Fine_IBD and age
advertisement

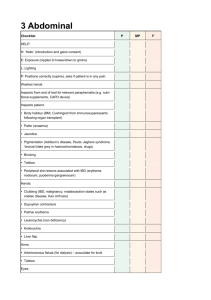
Inflammatory Bowel Disease in the Elderly Steven N. Fine, MD Chief of GI, MetroWest Med Cntr Med Director, Boston Endo Cntr IBD and aging Are there differences between older and younger patients with IBD? What are the differences? What are the similarities? How do we alter our approach to treatment? IBD and aging Is there a difference between developing IBD at an advanced age versus having IBD at a young age and growing older? Take Home Point #1 The onset of IBD at an advance age occurs more frequently than previously thought. Epidemiology Incidence varies from 3.1-14.6 cases per 100,000 for CD and 2.2-14.3 for UC Incidence of CD after age 60 is 3.5-4.0 per 100,000 Incidence of UC after age 60 is 4.5-8.0 per 100,000 Loftus EV. Gastroenterol Clin N Am 2002; 31:1-20 Robertson DJ. Gastroenterol Clin N Am 2001; 30:409-26 Evans PE. Aging Health 2007; 3:77-84 Epidemiology The onset of CD occurs after age 60 in 16% of patients (range: 7-26%) The onset of UC occurs after age 60 in 12% of patients (range: 8-20%) 65% in 60s, 25% in 70s, 10% in 80s Loftus EV. Gastroenterol Clin N Am 2002; 31:1-20 Robertson DJ. Gastroenterol Clin N Am 2001; 30:409-26 Evans PE. Aging Health 2007; 3:77-84 Take Home Point #2 The burden on the health care system from older IBD patients is rising. Epidemiology: National Hospital Discharge Survey Using data from NHDS Age-specific rates of hospitalization over consecutive 5-year periods Found more pronounced increase in rates of hospitalization for older age group (65+) Sonnenberg A. J Clin Gastroenterol 2009; 43:297-300 US Hospitalization: Crohn’s 700 600 500 65+ 45-64 -44 400 300 200 100 0 1970- 1975- 1980- 1985- 1990- 1995- 2000- 20054 9 4 9 4 9 4 6 US Hospitalizations: UC 600 500 400 65+ 45-64 -44 300 200 100 0 1970-4 1975-9 1980-4 1985-9 1990-4 1995-9 2000-4 Take Home Point #3 IBD at an advanced age has a less aggressive natural history and a different distribution at presentation. Natural History Northern France, EPIMAD Registry 1988-2006; 6 million people; 9.3% of pop 3 Academic and 27 Regional Hospitals 262 Gastroenterologists Largest population-based study of elderlyonset IBD reported to date. Charpentier C. Gut 2014; 63:423-432. IBD and age: Northern France Study IBD and age: distribution at presentation IBD and age: Natural History For Crohn’s: disease extension in 31% for <17 years vs 8% for >60 years For Ulcerative Colitis: disease extension in 49% for <17 years vs 16% for >60 years Charpentier C. Gut 2014; 63:423-432 Long-Term Course of Crohn’s Disease Probability of remaining FREE of complications N = 2002 patients with Crohn’s disease since diagnosis of the disease 100 Cumulative Probability (%) 90 80 70 60 Penetrating 50 40 30 Inflammatory Stricturing 20 10 0 0 12 24 36 48 60 72 84 96 108 120 132 144 156 168 180 192 204 216 228 240 Months These data precede biologic therapy for Crohn’s disease Cosnes J et al. Inflammatory Bowel Disease. 2002;8:244–250. CD: Evolution of behavior from diagnosis to maximal follow-up Proportions of behaviors according to disease duration Clinical Course Elderly-onset patients (>60 yrs at diagnosis) 5% 17% Penetrating Stricturing 10% 22% 78% Inflammatory 68% Pediatric-onset patients (<17 yrs at diagnosis) Northern France Study Conclusion: “Clinical course is mild in elderly-onset IBD patients. This information would need to be taken into account by physicians when therapeutic strategies are established.” Charpentier C. Gut 2014; 63:423-432 CD diagnosed at a young age: Natural History No difference in activity 3 years after dx compared with 20 years after dx 24% of Crohn’s patients had active disease 20 years later 48% in remission on treatment 28% in remission off treatment Crohn’s Disease does not “burn out” Etienney I. Gastroenterol Clin Biol 2004; 28: 1233-9 IBD at advanced age Relapses less likely Fewer post-surgical