechanism of Action Renin Angiotensinogen Other Pathways AT I Receptor Blocker ATI Angiotensin I Angiotensin II Receptors ACE AT II Receptor Blocker ATII Vasoconstriction Proliferative Vasodilation Action Antiproliferative Action Angiotensin Receptor Blocker Evidence: Secondary Prevention Candesartan in Heart Failure Assessment of Reduction in Mortality and Morbidity (CHARM) Alternative Trial 2,028 patients with symptomatic HF, LVSD (EF <40%), and intolerance to ACE inhibitor randomized to candesartan (32 mg) or placebo for 34 months CV Death or Hospitalization for HF 50 Placebo 40 30 Candesartan 20 10 HR 0.77 p=0.0004 0 0 1 2 Years 3 An ARB provides benefit in those intolerant of an ACE inhibitor ACE=Angiotensin converting enzyme, ARB=Angiotensin receptor blocker, CV=Cardiovascular, EF=Ejection fraction, HF=Heart failure, LVSD=Left ventricular systolic dysfunction Source: Granger CB et al. Lancet 2003;362:772-777 Angiotensin Receptor Blocker Evidence: Secondary Prevention Valsartan in Acute Myocardial Infarction Trial (VALIANT) All Cause Mortality 14,703 patients with post-MI HF or LVSD (EF <0.40) randomized to captopril (50 mg tid), valsartan (160 mg bid), or captopril (50 mg tid) plus valsartan (80 mg bid) for 2 years 0.4 Captopril 0.3 Valsartan Valsartan and Captopril 0.2 0.1 Valsartan vs. Captopril: HR = 1.00; P = 0.982 Valsartan + Captopril vs. Captopril: HR = 0.98; P = 0.726 0.0 0 6 12 18 24 30 36 Months An ARB provides similar efficacy to an ACE inhibitor in Post-MI LVSD ACE=Angiotensin converting enzyme, ARB=Angiotensin receptor blocker, EF=Ejection fraction, LVSD=Left ventricular systolic dysfunction Source: Pfeffer M et al. NEJM 2003;349:1893-1906 Angiotensin Receptor Blocker Evidence: Secondary Prevention Candesartan in Heart Failure Assessment of Reduction in Mortality and Morbidity (CHARM) Added Trial 2,548 patients with symptomatic HF and LVSD (EF <40%) randomized to candesartan (32 mg) or placebo in addition to an ACE inhibitor for 34 months CV Death or Hospitalization for HF 50 40 Placebo 30 Candesartan 20 10 HR 0.85, p=0.011 0 0 1 2 Years 3 Addition of an ARB to an ACE inhibitor may provide benefit in those with LVSD ACE=Angiotensin converting enzyme, ARB=Angiotensin receptor blocker, EF=Ejection fraction, HF=Heart failure, LVSD=Left ventricular systolic dysfunction Source: McMurray JJ et al. Lancet 2003;362:767-771 Angiotensin Receptor Blocker Evidence: Secondary Prevention Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial (ONTARGET) Non-inferiority Margin 25,620 patients with CVD or DM randomized to ramipril (10 mg), telmisartan (80 mg), or a combination of both for 56 months Primary Composite (p = 0.003) CV Death / MI / Stroke / Hospitalization for Heart Failure CV Death / MI / Stroke (HOPE Composite) (p = <0.001) Telmisartan better 0.8 Ramipril better 0.9 1.0 1.1 1.2 RR (95% CI) An ARB provides similar efficacy to an ACE-I in high risk patients ACE-I=Angiotensin converting enzyme inhibitor, ARB=Angiotensin receptor blocker, CVD=Cardiovascular disease, DM=Diabetes mellitus, MI=Myocardial infarction Source: ON TARGET Investigators. NEJM 2008;358:1547-1559 Angiotensin Receptor Blocker Evidence: Secondary Prevention Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial (ONTARGET) 25,620 patients with CVD or DM randomized to ramipril (10 mg), telmisartan (80 mg), or a combination of both for 56 months CV Death, MI, Stroke, or Hospitalization for Heart Failure 0.20 Telmisartan plus ramipril* Telmisartan 0.15 Ramipril 0.10 *Dual RAS blockade leads to greater renal impairment HR=1.33 (p<0.001) 0.05 0.00 0 1 2 3 Follow-up (years) 4 5 Dual RAS blockade provides no additional benefit but leads to greater renal impairment CVD=Cardiovascular disease, DM=Diabetes mellitus, MI=Myocardial