Draft Outline for MCGM-NGO Council Public Health Policy Project
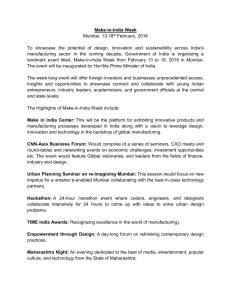
advertisement

Draft Outline for MCGM-NGO Council Public Health Policy Project
Background
This report started as a discussion between the members of the NGO Council and the MCGM
after it was found that there was no existing public health policy document on accessing health
care in Mumbai. The NGO Council is a representing body of NGOs in Mumbai seeking to
collaborate with local authorities on issues of priority. The NGO council was formed on August
22, 2005. The Council is comprised over 70 organizations with complementary expertise
covering all causes and sectors. The primary objectives of the NGO council is to work with
Government, Donors, NGOs, and other third-parties to raise awareness and convene to address
the important issues effecting the city of Mumbai.[1] On 12/12/2005, Municipal Corporation of
Greater Mumbai (MCGM) has entered into an MOU with the NGO Council, recognizing that an
institutionalized partnership between municipal bodies and non-governmental organizations
(NGOs) / civil society organizations (CSOs) is critical for promoting Good City Governance. [2]
Probable Value of the Report
In this section, the author has outlined how the report can be of value to the different existing
bodies in the city of Mumbai. The report was not only created for the MCGM, but also for all the
other proponents of health care in Mumbai. The following section details to value to each
constituency:
MCGM: This report should be seen as an objective analysis of the existing programming at the
MCGM. In addition to giving suggestions, the report also highlights the various successes of the
MCGM’s health programming. It will be of value in several aspects:
Assist lawmakers in allocating funds to priority areas
Provide insight to those responsible for programming in terms of areas of improvement
Increase the efficiency of the MCGM public health department
Increase the reputation of the MCGM’s health services in the city
Prove as an impetus that demonstrates the MCGM’s priority of the health of the people of
Mumbai
Intimate the top-level management as to the priority areas in various departments
Apprise mid-level management of the awareness of the lack of resources
Inform lower-level staff of the value of their work and increase worker morale
NGOs: Non-Governmental Organizations working in Mumbai are working to provide health care
to the same citizens that are also the responsibility of the MCGM. This report can help bring the
two groups together to not replicate programming in high-need areas and pave the way for NGOMCGM partnerships. NGO’s can cite the information in the report as representative of the
enormous need for improved health care systems in such a large and densely populated city.
Donors: With Corporate Social Responsibility representing the progressive era of charitable
giving, it is important for donors to also be aware of the issues that are effecting the communities
that benefit from their time, money, and resources.
Citizens: In a city like Mumbai, the average citizen doesn’t think about health care unless it is a
situation of urgency or crisis. This report will make citizens aware of the issues in health care
that effect all those seeking care through the government health sector.
Medical Students, Physicians, and Health Professionals: In light of the recent strike of the
doctors in Mumbai, it is also important for policy makers to understand the perspectives of those
working on the ground. This report helps shed light on the needs of physicians and avenues for
improvement in their occupation.
Media: The MCGM health department is often the recipient of negative publicity by the medial.
The information in the report can offer some information as to the inner workings of the MCGM
health department and what the media can do to support the improvement of these systems.
Overall, the report provides an in-depth analysis of the existing programs, challenges, and
successes of the MCGM health department. Looking at the history of health policy in India, it is
evident that there has been little emphasis on improving the health of local citizens in recent
years. The report attempts to create a common area for discussion and improvement of health
systems within this city. With good basic infrastructure, there are many avenues that can be
pursued if the aforementioned parties join together to work on a healthy Mumbai.
Conclusions and Summary
In the last 20 years, there have been few initiatives proposed to improve health for the citizens of
India. When looking at the policies and initiatives proposed by the Central Government, there is
a clear emphasis on improving rural health. However, with the urban poor population rising, the
health needs of the urban poor communities are beginning to exceed those in the rural
communities. The health care crisis of the growing urban poor, especially in Mumbai, represents
a new challenge in providing health care to the masses. The health care of the urban poor is often
worse than or equal to that of the rural poor population. Over 50% of Mumbai’s population of 18
million[3] lives in slums and are part of the growing urban poor. This population is plagued with
uneven access to care, malnutrition, and poor maternal and child health. Therefore, it is critical to
look at the health of Mumbai on a continuum of urban health.
The MCGM (Municipal Corporation of Greater Mumbai) provides medical services through
three levels of care, primary, secondary and tertiary. This includes an intricate network of
teaching hospitals, secondary hospitals, maternity homes, health posts and dispensaries.
Although the infrastructure is complex, there is a multitude of improvements needed to address
the health needs of the urban poor population in Mumbai. The various challenges plaguing the
MCGM health system are growing as rapidly as the population and need to be addressed
urgently. The challenges include:
Human Resources: A large amount of vacancies in the public health department of the MCGM
lead to the apathy of the staff and patients.