recurrence 1st episode of UC more fulminant and more likely to require surgery Acute abdomen more common in CD Lower frequency of FHx of IBD Wagtmans MJ. J Clin Gastroenterol 1998; 27:129-33 Harper PC. Arch Int Med 1986; 146: 753-5 Softley A. Scand J Gastroenterol 1988; 23:27-30 Triantafillidis JK. Digest Liver Dis 2000; 32:498-503 Polito JM. Gastroenterology 1996; 111:580-6 IBD at advanced age Colonic involvement is more likely Overall less risk for surgery Less risk for progression Less fistulizing disease Gisbert JP. Aliment Pharmacol Ther 2014; 1-19 Ha C. Curr Gastroenterol Rep 2013; 15: 310 (1-9) IBD and the Elderly: Mortality Prospective study 20 geographic areas in 12 European countries 2201 IBD patients 10 year clinical follow up Wolters FL. Gut 2006; 55:510-8 IBD and the Elderly: Mortality Increased mortality risk in patients with Crohn’s Disease 10 years after diagnosis Above 40 years at diagnosis was the sole factor associated with increased mortality Wolters FL. Gut 2006; 55:510-8 IBD and the Elderly: Mortality Age is an independent predictor of mortality in IBD inpatients Malnutrition, male sex, need for surgery were factors associated with higher risk In IBD, elderly age predictive of mortality with an odds ratio of 3.91 Ananthakrishnan A. Dig Dis 2009; 27: 327-34 Ananthakrishnan A. Inflamm Bowel Dis 2009; 15: 182-9 Take Home Point #4 Comorbidities and polypharmacy affect outcome, morbitity and mortality. Katz S. Inflamm Bowel Dis 2013; 19: 225772. Ha C. Curr Gastroenterol Rep 2013; 15: 310 (1-9). Kaplan GG. Arch Surg 2011; 146: 959-964. Comorbid Conditions CAD 33.8% CLD 22.6% CHF 22.6% PVD 7.4% CVD 12.5% PUD/GIB 17.8% Mod-sev Liver 10.7% DM 18.8% DM and end-org 9.4% CVA 12.5% Mod to sev RD 11.5% Rheum 10.2 % Dementia 2.5% HIV 0.5% Polypharmacy 128 IBD pts greater than 65 yo Average of 9.5 routine medications >10 meds (severe polypharmacy) associated with comorbidity scores and steroid use 80% of pts had at least one medication interaction, 63% involved IBD therapy. Parian AM. DDW 2013: Su1130 !" #$%&' %( )$*' +), -)! "# $% &&% ' % () #*" -%#.*, " ) Clinical Course Take Home Point #5 Look for, prophylax for, and treat C.difficile and venous thromboembolism. Risk Factors for Osteoporosis in IBD Medications Advanced age Low body mass Reduced physical activity Family History of Osteoporosis TOB Ali T. Am J Med 2009; 122: 599-604 AGA Recommendations for Managing Osteoporosis T score >-1 IBD patient: Any of: -Prolonged steroid use (>3mo consec or recurrent courses) -Low trauma, fragility fracture -Postmenopausal or male age >50 -Hypogonadism T score -2.5 to -1 DXA T score <-2.5 Vert Fracture Regardless of DXA Gastroenterology 2003;124:795-841 Basic Prevention: -Ca/Vit D -exercise -smoking cessation -avoid alcohol -minimize corticosteroids -treat hypogonadism Prevention and: -repeat DXA 2 years -Prolonged CS consider BP and DXA 1 year Prevention and: -Screen other causes low BMD -Bisphosphonate therapy or -Refer to bone specialist Adherence to Guidelines Survey 1000 AGA members 304 responders; 258 appropriate 49% utilized guidelines Wagnon J. Inflam Bowel Dis 2009; 15: 1082-1089 Reasons for Non-Utilization Adherence to Guidelines Retrospective study George Washington University 26.5% had DEXA 13.7% had vitamin D testing Less than half ordered by GI MDs 35.7% had vitamin D deficiency Bakshi A. Am J Gastroenterol 2009; 104: 791. Adherence to Guidelines Retrospective George Washington University Men with IBD 9% had vitamin D testing 21.5% had DEXA 65% had either osteoporosis or osteopenia Nguyen HD. Am J Meds Health 2010; 4: 71-4. Take Home Point #6 IBD patients over age 50 should have Bone Density Testing and then follow-up depending on results (follow the guidelines) IBD and the Elderly: Surgery Rate of early surgery for fulminant disease for UC higher in elderly; after 5 years for young Surgery for CD in elderly with higher mortality rate