416 lab 4 adj
advertisement

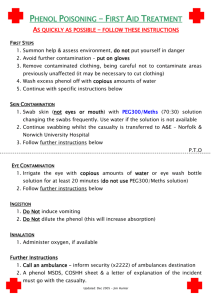
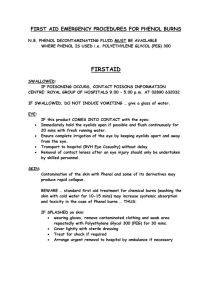
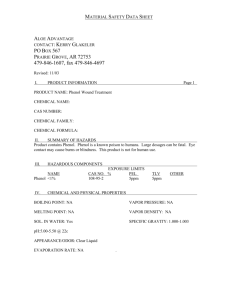
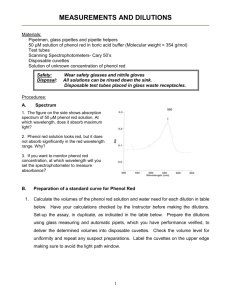
Sterilization: complete removal, destruction, inactivation of all forms of microbial life viruses, Fungi, bacteria, Spores. • Disinfection: elimination of most pathogenic organisms excluding sporicidal activity. There are 3 levels; • HLD, all vegetating bacteria, fungi, all viruses • ILD, all vegetating bacteria, majority of fungi, majority of viruses • LLD, vegetating bacteria, some fungi, some viruses •Antiseptics: chemical disinfectants applied to skin, mm but not systemic. •Cleaning: removal of dust, dirt, organics, FM. •Decontamination: general term applied to any procedure by which microorganisms are reduced to a level where items are safe to handle Patient’s care items are divided into 3 categories: Critical items Semi-critical items Non-critical items Depending on the risk of infection due to their utilization Critical Semi critical Items enter -sterile tissues-cavitiesvascular system Items come in contact with intact mm & non intact skin e.g. needles, implants, catheters, surgical instruments e.g. endoscopes, endotracheal tube, thermometer Sterilization: EO, autoclave, plasma. High level disinfectant, glutaraldehyde, chlorine active, hydrogen peroxide Noncritical Items come in contact with intact skin e.g. sphygmomanometers, bed linens, floors Intermediate and low level disinfectants, alcohols, phenols Decreasing order of resistance of microorganisms to disinfection and sterilization Resistant • • • • • • • Susceptible • • Prions Bacterial spores Mycobacteria Small non-enveloped viruses Gram-negative bacteria Fungi Large non-enveloped viruses Gram-positive bacteria Lipid enveloped viruses Decontamination Steps I. Heat 1- Moist heat or steam sterilization 2- Dry heat sterilization II. Low temperature (cold): 1. chemical a. ethylene oxide b. liquid steriliants: GLD, PAA, H2O2 2- plasma sterilizer III. Other sterilizers: 1- ionizing radiation 2- filtration 3- microwaves; in pharmaceutical industries • Heat is the most practical, efficient, and inexpensive method of sterilization and disinfection of objects that can withstand high temperatures. • There are two forms: – Moist heat is much more efficient than dry heat because: • it kills microorganisms by coagulating and denaturing their enzymes and structural proteins • it is quicker in heating up the article to be sterilized. – Dry heat is believed to kill microorganisms by causing destructive oxidation of essential cell constituents. Autoclave principle>> saturated water steam under high pressure. •heating water under controlled conditions in a closed vessel in order that boiling point of water rises above 100°C. •Saturated steam carries the same temperature of boiling water. It is essential to make steam saturated and free of any residual air because air acts as an insulator, reduces temperature and hinders penetration. Sterilization temperature and exposure time : at 121°C for 20-30 minutes at double atmospheric pressure (2 bar) Or at 134°C for 3-6 minutes (at 3 bar). • Steam sterilization is the most common and preferred method for sterilizing those items that can withstand high temperature and moisture, • e.g. culture media, surgical instruments and dressings. Autoclave: Advantages: 1- Non-toxic 2- liberation of latent heat due to condensation of steam 3- Inexpensive 4- Rapidly microbicidal 5- Least affected by organic/inorganic soils 6- Rapid cycle time 7- Penetrates medical packing, device lumens Disadvantages: 1- Deleterious for heat labile instruments 2- not suitable for powders and oils Sterilization monitored routinely by combination of mechanical, chemical, and biological parameters • Physical - cycle time, temperature, pressure • Chemical - heat or chemical sensitive inks that change color when germicidal-related parameters present • Biological - Bacillus spores that directly measure sterilization (bacillus stearothermophilus) Chemical Indicators I. Incineration: II. Red heat: • • For dead animal bodies Infectious hospital waste for wires, loops, tips of forceps they are flamed till reach redness III. Hot air oven: Dry hot air used either 170c for 60 min or 160c for 120 min Micro-incinerator • Hot air oven - They are electrical devices used in sterilization. -There is a digitally controlled thermostat controlling the temperature. - Their double walled insulation keeps the heat in . - There is also an air filled space in between to aid insulation. - An air circulating fan helps in uniform distribution of the heat. Advantage of dry heat 1.Hot air penetrates certain substances that cannot be steam sterilized (oil, powder). 