Infrastructural: Lack of equipment and services at the primary and secondary level of care; lack
of referral systems to direct patients to the appropriate care level; lack of quality assurance
Systems: Lack of a centralized data system, lack of awareness of existing programs within the
MCGM
Ethical: Dilution of the value and faith in the public health system as a facility for all, not just the
indigent and underprivileged. This is a phenomenon that affects the patients as well as the staff.
Educational: Educational materials for prevention of disease and promotion of health are underutlilized or unavailable, patients do not understand the complexities of their own health
With a confident team, collaborations, and an open attitude toward change, there are many
options for the MCGM health system to become an accessible service for people seeking quality
health care at an affordable price. A no-frills health care system that emphasizes good quality at
the lowest possible cost to the consumer will not only benefit the poor, but also those taxpayers
whose money is being invested in the government run health care system. Working with existing
private providers and NGOs can be beneficial for the MCGM system in terms of decreasing the
burden and using best practices of existing programs.
Utilizing best practices from cities with similar problems to Mumbai will provide some insight
into innovations that could be implemented throughout the existing health systems. While the
problems sometimes seem to vast to deal with, it is important to remember that an
implementation strategy that works on a step-by-step approach will be the ideal method of
slowly improving the system. The MOU between the NGO Council and the MCGM is the
critical agreement that should be kept in mind in the difficult stages of planning and
implementation. This agreement is meant to bridge the gap between the government and the non
profit organizations that provide many needed services to the impoverished. Both have similar
goals, it is now time to devise a better strategy through collaboration.
Recommendations- Brief
A. Education and Information Dissemination
Ensure that a Patient Bill of Rights (enclosed) and Patient Code of Conduct are posted in every
public health care facility being operated by the MCGM
Create a map of Mumbai (in Hindi, Marathi, English, etc) with locations, timings, and services of
each healthy care facility.
Improve primary and secondary health care systems by providing training for quality assurance
at all facilities.
E
nsure that educational materials on ALL illnesses and ailments are available in multiple
languages at respective primary and secondary health care levels via posters, pamphlets, and
CHVs.
B. Reproductive and Child Health
Increase awareness about institutional deliveries by collaborating with local women’s groups.
Develop IEC materials relevant to reproductive and child health as well as other relevant
diseases by working with NGOs
Ensure all maternal, reproductive and child health services are free of cost.
Ensure that all municipal facilities are always stocked with medications for pre-natal care (iron,
folic acid etc.)
C. Medical and Administrative Personnel
Increase skills, salaries, and working hours of the Community Health Volunteers and have
CHV’s collaborate with health workers from NGOs
Discontinue the practice of allowing doctors to have private practices while employed by the
MCGM.
De-centralize the management of the primary and secondary health care services
D. Infrastructure
Hire staff to fill vacancies of doctors at the primary health care level (Health Posts and
Dispensaries) to improve the quality of care
Conduct a needs assessment of the infrastructural (both equipment, human resources) gaps in the
MCGM public health system via a survey and analysis to apply appropriate solutions.
Decrease the gaps in infrastructure (staff, equipment, and training) at the primary and secondary
levels of health care
Create a referral system so that people can access the medical services at the appropriate lowest
level.
Utilize the referral system to minimize costs, patient load, and provide better quality treatment
for serious cases.
Create management information systems to store and utilize data, statistics, and health records
appropriately.
Create systems for MCGM circulars to be accessible to all
Revamp the ambulatory system completely to provide emergency care as well as transport.
De-centralize the laboratory system. Ensure all peripheral hospitals have functional labs.
E. Systems
Create a patient feedback system to improve policies, procedures, and services for patients and
for MCGM staff.
Create a Public Health Monitoring Department that meets once in 2 months to plan for upcoming
public health issues (i.e. bird flu, leptospirosis).
F. Coordinating with other MGCM Departments
Introduce adolescent health education through the municipal school system.
Increase citizen participation through a public health citizen committee in collaboration with the
MCGM public health department.
Improve disaster management to minimize public health outbreaks
Improve water supply and sanitation at all slums, this will decrease the amount of diseases in the
area.
G. Priorities in Health
Create a department that addresses issues of respiratory health in Mumbai, this should also be a
division of the school health department
Utilizing the existing DOTS program, increase the priorities of TB management
Implement more programs focused on decreasing IMR and MMR (these should be focused on
nutrition, education, and health of the mother as well as the child)
Create a city-wide campaign regarding Malaria awareness to be promoted during and before
Malaria months
Ensure that all vitamins and supplements are available to NGOs distributing them to children
through various programs
Patient Bill of Rights
Each place posting the Patient Bill of Rights needs to affirm the following statement.
"We, the staff and the administration of {health facility} declare the following Bills of Rights
for the patients of this medical facility. As per the Municipal Corporation of Greater Mumbai, we
declare that staff and administration of {the health facility} have read and understood the
following rights of a patient and hereby agree to all the terms listed below. If you have any
questions or complaints, please contact {Name of accountable person at health facility} or {name
of accountable person at BMC}."