infarction, RAS=Renin angiotensin system Source: ON TARGET Investigators. NEJM 2008;358-1547-1559 Angiotensin Receptor Blocker Evidence: Secondary Prevention Telmisartan Randomized Assessment Study in ACE Intolerant Subjects with Cardiovascular Disease (TRANSCEND) 5,926 high risk patients intolerant to ACE inhibitors randomized to telmisartan (80 mg) or placebo for 56 months Percent of patients P=0.055 P=0.216 P=0.048 * An ARB is well tolerated in those unable to take an ACE inhibitor *Primary endpoint is a composite of CV death, MI, stroke or heart failure hospitalization ACE=Angiotensin converting enzyme, ARB=Angiotensin receptor blocker, CV=Cardiovascular, MI=Myocardial infarction Source: TRANSCEND Investigators. Lancet. 2008;372:1174-83 Angiotensin Receptor Blocker Recommendations Secondary Prevention I IIa IIb III An ARB in patients who have HF or who have had a MI with left ventricular ejection fraction <40% and who are ACE-inhibitor intolerant I IIa IIb III An ARB in other patients who are intolerant of an ACE inhibitor I IIa IIb III Use of an ARB in combination with an ACE inhibitor is not well established in those with systolic heart failure ACE=Angiotensin converting enzyme, ARB=Angiotensin receptor blocker, HF=Heart failure, MI=Myocardial infarction Source: Smith SC Jr. et al. JACC 2011;58:2432-2446 AHA Primary Prevention of CV Disease in DM Blood Pressure Recommendations Primary Prevention • Patients with a SBP >140 mm Hg or DBP >90 mm Hg should receive drug therapy in addition to lifestyle and behavioral therapy. • All patients with hypertension should be treated with a regimen that includes an ACE inhibitor or an ARB. If one class is not tolerated, the other should be substituted. Other drug classes* that have been demonstrated to reduce CVD events should be added as needed to achieve BP targets. • If ACE inhibitors, ARBs, or diuretics are used, renal function and serum potassium levels should be monitored within the first 3 months. If stable, follow-up could occur every 6 months. *Includes beta-blockers, thiazide diuretics, and calcium channel blockers ACE=Angiotensin converting enzyme, ARB=Angiotensin receptor blocker, BP=Blood pressure, CV=Cardiovascular, CVD=Cardiovascular disease, DBP=Diastolic blood pressure, DM=Diabetes mellitus, SBP=Systolic blood pressure Source: Buse JB et al. Circulation 2007;115:114-126 ADA Blood Pressure Recommendations for Patients with Diabetes Mellitus (Continued) Primary Prevention • If an ACE inhibitor, ARB, or diuretic is used, kidney function and serum potassium levels should be closely monitored. • In pregnant patients with DM and chronic hypertension, BP target goals of 110-129/65-79 mm Hg are suggested in the interest of long-term maternal health and minimizing impaired fetal growth. • An ACE inhibitor and ARB are contraindicated during pregnancy. ACE=Angiotensin converting enzyme, ADA=American Diabetes Association, ARB=Angiotensin receptor blocker, BP=Blood pressure, DM=Diabetes mellitus Source: American Diabetes Association. Diabetes Care 2010;33:S11-61 Evidence for Current Cardiovascular Disease Prevention Guidelines Beta-blocker Evidence and Guidelines Beta-blocker: Targets and Receptor Selectivity Heart Inotropy Chronotropy Dromotropy + + + _ a2 b1 b2 a1 M2 b1 selective blocker b non-selective blocker b non-selective blocker with a1 blocking activity Parasympathetic Nerve Terminal NE _ _ Blood Vessel a2 _ NE NE + M2 b2 a2 Vasoconstriction a1 Vasoconstriction b2 Vasodilation M2 Vasodilation Sympathetic Nerve Terminal ACh Sympathetic Cholinergic Nerve Terminal a=Alpha receptor, Ach=Acetylcholine, b=Beta receptor, M=Muscarinic receptor, NE=Norepinephrine Source: Klabunde, RE (ed) Cardiovascular Physiology Concepts LWW 2001 Beta-blocker Evidence: Secondary