2. Dry heat can be used in laboratories to sterilize glassware 3. Dry heat is a protective method of sterilizing, no erosion or corrosion. 4. Instruments that cannot be disassembled may be sterilized in hot air. 5. Low cost Disadvantages of dry heat 1. A long exposure period is required( because hot air penetrates slowly possibly unevenly. ) 2. Time and temperature vary for different substances. 3. Over exposure may ruin some substances. 4. It is destructive to fabrics and rubber goods Monitored by B.subtilis spores. • Ethylene oxide gas is commonly used to sterilize objects sensitive to temperatures greater than 60 °C such as plastics, optics and electrics. • Ethylene oxide penetrates well, moving through paper, cloth, and some plastic films and is highly effective. • Ethylene oxide sterilizers are used to process sensitive instruments which cannot be adequately sterilized by other methods • Advantages – Very effective at killing microorganisms – Penetrates medical packaging and many plastics – Compatible with most medical materials not withstanding heat – Cycle easy to control and monitor • Disadvantages 1. highly flammable 2. requires a longer time to sterilize than any heat treatment 3. The process also requires a period of post-sterilization aeration to remove toxic residues. Monitored by B. subtilis spores 1- Gamma rays (Co-60). 2-High energy electrons (electron accelerator). This process does not result in rise in temp; but the time required for sterilization is long (48hrs). High penetration power so used in prepacked items, as gloves, syringes, plastic IV lines,… Monitored by B.pumilus spores Filtration: Fluids • Sterilization of fluids which would not withstand heat such as antibiotic solutions, blood products, hormones, vitamins….etc. • Fluids can be rendered free of bacteria by passage through filters with a pore size of less than 0.45 µm. – However, most viruses and certain bacteria as mycoplasma can pass through filters with a pore size as small as 0.22 µm. • Early filters made from glass and asbestos – largely replaced by membrane filters made of cellulose esters or other polymers. • Membrane filters are preferred because: – they filter more rapidly. – they don't affect the filtrate in any way. – they adsorb very little of the substance being filtered. • The endopigment producing Serratia marcescens can be used to test the efficiency of bacterial filters. • Filters can be used to remove microorganisms from air supplied to critical areas such as operating rooms, drug factories and laminar flow ventilation system. • A properly installed high efficiency particulate air (HEPA) filter can achieve 99.997% arrest to particles ≥ 0.5 µm, and can produce sterile air. • Spores of the fungus Aspergillus can be used to test the efficiency of HEPA filters. Filtration: Air 1- Chemical disinfection 2- Boiling water 3- Pasteurization 4- Ultraviolet irradiation Chemical disinfection 1- Alcohol 70% (ethyl and isopropyl). 2- Biguanides (chlorhexidine). 3- Chlorine- active compounds (hypochlorite, house hold bleach). 4- Iodine based compounds 5- Phenol containing preparations. 6- Quternary ammonium compounds . 7- Hydrogen peroxide 8- Peracetic acid 9- Glutaraldehyde(cidex) and Formaldehyde 1- Alcohol 70% (ethyl and isopropyl): Exposure time: 5 min at least Uses: 1- disinfection of a. external surfaces b. non invasive instruments 2- skin antiseptic, alone or added to iodine or chlorhexidine 2- Biguanides (chlorhexidine): 1- antiseptic for skin and mm, mouth wash (hexitol) 2- combined with . Alcohol as hand rub . Detergent as hand wash 3- Chlorine- active compounds (hypochlorite, house hold bleach): 1- decontamination of blood splashes and lab. Working surfaces (100-1000ppm) 2- linen bleaching 3- disinfection of water 4- Iodine based compounds (most effective antiseptics): 1. 2. 3. 4. 