To be treated with dignity irrespective of their caste, class, sex, religion, and disease
To have a list of exact services available and corresponding fees (for supplies, bandages, etc)
To have a visible map of the hospital (in Marathi, Hindi, English, and other languages)
To have a list of emergency services such as blood banks and ambulatory services listed in
Marathi, Hindi, English and other languages
To know and understand the procedures involved
To be given a reasonable time frame for the treatment and receive a proportional discount in fees
for all services after the upper limit of approximation is over and treatment needs to be continued
To have a comprehensive (various tests, blood work, x-rays, room tarrifs, operations, consulting
fees, etc) costs associated with seeking medical care
To receive prompt and courteous care
To be informed about the documentation needed for treatment
To have minimal documentation for emergency cases
To receive Reproductive and Child Health Services free of cost at public health facilities
To receive medications and vaccinations from the local public health post or dispensary
To get medical services which are within the capability of the medical facility
To obtain from the doctor complete information concerning the diagnosis, treatment, and
prognosis in language the patient can understand.
To receive necessary information from the doctor such as long-term effects, side effects etc.,
before giving any prior consent to a medical procedure and/or treatment
To receive the records or a certified copy that gives the details of the disease, treatment, and
follow-up necessary at the time of discharge
To refuse the suggested treatment and be informed of the medical consequences thereof
To receive medical care in well-equipped and sanitized conditions
To receive quality care from competent medical professionals
To select doctor’s of one’s choice when possible
To obtain a second opinion
To privacy during medical check-ups
To be assured that all communication and records will be kept confidential
To educational information about medical problems eg. via a library, IEC materials, etc.
To receive a bill cum receipt after the payment is made
To be enabled to pay hospital fees on a payment plan
To have access to a non-hospital staff member appointed to address complaints as soon as
possible
To have the contact information of the responsible person (both at the hospital and head office)
to register a complaint or give feedback
To have adequate waiting space
To allow relatives to have flexible visiting hours
Patient Code of Conduct
Patients are also responsible for their personal and environmental well-being. The following
code of conduct emphasizes the responsibilities of a patient while seeking medical care.
As a patient:
You should provide the doctor with accurate and complete information about his/her medical
history, past illnesses, allergies, hospitalizations, and medications
You should report the changes in your medical changes
You should ask for clarity if the doctor’s prescription and diagnosis seem unclear
You should follow the doctor’s treatment plan
You should pay your medical bills promptly
You should follow hospital rules and regulations
You should have realistic expectations of what the doctor can do for you
You should help your doctor help you, if something isn’t working, be clear and the doctor can
advise alternative care
You should participate actively in your own medical care (in terms of awareness and
preventions)
You should ask the doctor questions to clarify any doubts or misconceptions in your mind
You should treat the doctors with respect
You should not ask doctors for false bills or certificates for any reason
I. Recommendations- Expanded
A. Education and Information Dissemination
Ensure that the Patient Bill of Rights and Code of Conduct (attached) is posted in every public
health care facility being operated by the MCGM
Action Steps:
Translate the documents into Hindi, Marathi, and other regional languages
Pilot test it with a core group to ensure comprehension of the concept and what it actually would
mean
Send around a circular for ALL staff to read and understand the Bill of Rights and Code of
Conduct
Post accordingly in all health care facilities in Mumbai
Time line: 2 months
Measure of Success: Increased awareness of rights and responsibilities of patients, perhaps
greater accountability of staff
Create a map of Mumbai (in Hindi, Marathi, English, etc) with locations, timings, and services of
each healthy care facility.
Action Steps:
Hire a group of college students for 2 months to work with the Public Health Department to
come up with a map that identifies all the locations of the health facilities
This should include timings, doctor’s name, and phone number
This map should be updated twice a year by the Public Health Department, once the
infrastructure is in place
Time line: 2 months
Measure of Success: Increased awareness of government facilities, accountability for doctors,
less patient load at tertiary care services
Improve primary and secondary health care systems by providing training for quality assurance
at all facilities.
Before implementing any kind of quality measures, the entire MCGM public health department
(from the sweeper to the doctor) should understand the need for such innovations
Through role plays and consciousness raising, the staff should become aware of the challenges
before them
Hold monthly meetings with staff to imbibe aspects of quality assurance throughout the MCGM
public health department
Utilizing the health committee formulated, hold trainings for improved quality of care
Provide incentives for randomly conducted surveys of facilities that provide quality care to their
patients
Time line: 4 months
Measure of Success: Increased patient satisfaction as well as improved attitudes among staff.
Ensure that educational materials on ALL illnesses and ailments are available in multiple
languages at respective primary and secondary health care levels via posters, pamphlets, and
CHVs.
Action Steps:
Collaborate with the HELP library to create educational materials
Make sure such materials are available at ALL health facilities being run by the government
sector
Ensure that a wide array of languages are covered in these materials
Time line: 3 months
Measure of Success: Increased patient health education, awareness of preventable diseases
B. Reproductive and Child Health
Increase awareness about institutional deliveries by collaborating with local women’s groups.