Prevention Placebo-controlled post-MI trials* using oral beta-blockers Study Patient s (N) Göteborg Study† 1,395 Metoprolol tartrate 3 months 36% (P.03) PNS Timolol Trial (Norwegian) 1,884 Timolol 17 months 39% (P.003) 28% (P.0005) Lopressor Intervention Trial 2,395 Metoprolol tartrate 12 months PNS NA Beta-blocker Heart Attack Trial 3,837 Propranolol 25 months 26% (P.005) PNS CAPRICORN Trial 1,959 Carvedilol 15 months 23% (P=.03) 40% (P.01) Treatment Groups Duration of Follow-Up Effect on Mortality Effect on Reinfarction *Includes the largest trials performed to date received IV followed by oral metoprolol †Patients MI=Myocardial infarction, NA=Not applicable, NS=Not significant Beta-blocker Evidence: Secondary Prevention Summary of secondary prevention trials of beta-blocker therapy Phase of Treatment Total # Patients RR (95% CI) Acute treatment 28,970 0.87 (0.77-0.98) Secondary prevention 24,298 0.77 (0.70-0.84) Overall 53,268 0.81 (0.75-0.87) 0.5 1.0 RR of death Beta-blocker Placebo better better 2.0 CI=Confidence interval, RR=Relative risk Source: Antman E, Braunwald E. Acute Myocardial Infarction. In: Braunwald E, Zipes DP, Libby P, eds. Heart Disease: A textbook of Cardiovascular Medicine, 6th ed., Philadelphia, PA: W.B. Sanders, 2001, 1168. Beta-blocker Evidence: Benefit in HF and/or LVSD Study Drug HF Severity Patients (n) Follow-up Mean Dosage Effects on Outcomes CIBIS Bisoprolol* ModerateSevere 641 1.9 Years 3.8 mg/day All cause mortality (p=NS) CIBIS-II Bisoprolol* ModerateSevere 2,647 1.3 Years 7.5 mg/day All cause mortality 34% (P<0.0001) BEST Bucindolol* ModerateSevere 2,708 2.0 Years 152 mg/day All cause mortality (p=NS) MERIT-HF Metoprolol succinate# MildModerate 3,991 1.0 Years 159 mg/day All cause mortality 34% (P=0.0062) MDC Metoprolol tartrate* MildModerate 383 1.0 Years 108 mg/day Death or Need for TX (P=NS) CAPRICORN Carvedilol Mild 1,989 1.3 Years 40 mg/day All cause mortality 23% (P =0.03) US Carvedilol Carvedilol MildModerate 1,094 0.5 Years 45 mg/day All-cause mortality† 65% (P=.0001) COPERNICUS Carvedilol Severe 2,289 0.9 Years 37 mg/day All-cause mortality 35% (P =0.0014) SENIORS Nebivolol Moderate 2,128 3.0 Years 7.7 mg/day All-cause mortality or CV hospitalization 14% (P =0.039) *Not an approved indication, †Not a planned end point #Not approved for severe HF/mortality reduction alone HF=Heart failure, LVSD=Left ventricular systolic dysfunction, NS=Not significant, TX=Transplant Beta-Blocker Recommendations Secondary Prevention I IIa IIb III Beta-blocker should be used in all patients with LVSD (ejection fraction <40%) with HF or prior MI, unless contraindicated*. (Use should be limited to carvedilol, metoprolol succinate, or bisoprolol, which have been shown to reduce mortality.) I IIa IIb III Beta-blocker for 3 years in all patients with normal left ventricular function who have had a MI or ACS I IIa IIb III Beta-blocker beyond 3 years as chronic therapy in all patients with normal left ventricular function who have had a MI or ACS *Relative contraindications include asthma, chronic obstructive pulmonary disease, insulin dependent diabetes mellitus, severe peripheral arterial disease, and a PR interval >0.24 seconds ACS=Acute coronary syndrome, HF=Heart failure, LVSD=Left ventricular systolic dysfunction, MI=Myocardial infarction Source: Smith SC Jr. et al. JACC 2011;58:2432-2446 Beta-Blocker Recommendations (Continued) I IIa IIb III Secondary Prevention Beta-blocker in patients with LVSD (ejection fraction <40%) without HF or prior MI I IIa IIb III Beta-blocker as chronic therapy for all other patients with coronary or other vascular disease HF=Heart failure, LVSD=Left ventricular systolic dysfunction, MI=Myocardial infarction Source: Smith SC Jr. et al. JACC 2011;58:2432-2446