The Urinary System - Mater Academy Lakes High School
advertisement

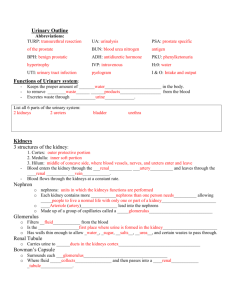
The Urinary System * * * * Urinary System Functions 3 main functions: Excretion – _____________________________________________________________________ Elimination – ___________________________________________________________________ ______________________________________________________________________________ 4 other essential homeostatic functions: Regulating blood volume and pressure Helping to stabilize blood pH Conserving valuable nutrients Parts/Path of the Urinary Tract _______________ produce urine Urine travels though the _______________ to the urinary bladder The _______________ _______________ stores urine until you are ready for excretion Urine leaves the urinary bladder through the _______________ and exits the body The Kidneys The right kidney sits slightly lower than the left Each kidney is covered by a fibrous capsule and is packed is a cushion of adipose tissue (fat) Typically reddish-brown in color and about 4in long Indentation along the medial side called the _______________ that is the site of exit for the ureter and renal vein and the site of entrance for the renal artery and nerve Sectional anatomy ______________________________ ______________________________ Contains 6-18 renal pyramids (______________________________________________) The tip of each pyramid is the renal papilla Urine is discharged into the minor calyx from the renal papilla 4-5 minor calyces join to form the 2 major calyces The 2 major calyces join to form the renal pelvis (connected to the ureter) The Kidneys – The Nephron _____________________________________________________________________________________ ______________________________________________________________________________ 2 types: cortical (in the cortex) and juxtamedullary (near the medulla) Begins at the renal corpuscle – a round structure consisting of the glomerular (______________) capsule and a capillary network (_______________) within separated by capsular space Blood pressure forces fluid and dissolved solutes out of the capillaries and into the surrounding capsular space. _________________________________________________________________ The advantage of filtration is that it is passive, so it requires no energy expense. However, its large pores allow needed ions and nutrients to escape Filtrate then enters the renal tubule 3 parts: ________________________________________________________________________ As filtrate travels through it changes composition and becomes tubular fluid The job of the renal tubule is to reabsorb all of the useful organic molecules from filtrate, _______________________________________________, and secrete waste products that were missed by the filtration process ________________________________________________________________________ Finally empties into the collecting system Many nephrons release tubular fluid into a collecting duct and then several collecting ducts merge to form a papillary duct, which deliver urine to a minor calyx Blood supply to the kidneys Every minute about _______________ of the cardiac output of blood flows through the kidneys Urine Formation _____________________________________________________________________________________ The excretion of urea, creatinine, and uric acid is especially important in this process The kidneys must concentrate urine to avoid large amounts of water loss To do this the kidneys must perform 3 processes: _______________ – blood pressure forces water across the filtration membrane in the renal corpuscle. Solute molecules small enough to pass through the membrane are carried into the filtrate with water _______________ – this is the removal of water and solute molecules from the filtrate and their reentry into the circulation at the peritubular capillaries _______________ – the transport of solutes from the paratubular capillaries, across the tubular epithelium, and into the filtrate Summary of Kidney Function & Urine Formation Step 1 - ______________________________________________________________________________ Step 2 - In the PCT 60-70% of the water and almost all of the dissolved nutrients are reabsorbed Step 3 - From the PCT going towards the loop of Henle, water moves into surrounding interstitial fluid and then into the peritubular capillaries, leaving a small volume of highly concentrated tubular fluid Step 4 - Going from the loop to the DCT, tubular cells actively pump sodium and chloride ions out of tubular fluid Step 5 - Final concentration and composition of tubular fluid is determined in the DCT Step 6 - Concentration of urine is determined Step 7 - ______________________________________________________________________________ Glomerular Filtration Rate (GFR) _____________________________________________________________________________________ GFR is regulated in 3 ways: 1. Local, automatic adjustments in glomerular pressures ________________________________________________________________________ 2. Activities of the sympathetic division of the ANS Primarily shift blood flow away from the kidneys, lowering the GFR and slowing the production of filtrate 3. The effects of various hormones (long-term adjustments) 4 main hormones: _________________________________ o Vasoconstriction in capillary beds, constriction of efferent arterioles in the nephron, triggers release of ADH, and stimulates secretion of aldosterone _________________________________ o Increases water permeability in the DCT and collecting duct o Induces sensation of thirst _________________________________ o Stimulates reabsorption of sodium ion and secretion of potassium ion * * * * _________________________________ o Decreases sodium ion reabsorption, increasing sodium ion loss in urine o Dilation