Action Steps:
Engage NGOs to help involve Mahila Mandals
Create awareness among leaders in these groups about the hazards of home deliveries
Hold events and public gatherings to raise awareness among these women’s groups
Time line: Ongoing, but start up should be 3 months
Measure of Success: Increase in amount of institutional deliveries at the hospitals in the areas
where the education has taken place.
Develop IEC materials relevant to reproductive and child health as well as other relevant
diseases by working with NGOs
Action Steps:
Team up with 5 NGO Partners in order to start collecting information that already exists on these
topics
Devise a strategy to review these materials and edit/modify as needed
Print and distribute to all women
Time line: Ongoing, but start up will be 2 months
Measure of Success: Increased awareness of RCH as well as other diseases; may lead to
prevention
Ensure all maternal, reproductive and child health services are free of cost.
Action Steps:
Appeal to the budget making entities of the value of free RCH services
Create a public service campaign regarding increasing awareness for these initiatives
Time line: Ongoing campaign, start up will be 2 months
Measure of Success: More urban poor women accessing government health care facilities for
prenatal, postnatal, and neonatal care
Ensure that all municipal facilities are always stocked with medications for pre-natal care (iron,
folic acid etc.)
Action Steps:
a. Partnerships with pharmaceutical companies can guarantee a constant stock of these very
necessary vitamins and supplements
b. An education campaign should educate women of the value of the proper utilization of these
medications before and during pregnancy
Time line: 2 months
Measure of Success: Decreased infant mortality and maternal mortality rates
C. Medical and Administrative Personnel
Increase skills, salaries, and working hours of the Community Health Volunteers and have
CHV’s collaborate with health workers from NGOs
Action Steps:
Expand job descriptions to include more responsibilities of the CHVs
Increase salary to Rs. 1000 per month
Provide ongoing trainings for them to be more engaged in the work they do
Allow them to collaborate with local NGOs CHW’s as well
Time line: 4-6 months
Measure of Success: Increased job satisfaction and output by the CHVs, greater collaboration
and raising awareness
Discontinue the practice of allowing doctors to have private practices while employed by the
MCGM.
Action Steps:
As an overall initiative, doctors should shut down their private practices at MCGM facilities
Terminate all benefits for those that had such practices
Time line: 1 month
Measure of Success: Discontinuation of private practices for MCGM doctors
De-centralize the management of the primary and secondary health care services
Action Steps:
Allow Medical Officers in each ward to take the lead in decision making
Tell them they have a certain amount of money in the budget and set realistic goals
Encourage them to reach these goals through collaboration and hard work
If they demonstrate leadership skills, there can be incentives for group management of wards
(rather than it always having to be cleared through the main office)
Time line: 4 months
Measure of Success: Increased job satisfaction and participation in the process
D. Infrastructure
Hire staff to fill vacancies of doctors at the primary health care level (Health Posts and
Dispensaries) to improve the quality of care
Action Steps:
a. Revise the personnel policies for the doctors at the primary health care to improve salaries and
make sure the following basic facilities are available at every dispensary:
Equipment to sterilize the instruments used for examination
Ample medications for all basic illnesses (diarrhea, cough, cold, flu, and fever)
Enough stock of iron, folic acid, for supplying to all women who may come to register their
pregnancies
Training in the basics of pre-natal care for community health volunteers
X-ray facilities at certain upgraded facilities
b. Collaborate with medical schools to create incentives for graduating students to commit 2
years to service at the primary or secondary level
c. Involve current doctors in recruiting of new physicians, offer incentives to those who can find
doctors who sign contracts for 2 years or more.
d. Improve the overall image of working for the MCGM improving facilities and systems
through a circular highlighting the successes of the primary health care physicians
Time line: 6 months
Measure of Success: Decreased vacancies, greater staff job satisfaction
Conduct a needs assessment of the infrastructural (both equipment, human resources) gaps in the
MCGM public health system via a survey and analysis to apply appropriate solutions.
Action Steps:
Create a simple survey to assess the equipment, amount of staff, medicines etc.
Utilizing the CHV’s (increase their work hours and pay to Rs.1000) to have a basic assessment
of equipment, vaccinations, medicines, vitamins etc (each CHV would assess a health post
different from their own to maintain objectivity
Put all the data gathered together in a simple report revealing the gaps in services and
infrastructure at the primary level
Time line: 3 months
Measure of Success: A report that identifies the gaps and direct action by the administration.
Decrease the gaps in infrastructure (staff, equipment, and training) at the primary and secondary
levels of health care
Action Steps:
Utilizing the assessment in Recommendation 13, assess the needs of each of the primary and
secondary health care facilities.
The health committee can further lobby the administration about improving the infrastructure at
each of these locations.
Infrastructure specifies: lab equipment, x-ray facilities, storage for vaccinations, provisions for
sterilizing needles, and other needs identified by the survey.
Time line: 6 months
Measure of Success: Increase in utilization at the primary and secondary levels of health care,
increased resources and infrastructure.
Create a referral system so that people can access the medical services at the appropriate lowest
level.
Action Steps:
In 5 wards, pilot test the referral system of care described in the Appendix 1, already tried once
by the Women Centered Health Project.