5. include - tincture iodine (iodine in alcohol), staining and irritant - iodophores (iodine with neutral carrier): slow release of free iodine. more penetration. no staining . not irritant, betadine (30-50ppm)used as skin antiseptic in surgical scrubbing and before surgery. Both halogens exert their bactericidal action by irreversible oxidation of the essential enzymes by the free radicals 5- Phenol containing preparations (phenol\lysol) ILD: Used for floors, walls and furniture Hexaphenol (detol) was used as antiseptic, was proven to cause neurological damage 6- Quternary ammonium compounds LLD: detergent either .anionic as soap or . Cationic as cetylethyl-ammonium chloride. Used for routine cleaning of walls, floors or furniture. 7- Hydrogen peroxide: (oxidizing agent) HLD& sterilants 1- antiseptic for open wounds( kill anaerobes) 2-disinfection of soft contact lenses, some endoscopes 8- Peracetic acid: (oxidizing agent) HLD& sterilants HLD, strilizant of instruments as endoscopes 9- Glutaraldehyde(cidex) and Formaldehyde HLD& sterilants: GLD: HLD, sterilizant of instruments as endoscopes, respiratory and anaesthesia equipments FLD: gas not used now, found to be carcinogenic, only used in sterilization of HEPA filters. Evaluation methods of disinfectants: To evaluate an antiseptic or disinfectant, the phenol coefficient test is used. Phenol coefficient test (Rideal Walker method) Principle: It is a measure of the bactericidal activity of a chemical compound in relation to phenol. Phenol Coefficient Test is done by measuring the concentration at which a chemical is equal in effectiveness to phenol. a. If a chemical is equal in effectiveness to phenol at the same concentration, its phenol coefficient is 1. b. If the concentration of the chemical to be tested must be twice that of phenol, its phenol coefficient is 1/2. c. If the solution is less concentrated than the phenol standard, its phenol coefficient is greater than 1. Phenol Coefficient = dilution of chemical dilution of phenol • Phenol Coefficient Test – A series of dilutions of phenol and the experimental disinfectant are inoculated with Salmonella typhi or Staphylococcus aureus . – Samples are removed at 2.5 min intervals and inoculated into fresh broth. – The cultures are incubated at 37°C for 2 days – The highest dilution that kills the bacteria after a 7.5min exposure, but not after 5 min, is used to calculate the phenol coefficient – The reciprocal of the maximum effective dilution for the test disinfectant is divided by the reciprocal of the maximum effective dilution for phenol to get the phenol coefficient – For example: Suppose that, on the test with Salmonella typhi The maximum effective dilution for phenol is 1/90 The maximum effective dilution for “Disinfectant X” is 1/450 The phenol coefficient for “Disinfectant X” with S. typhi = 450/90 = 5 EVALUATION OF THE EFFICACY OF AN ANTISEPTIC BY RIDEAL WALKER TEST • Materials: – Staph. aureus suspension – 5ml of phenol (1:95) – 5 ml of different dilutions of the antiseptic under test.(1:50,1:100,1:150………………. – 4 sterile broth tubes for each dilution. – Loop – 1sterile pipette 1 ml Methods: • Add 0.2 ml of S.aureus suspension to each of the dilutions of the phenol and antiseptic leaving 30 seconds intervals between each tube. • At 2.5 minutes intervals inoculate one loopful of each of the previous dilution tubes into a sterile broth tubes. • Shake all the tubes and incubate at 37oC for 2 days. • Record the results as – if there is no growth and + if growth occurs. • Calculate the phenol coefficient of the given antiseptic. Results: Time of Sampling (min) phenol 1:95 1:50 Antiseptic 1:100 1:150 1:200 2.5 + _ + + + 5 + _ _ + + 7.5 _ _ _ _ + 10 _ _ _ _ _ Boiling at 100c for 20 min = HLD ……Only in emergencies Three methods of pasteurization • Low temperature (62°C) for long time (30 minutes), rapid cooling. • High-temperature-short-time (HTST) method (72°C for 15 seconds) rapid cooling . • Ultra-high-temperature (UHT) method (140-150°C for few seconds) rapid cooling. UV is a low energy, non ionizing irradiation Its present in sun, artificially produced by mercury lamps Over exposure may cause eye damage and skin irritation Have extremely weak penetration power Used only for: Air and surface disinfection in Operating rooms Safety cabinet Importance of bacterial count Various methods are used in microbiology to measure the numbers of microorganisms per unit volume of a given sample This measurement is needed for:1. Standardization of inocula in microbiological assay • [e.g. evaluation of antimicrobial agents, assay of vitamins] 1. Industrial fermentation. 2. Evaluation of sterilization technique. How to determine bacterial growth? 