of glomerular capillaries, increasing urinary water loss * * * * * The Ureters _____________________________________________________________________________________ Begins at the renal pelvis and ends at the posterior wall of the bladder Ureteral openings are slit-like to prevent the backflow of urine into the ureters or kidneys when the bladder contracts The Urinary Bladder _____________________________________________________________________________________ Can hold up to a liter or urine Trigone Smooth triangular area outlined by the openings for the ureters and the urethra ______________________________________________________________________________ Collapses when empty; rague will appear Bladder neck is surrounded by internal urethral sphincter which provides involuntary control over discharge of urine from the bladder Contraction of the _________________ compresses the bladder and expels its contents into the urethra The Urethra Extends from the neck of the urinary bladder to the exterior (________________________) of the body Where the urethra passes through the floor of the pelvic cavity, a band of skeletal muscle forms the external urethral sphincter (_______________________________) The micturition (_____________________) reflex Stretch receptors are stimulated as the bladder fills with urine and these impulses are carried to the sacral spinal cord These sensations are then relayed to the cerebral cortex and we become aware of pressure within our urinary bladder ______________________________________________________________________________ ______________________________________________________________________________ If volume reaches 500mL, sphincters are forced open Fluid, Electrolyte, and Acid-Base Balance Treatment of any serious illness affecting the nervous, cardiovascular, respiratory, urinary, or digestive system must always include steps to restore normal fluid , electrolyte, and acid-base balance Water is essential for life; if water content in the body declines too far, cellular activities are jeopardized ______________________________________________________________________________ ______________________________________________________________________________ Homeostasis of fluid volumes, solute concentrations, and pH involves 3 interrelated factors: ____________________ – involves regulating water in the ECF and ICF ____________________ – gained in food/water & lost through urine, sweat, and feces ____________________ – exists when the pH of body fluids is within normal limits Fluid Balance Water moves out of plasma and into interstitial spaces via capillary beds and moves back and forth across epithelial surfaces Fluid shifts – __________________________________________________________________________ Occur relatively rapidly, reaching equilibrium within minutes/hours ______________________________________________________________________________ * * * * Electrolyte Balance Electrolyte balance is important because: A gain/loss of electrolytes can cause a gain/loss of water The concentration of individual electrolytes affects a variety of cell functions Na+ and K+ are major contributors to osmotic concentrations and directly affect normal functioning cells ______________________________________________________________________________ ______________________________________________________________________________ Acid-Base Balance The pH of your body fluids represents a balance among the acids, bases, and salts in solution (pH of the ECF is between 7.35-7.45) ______________________________________________________________________________ ______________________________________________________________________________ Acids in the body Carbonic acid (H2CO3) is important in the body, it gets broken down into CO2 and H2O In peripheral tissues, the CO2 interacts with H2O again to form H2CO3 which then dissociates into H+ and HCO3 ________________________________________________________________________ This reaction occurs spontaneously but can be rapid in the presence of carbonic _________ (an enzyme) Because of how this reaction proceeds, ___________________________________________ (PCO2 is the most important factor affecting pH in body tissues) Buffers and buffer systems _____________________________________________________________________________________ The body has 3 major buffer systems: Protein buffer systems – __________________________________________________________ Depend on amino acid side groups(either –COOH or –NH2) to give/receive hydrogen ions Carbonic acid-bicarbonate buffer systems – ___________________________________________ Primary role is to prevent pH changes caused by metabolic acids Phosphate buffer systems – _______________________________________________________ Consists of an anion, __________________________________ (H2PO4-), which is a weak acid that dissociates into a hydrogen ion and ____________________________ (HPO42-) Maintaining acid-base balance Because buffer systems do not eliminate the excess hydrogen ions, they provide only a temporary solution. For homeostasis to maintain balance, the captured hydrogen ions must be removed. The problem is that buffer supply is low _____________________________________________________________________________________ Respiratory and renal mechanisms support buffer systems by: ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ Respiratory contributions to pH regulation ______________________________________________________________________________ Occurs when pH exceeds normal limit Has a direct effect on the carbonic acid-bicarbonate buffer system Renal contributions to pH regulation ______________________________________________________________________________ ______________________________________________________________________________