Using the lessons learned by SNEHA’s CINH program that brings together NGOs and public
health systems, implement 3 wards using their methods.
Assess the pilots and determine which was most complementary to the needs of the patients that
access the MCGM health care system.
Time line: 1 year
Measure of Success: No overcrowding at tertiary hospitals, greater patient understanding of
each of the tiers and what they offer.
Create management information systems to store and utilize data, statistics, and health records
appropriately.
This can be a part of the TCS created system.
Create systems for MCGM circulars to be accessible to all
Action Steps:
Using a computerized system, circulars should be sent out to all departments, and not just
specific departments
The circulars should be stored in a computer as well as hard copy
TCS is also implementing a computerized network, this should be a part of it.
Time line: 6 months
Measure of Success: Improved record-keeping and awareness of all the programs/updates going
through the MCGM system.
Revamp the ambulatory system completely to provide emergency care as well as transport.
Action Steps:
Create a public-private company willing to partner with the MCGM on issues of ambulatory care
Create minimum qualification guidelines of those operating the vehicles
Ensure the vehicles are well equipped with supplies and equipment for saving lives
Create a free call system for people to call this number 24 hours a day
Cost? Should be further discussed
Time line: 6 months
Measure of Success: Decreased deaths due to the scarcity of quality ambulatory care, perhaps
some benefits from the public-private partnership
De-centralize the laboratory system. Ensure all peripheral hospitals have functional labs.
Action Steps:
Using the infrastructure survey, it is important to assess which areas are lacking proper labs
These labs should be equipped to test for TB, AIDS, and conduct all other necessary blood work
on site
There should be no additional user fees associated with this service
Time line: 4-6 months
Measure of Success: Decreased load on the 3rd tier lab systems, better facilities for patients to
access blood work results
E. Systems
Create a patient feedback system to improve policies, procedures, and services for patients and
for MCGM staff.
Action Steps:
Through a screening process, select non-hospital staff to field the concerns of patients
Ensure the person is competent in mediation and can handle high pressure situations
The person will then bring the issue to the hospital administration team to be addressed within a
certain time frame depending on the emergency
Ensure this process is well documented with appropriate attention from administration for
complaint management
Time line: Ongoing, set up time 3 months
Measure of Success: Decreased frustration among patients and staff alike, decreased attacks on
doctors
Create a Public Health Monitoring Committee that meets once in 2 months to plan for upcoming
public health issues (i.e. bird flu, leptospirosis) and acts a citizen body to represent the concerns
of the locals.
Action Steps:
Review examples of Porto Alegre and other participatory/citizen committees
MCGM’s public health department should set up an open house day to invite all interested
parties to learn more about how the MCGM works.
The main role of the committee should be monitoring upcoming health issues and creating a
forum for discussion and preparedness (i.e. avian flu, monsoon related illnesses)
Utilize media partners to help support and promote the outputs of this collaboration
Time line: 6 months
Measure of Success: Increased citizen participation and actual change as a result of the
participation.
F. Coordinating with other MGCM Departments
Introduce adolescent health education through the municipal school system.
Action Steps:
Work with the Niramaya Health Foundation which just launched SPARSH, an adolescent health
education initiative
Pilot this initiative at some of the schools
Replicate and disseminate
Time line: 6 months
Measure of Success: Increased awareness in adolescent health, increased awareness among
children on life skills and personal health
Improve disaster management to minimize public health outbreaks
Action Steps:
Work closely with the disaster management cell and the NGO Council to start to address some of
the issues related to disaster management
Educate the city through the LACGs on the importance of preparedness
Ensure the release of it before onset of monsoon season
Time line: 4 months
Measure of Success: Increased confidence in the public health system, increased preparedness
for individuals and families
Improve water supply and sanitation at all slums to decrease the amount of diseases in the area.
To be further developed.
G. Priorities in Health
Create a department that addresses issues of respiratory health in Mumbai, this should also be a
division of the school health department
Action Steps:
Conduct an in-depth analysis of the respiratory health of Mumbai
Work with NGOs to create greater awareness
Create a cell within the school department so children can be screened for respiratory issues
Further follow up will be needed by the public health and the school department
Time line: 6 months
Measure of Success: Increased awareness of respiratory health, greater initiatives to address
them
Utilizing the existing DOTS program, increase the priorities of TB management
Action Steps:
Given the numbers of cases and deaths reported in the Mumbai health profile, it is critical that
there be more initiatives to address TB in Mumbai
Create a commission to address why there are still so many cases despite the presence of DOTs
Ensure that people suffering from TB are not building up a resistance to the medication.