and complications 8-fold increase in post-op mortality (perf/sepsis) As the number of comorbidities increase, postoperative mortality increases Greenwald DA. Curr Treat Options in Gastro 2003; 6:213-225 Almony G. Scand J Gastroenterol 2002; 37:1025-28 Juneja M. Dig Dis Sci 2012; 57:2408-15 Guy TS. Surg Clin North Am 2001; 81:159-168 Kaplan GG. Arch Surg 2011; 146: 959-964 IBD in the Elderly: Surgical Outcomes Medical College of Wisconsin IBD surgeries in patients after 65 yo Compared with 3 control groups: 18-35 yo, 36-49 yo, 50-64 yo No difference in complication rate. Comorbidity Index and nutritional status are risk factors. Bautista MC. Dig Dis Sci 2013; 58:2955-62 IBD and the Elderly: Ileal Pouch-Anal Anastomosis Mayo Clinic 2002 pts IPAA for UC or FAP Over a 9 year period Question: does age affect surgical outcome? Chapman JR. Arch Surg 2005; 140:534-40 IBD and the Elderly: Ileal Pouch-Anal Anastomosis No increase in pouch failure in the elderly Increase in incontinence No difference in quality of life Chapman JR. Arch Surg 2005; 140:534-40 Take Home Point #7 There is less tendency for surgery in the elderly, but worse outcomes; and comorbid conditions and nutritional status are risk factors for poor surgical outcomes. Fit Elderly and Frail Elderly concept for individualizing therapy walker, wheelchair, falls, polypharmacy, comorbidities, oxygen, cognitive function, level of activity help to define risk. guide therapeutic decisions. no scientific studies. Katz S. Inflamm Bowel Dis 2013; 19: 2257-72 Katz S. Gastroenterol & Hep 2008; 4: 337-47 IBD and the Elderly: 5-ASA More attention may be needed for patients with chronic renal insufficiency and 5-ASA Exacerbations of the IBD may increase risk due to dehydration and pre-renal state Half-life is increased in elderly Interactions with warfarin and 6MP/AZA Katz S. Inflamm Bowel Dis 2013; 19: 2257-72 Gisbert JP. Inflamm Bowel Dis 2007; 13:629-38 Katz S. Gastroenterol & Hep 2008; 4:337-47 IBD and the Elderly Antibiotics Neuropathic effects of metronidazole Effects on warfarin Cdifficile Greenwald DA. Curr Treat Option Gastroenterol 2003; 6:213-25 Katz S. Gastroenterol & Hep 2008; 4:337-47 Katz S. Inflamm Bowel Dis 2013; 19: 2257-72 IBD and the Elderly: Steroids Infection Osteoporosis Mental status Depression HTN DM Katz S. Gastroenterol & Hep 2008; 4: 337-47 Hypertension Hypokalemia Hyperglycemia Osteonecrosis CHF Consider budesonide IBD and the Elderly: Methotrexate Decrease in GFR impacts on drug clearance Effects on warfarin May increase atherosclerosis and cardiovascular mortality by increasing levels of homocysteine Increase risk of osteoporosis Katz S. Inflamm Bowel Dis 2013; 19: 2257-72 Landewe RBM. Lancet 2000; 355:1616-7 Greenwald DA. Curr Treat Options Gastro 2003; 6:213-225 IBD and the Elderly: 6MP/Azathioprine Myelosuppression is unrelated to age Significant dose reduction if used with allopurinol; inhibit warfarin effect Use TPMT enzyme activity and Thiopurine metabolites to guide therapy MTX to avoid risk of Lymphoma/Skin Ca Present DH. Ann Int Med 1989; 111:641-9 Connell WR. Gut 1993; 34:1981-5 O’Brien JJ. Gastroenterology 1991; 101:39-46 CESAME Incidence rates of lymphoproliferative disorders according to thiopurine exposure grouped by age at entry in the cohort Beaugerie L et al. Lancet 2009 Take Home Point #8 6MP/AZA pose a significant risk of lymphoproliferative disorders in the elderly, so methotrexate may be a better option. IBD and the Elderly: Anti-TNFs Evaluated the safety of infliximab in older pts (70 yo) Used infliximab withdrawal and the reason for withdrawal as outcome 9 hospitals around Burgundy, France 83 pts (RA and AS) Chevillotte-Maillard H. Rheumatology 2005; 44:696-7 IBD and the Elderly: Anti-TNFs 14 12 10 8 20-40 41-60 60+ 6 4 2 0 % infections IBD and the Elderly: Anti-TNFs Northern Ireland 94 patients Severe inflammatory arthritis Mean age of pts with major