1. Direct microscopic count: Used to determine the number of both dead and living bacterial cells (haemocytometer). 2.Turbidimetricdetermination (viable & dead) • Increased turbidity in a culture is another index of bacterial growth and cell numbers. The increase in the number of cells during growth increases the turbidity. Turbidimetric determination is done using a spectrophotometer. SPECTROPHOTOMETER Measure growth rates with a spectrophotometer – Measure living and dead cells • Gives immediate assessment of the number of cells in a population. • Direct relationship between cell number and absorbance, Otherwise known as Optical Density More bacteria= higher absorbance. less light reaches sensor Cells scatter light, not absorb light How to USE THE SPECTROPHOTOMETER Bacterial suspensions are measured at wave length equals 600 nm . A clear solution will allow almost all of the light through (BLANK). Light entering a cloudy solution will be absorbed. The amount of absorbance obtained measures what fraction of light passes through a given solution and compared to that absorbed by a clear solutio The amount of cells in the solution is directly proportional to the absorbance reading (linear relationship) A graph of absorbance vs. concentration will give a straight line. Dry weight and nitrogen content determinations: . In this method, the bacterial cells are collected by centrifugation, then dried in an oven overnight at 85℃. • The dry weight of bacterial mass will be proportional to their number. • Also the nitrogen content of the dry sample can be determined by micro kjeldahl method MICRO KJELDAHL METHOD • Bacterial cells are heated with conc H2SO4 • Ammonia is liberated. • Ammonia is distilled & captured in boric acid solution. • Titrate with 0.01N HCL • Using methyl red- bromo cresol green as indicator. 4. Measurement of microbial activity • Many microbial activity measured quantitatively and used as a measure of microbial growth. e.g; the growth of acid forming bacteria may be measured by simple titration of the culture using standard alkali. 5. Viable count of bacteria: • in this method only viable cells which are capable of reproduction are counted. • Principle: Based on the fact that if the viable cells are allowed to grow apart from each other on a solid medium, each cell develops into one visible colony. The number of colonies obtained is equal to the number of viable cells. Viable count of bacteria • There are different procedures used to determine viable bacterial count:a. Pour plate method. b. Spread plate method. c. Surface viable count A. pour plate method • In this method different dilutions are done from • • • • the bacterial suspension. 1 ml of each dilution is then poured on a sterile empty Petri dish. 15 ml of melted nutrient agar whose temperature is about 45oC is poured in each plate with swirling. The plates are left to dry and then incubated at 37oC for 48 hours. The plates containing number of colonies between 30-300 only are counted to eliminate error,Calculate CFU/ml by multiplying number of colonies by the dilution factor. B. Spread plate technique In this method different dilutions are done from the bacterial suspension. Sterile nutrient agar plates are prepared for each dilution. 1 ml of each dilution is then poured on the agar plates. Using a glass or metal spreader- previously sterilized by dipping it in alcohol and flaming-the bacterial suspension is then uniformly spread on the plate The plates are left to dry and then incubated at 37oC for 48 hours. The plates containing number of colonies between 30-300 only are counted to eliminate error. Calculate CFU/ml by multiplying number of colonies by the dilution factor. C. Surface viable technique Materials: Culture of S. aureus. Nutrient agar plate. Ringer solution. 3 Test tubes. Sterile 3ml pipettes. Sterile 10ml pipette. Sterile Pasteur pipette 9 ml ringer solution 1ml 1ml 1ml bact. Susp. R.S S 1 1:10 2 1:100 3 1:1000 dilution 1 drop in each sector Don’t Invert and incubate After incubation Each sector from 10-30 colonies Count the colonies in each sector and record the results Result • Count the number of colonies on each sector in the plate which are in the range of 10-30. • Over 30 reported as TNTC. • Under 10 reported as TFTC. Result Sector number No. of colonies /sector 1 a 2 b 3 c 4 d Result No of cell / 1ml of original culture (cfu/ml)=( ( a+b+c+d )/4 )X20X dilution factor