If that is the case, there needs to be further concentration of a public health strategy in this area
Time line: 1 year
Measure of Success: Decreased deaths and cases reported due to TB in Mumbai
Implement more programs focused on decreasing IMR and MMR (these should be focused on
nutrition, education, and health of the mother as well as the child)
Action Steps:
Work with NGOs like SNEHA and CCDT to look at how they are improving systems to support
better Reproductive and Child Health
Utilize the benefits of the new RCH II policy that was released as an impetus for improving the
health services provided to women and children
Time line: 6 months, ongoing
Measure of Success: Decreased IMR and MMR (at least by 30-40%)
Create a city-wide campaign regarding Malaria awareness to be promoted during and before
Malaria months
Action Steps:
Given the fact that Malaria is a major problem in climates like those of Mumbai, it is critical that
the Public Health Department address this issue
Teach the public about increasing awareness about the dangers of malaria and how to prevent it
Provide citizens with information through the LACG meetings
Information should be circulated in all newspapers
NGOs and the MCGM can collaborate on this campaign
Time line: Ongoing
Measure of Success: Decreased cases and deaths by Malaria
Ensure that all vitamins and supplements are available to NGOs distributing them to children
through various programs
Action Steps:
Every month the MCGM should conduct an inventory of the stock
NGOs should submit requests for vitamins 2 months in advance
Stock should always be ensured and monitored
Time line: 3 months
Measure of Success: Increased availability of critical nutrients necessary for the development of
children
II. Executive Summary
Introduction
This report started as a discussion between the members of the NGO Council and the MCGM
after it was found that there was no existing public health policy document on accessing health
care in Mumbai. The NGO Council is a representing body of NGOs in Mumbai seeking to
collaborate with local authorities on issues of priority. The NGO council was formed on August
22, 2005. The Council is comprised over 70 organizations with complementary expertise
covering all causes and sectors. The primary objectives of the NGO council is to work with
Government, Donors, NGOs, and other third-parties to raise awareness and convene to address
the important issues effecting the city of Mumbai.[4] On 12/12/2005, Municipal Corporation of
Greater Mumbai (MCGM) has entered into an MOU with the NGO Council, recognizing that an
institutionalized partnership between municipal bodies and non-governmental organizations
(NGOs) / civil society organizations (CSOs) is critical for promoting Good City Governance. [5]
The relationship between the NGO Council and MCGM has been utilized in various Solid Waste
& Local Area Citizen Group initiatives. This report was initiated to maximize the output of the
public health system. This report is an in-depth policy analysis into Central and Municipal
policies pertaining to health via an analysis of existing programs, successes, challenges, personal
interviews, conclusions, and recommendations. The purpose of the report is to highlight what is
working and offer suggestions for where improvements can be made. This report serves as an
initial policy document necessary to begin conversations on trends in public health in Mumbai.
As India becomes a major player in the global economy, it is critical that local governments
understand the global repercussions of a weak health system in light of a strong economy. Since
Mumbai already has an existing infrastructure to catalyze these efforts, it is in this spirit that we
propose that the MCGM and NGO Council work together to address the issues in health in
Mumbai.
2. National Policies in Health Care in India National Health Policy 1982
The first national health care policy was written in 1982 by the Central Government. This policy
was created to set a primary objective of Health Care for All by 2000. The establishment of
efficient and effective primary health care systems, especially for the vulnerable: the
underprivileged, women, and children were critical elements of achieving health care for all by
2000. The GOI had set an ambitious agenda for improvement of health of the Indian citizen. An
integrated network of evenly spread specialty and super-specialty services was specified in the
draft. Since implementation of NHP-1983, the national health program was able to achieve some
successes in health care. Smallpox and Guinea Worm Disease have been eradicated from the
country; Polio is on the verge of being eradicated; Leprosy, Kala Azar, and Filariasis can be
expected to be eliminated in the foreseeable future. There has been substantial drop in the Total
Fertility Rate and Infant Mortality Rate. The life expectancy has gone from 36.7 to 64.6 in 50
years. The Infant Mortality Rate (IMR) has been cut in half since 1951.
Fifty years later, the achievements of this policy only represent a fraction of the need that exists
in India. Ironically, with a hike in user charges, proposals of privatization of government
hospitals, and increasing healthcare costs, the year 2000 represented a dynamic turn in the
intended goals of NHP-1983.[6]The burden of cost of care subsequently has shifted from being
the responsibility of the government to becoming a burden on the patient seeking care. A
retrospective analysis of the NHP-1983 alludes to the fact that the policy may have been over
ambitious considering the infrastructure that existed at that time.
National Health Policy 2002
The next National Health Policy was written in 2002, when public health investment was at an
all time low, 1.3% of the GDP in 1990 to .9% of the GDP in 1999 (GOI, 2002). The aggregate
expenditure in the Health sector is 5.2 percent of the GDP. Out of this, about 17 percent of the
aggregate expenditure is public health spending, the balance being what ends up being out-ofpocket expenses.[7] The central budgetary allocation for health over this period, as a percentage
of the total Central Budget, has been stagnant at 1.3 percent, while that in the States has declined
from 7.0 percent to 5.5 percent.
NHP 2002 expounds that country wide, less than 20% of the population which seeks OPD
services, and less than 45% of those that seek indoor treatment, avail services such as public
hospitals. This low incidence of seeking OPD (Out-Patient Dispensary) treatment is due to
unsatisfactory factors like time, workday loss, lack of faith in medication as also the outside
medical prescriptions The NHP 2002 firstly stresses the aspect of vertical programming in
current public health services provided by the government; keeping in mind that horizontal
programming (health programming that works within several sectors to accomplish similar
goals) would be more cost effective for the kind of health needs of the population on India.