infections was 65 yo Cairns AP. The Ulster Medical Journal 2002; 71: 101-5 IBD and the Elderly: Anti-TNFs Mayo Clinic experience 500 patients; Crohn’s Disease 1% mortality 3 of the 5 attributable deaths were associated with “relatively old age” and “severe comorbidities” Colombel J. Gastroenterlogy 2004;126:19-31 Older age is an independent risk factor for serious infections and mortality in IBD patients on anti-TNFs Patients >65 Patients <65 years with years with biologics biologics (n=95) (n=190) Patients >65 years without biologics (n=190) Serious infections 11% 2.6% 0.5% Neoplasms 3% 0% 2% Deaths 10% 1% 2% Cottone M et al. Clin Gastroenterol Hepatol 2011 Efficacy of Anti-TNF in the elderly ALL PATIENTS EXCLUDING PNR Reason for stopping the anti-TNF (n=63) <65 (n=118) Primary NR (%) 44 19 Loss of response (%) 6 37 Side effects (%) 19 29 Remission-other (%) 31 14 P < 0.001 Lobaton T et al. Leuven group. Safety of anti-TNF in the elderly1 (n=63) < 65 anti-TNF (n=118) -CS (n=70) Infection (%) 21 12 20 Infection with hospitalization (%) 13 (p= 0.026) 3 16 Any SAE (%) 56 (p= 0.028) 39 10 Need for surgery (%) 19 10 14 Death (%) 6 1 Malignancy (%) 6 2 19 Acute reaction with antiTNF (%) 5 11 - Delayed hypersensitivity with antiTNF (%) 4 11 - Adverse events -TNF Lobaton T et al. Leuven group Take Home Point #9 Anti-TNFs have a lower efficacy and a higher risk in the elderly Take Home Point #10 Step-Up Therapy is the better approach than Top-Down Therapy for elderly IBD patients. Medical Therapy Proposed step-up medical therapy in elderly-onset IBD Biologic therapy use increases the risk of severe infections in elderly patients with IBD. A step-up approach of adding therapies may be preferred over a top-down approach in elderly-onset IBD. In patients requiring anti-TNF therapy for induction, monotherapy for maintenance of remission should be the preferred choice given the greater risk of lymphoma and infection in this age group with combination therapy. If a patient has failed immunomodulators, monotherapy with anti-TNF therapy would appear appropriate. Biologic therapy Methotrexate* > Thiopurines Antibiotics / Budesonide > Corticosteroids 5-Aminosalicylates * In patients with CD Additional Thoughts/Concerns Colon Cancer Screening/Surveillance Depression Compliance Intestinal Bacteria Vaccination Gisbert JP. Aliment Pharmacol Ther 2014; 1-19 Long MD. J Crohns Colitis 2013; 1-7 Enck P. Z Gastroenterol. 2009; 47: 653-8 Vaccination concerns Stop IS / TNF inhibitor Diagnosis of IBD 3 weeks Live and live attenuated vaccines 3 months* NO VZV/MMR (children) Others: case by case Inactivated vaccines DTP / influenza / pneumococcal polysaccharide / recombinant hepatitis B / HPV * This delay may be reduced to 1 month in case of use of corticosteroids alone IS = immunosuppressant; DTP = diphtheria/tetanus toxoids and pertussis vaccine; HPV = human papillomavirus vaccine; MMR = measles, mumps and rubella vaccine; VZV = varicella-zoster virus vaccine. Conclusions: Take Home Points The onset of IBD at an advanced age occurs more frequently than previously thought. The burden on the healthcare system from older IBD patients is rising. IBD at an advanced age has a less aggressive natural history and a different distribution at presentation. Conclusions: Take Home Points Comorbidities and polypharmacy affect outcomes, morbidity, and mortality. Look for, prophylax for, and treat Cdifficile and venous thromboembolism. IBD patients over age 50 should have bone density testing. Less tendency for surg, but worse outcomes; comorbid conditions&nutritional status are RFs for poor surgical outcomes. Conclusions: Take Home Points 6MP/AZA pose significant risk of lymphoproliferative disorders in the elderly, so methotrexate may be a better option. Anti-TNFs have a lower efficacy and a higher risk in the elderly. Step-Up Therapy is the better approach than Top-Down Therapy for the elderly.