Secondly, there is an imperative need to upgrade the national and statewide Disease Surveillance
Network.
Overall, the NHP-2002 document envisions the existence of an organized primary health care
structure. Since the physical features and needs of urban settings are different from rural areas,
there is a need to set a different set of measurable criteria for urban health care. In addition to
improved ambulatory and emergency care, in urban settings, the NHP-2002 emphasizes a 2
tiered healthcare system:
Primary Health Care: 1st Tier; serve a population of 1 lakh, dispensary for OPD and essential
medications
Secondary Health Care: 2nd Tier; a government hospital, where a referral is made from the
primary health centre[8]
Although the NHP-2002 document is quite thorough, it covers just basic objectives in urban
health care for the poor, which are the upcoming communities that will need the attention of the
government. The aforementioned objectives are part of the mandate for improved services in
public health services in an urban setting.
National Population Policy
The National Population Policy (NPP), drafted in 2000, also includes the critical aspect of urban
health care and its effect on population policy. The NPP 2000 affirms the commitment of
government towards voluntary and informed choice and consent of citizens while utilizing
reproductive health care services, and continuation of the target free approach in administering
family planning services.[9]
The NPP 2000 provides a policy framework for advancing goals and prioritizing strategies
during the next decade, to meet the reproductive and child health needs of the people of India,
and to achieve net replacement levels (or Total Fertility Rates) by 2010. It is based upon the need
to simultaneously address issues of child survival, maternal health, and contraception, while
increasing outreach and coverage of a comprehensive package of reproductive and child heath
services by government, industry and the voluntary non-government sector, by working in
partnership.[10] The NPP document emphasizes the importance of connecting population policy
to health care systems “it is as much a function of making reproductive health care accessible
and affordable for all, as of increasing the provision and outreach of primary and secondary
education, extending basic amenities including sanitation, safe drinking water and housing,
besides empowering women and enhancing their employment opportunities, and providing
transport and communications.[11]
Report of National Commission on Macroeconomics and Health
The Ministry of Health and Family Welfare, a division of the Government of India, submitted
this report in 2005 with the intention of taking an informative look at the health of the nation.
The terms of reference of the National Commission on Macroeconomics & Health (NCMH),
included among others, a critical appraisal of the present health system — both in the public and
the private sector — and suggesting ways and means of further strengthening it with the specific
objective of improving access to a minimum set of essential health interventions to all. It was
also intended that the Commission would look into the issue of improving the efficiency of the
delivery system and encouraging public-private partnerships in providing comprehensive health
care.[12]According to the NCMH report, the public health system in India is currently
overwhelmed by the co-existence of communicable and infectious diseases, alongside an
epidemic of non-communicable diseases (Cardiovascular diseases, cancer, diabetes, etc). Even
with existing interventions, communicable diseases are expected to decline, but there are further
risks with the emergence of new infections and non-communicable diseases that will need to be
addressed as well.
As the report is focuses on the macro-economic perspective of health, the NCMH postulates the
three major drivers of health care costs as[13]:
Human Infrastructure: Cost of staffing the health needs of the country
Drug Regime: Cost of drugs is an issue
Technology Used: Advancing health care to suit the countries needs through the use of
technology
World Health Organization Country Profile
The World Health Organization Country Profile gives an overview of the health of the country.
The World Health Organization has also analyzed the health of India. According to a report on
India by the World Health Organization (WHO) there are approximately 501,900 doctors in the
country, which equals 5.2 docs per 10,000. This is important as these doctors not only look after
a large population in urban pockets and many are even employed by many private hospitals. The
number of nurses/midwives are about 607, 376.[14] Other problems in health resources include a
shortage of funds and government medical training and there are many vacancies in lab techs,
radiologists, for diseases like malaria and tuberculosis.
Overall, the health policies of India seem to overlap in areas such as access to health, nutritional
deficiencies, lack of resources, high rates of infant and maternal mortality, lack of primary health
care services, lack of expenditure as per the state governments, and the presence of
communicable, non-communicable, and infectious diseases all at the same time. However,
through the NHP-2002, NPP-2002, the NCMH report, and the country health profile of the WHO
collaboratively offer various solutions to the aforementioned challenges in country-wide health
care. While it is clear that there have been initiatives to address health in India, it has primarily
been from a rural perspective. A closer look at the changing population intimates us that the
urban poor are the ones suffering from a new illness: access to health care.
3. Urban Poor and Health
Although the focus of many of the Central government initiatives for health have been focused
on the rural sector, it is critical to now start exploring the gaps in urban health care. Rapid and
unplanned urbanization is a marked feature of Indian demography during the last 40-50 years.
According to the 2001 census, India’s urban population currently accounts for almost 30% of the
population (approximately 285 million). This represents a 100 times increase in the past century
and nearly 40% increase during the last decade. The population and the amount of urban poor are
rapidly increasing and contributing to a significant strain on resources. The unabated growth of
the urban poor is leading to what is currently being called the “2-3-4-5 Phenomenon of
Population Growth”, which states that the Urban Population is India is currently at 285
million[15], urban poor are estimated at 70[16]-90[17] million, and the estimated annual births
among the urban poor are 2 million.[18]
The health conditions of the urban poor are similar to or worse than the rural population and far
worse than urban averages. High infant and maternal mortality, malnutrition, lack of access to
services, sub-optimal health behaviors, and inadequate public sector reproductive and child
health services. The Environmental Health Project (EHP), a project of USAID has re-analyzed
the (NFHS) National Family Health Survey (1998-1999) in 2003 and found that the health of the
urban poor has been under-estimated up to this point. The tables below have been adapted from
the EHP website. A closer comparison between the problems of the rural population versus the
urban poor gives greater insight into the upcoming challenges in urban health. As the country
shifts to the urban areas, evidence demonstrates the need for more of a focus on improving
(access to) urban health care.
Urban health care in Mumbai
In Mumbai, a city of approximately 18[19] million people, over 50% of the population lives in the
slums. With a city’s population expanding at a rate faster than infrastructure to address it, health
is likely to be impacted severely, with the underprivileged communities being the hardest hit. In
Mumbai, urban poverty manifests into informal settlements and slums which have little or no
access to sanitation, water supply, education, and health infrastructure. This dramatic increase in
the population of cities in developing countries has put enormous pressure on services like water,
sewerage, housing and transport.
The infant mortality rate (IMR) in the city is 40% and the maternal mortality rate (MMR) is
14%. The survey conducted by Reproductive and Child Health (RCH) and Centre for Operations
Research and Training (CORT) in 1999 states the sex ratio in the city as 872 females per 1000
males, net migration has contributed 19% to the population growth of the city. The crude birth
rate (CBR) in the city is 16.6 per 1000 and the general marital fertility rate (GMFR) is 108.7 per
1000. Nearly 76% of the children and 42.1% of women in the city are anemic; this percentage in
the slum and non-slum areas is 45.5 and 37.4, respectively. Nearly 50% of the children under
three years are underweight (measured in terms of weight-for-age), 40% are stunted (height-forage) and 21% are wasted (weight-for-age).[20]
According to the Maharashtra Economic Survey 2004-05, the incidence of poverty in the rural
areas of the State dropped from 58% per cent in 1973-74 to 24% per cent in 1999-2000. In the
same period, in urban areas it dropped from 43.9 per cent to 26.8 per cent. At present, the
incidence of poverty is higher in urban areas than in the rural areas.
Of the 2,38,247 children weighed in June 2005 at various anganwadis in Mumbai, 1,066 were
severely malnourished, according to government figures. In 2002, a study conducted by Neeraj
Hatekar and Sanjay Rode of the University of Mumbai's Department of Economics, projected a
floor estimate of least about 750 children dying of malnutrition in Mumbai alone each
year. [21] Further, the rates of malnutrition are higher in the urban poor than the rural average.
When looking at access to health services, the presence of infrastructure seems to make little
difference in how the poor seek health care. Table 3.1 indicates that despite the presence of
infrastructure (hospitals, health posts), only about 43% of the urban poor actually access health
services.
Mumbai is a good example of challenges of health care access for the urban poor. With some of
the finest health care institutions in the country, the urban poor often face health problems that
are similar to those effecting the rural population. The next section provides insight into the
existing health infrastructure in the city of Mumbai.
Existing Infrastructure in Mumbai
The MCGM’s existing public health system is a stark contrast in infrastructure and utilization.
Under its programs for public health care, the MCGM runs four major hospitals, 16 peripheral
hospitals, five specialized hospitals, 168 dispensaries, 176 health posts, and 28 maternity homes
with a staff of over 17,000 employees. The Corporation also runs three medical colleges. Of the
total 40,000+ hospital beds in the city, the MCGM run hospitals have about 11,900 beds. As
many as 10 million patients are treated annually in the Out-Patient Departments (OPDs) in the
MCGM hospitals.
The largest hospital, the King Edward Memorial Hospital and Medical College, alone annually
treats 1.2 million patients in its OPD. The state government has one medical college, three
general hospitals and two health units with a total of 2,871 beds. Each of the peripheral hospitals
is linked to one of the four super specialty hospitals. The health posts and the dispensaries are
linked to the peripheral hospitals in their respective Wards. These health posts were established
under the World Bank Funded project called IPP-V, and resulted in the set up of the Health Posts
which were meant to serve as the primary link between the citizen and the government.[22]
MCGM Facilities and Programs
In addition to the hospitals run by the MCGM there are secondary hospitals, maternity homes,
health posts, and dispensaries that are under their jurisdiction. There are 168 dispensaries and
176 health posts set up in Mumbai. The health posts were set up from a World Bank Initiative
called IPP-5 (India Population Project 5) which sought to set up primary health care centers in
Mumbai from 1988-1996.
The health posts provide medications for DOTS as well as medications for basic ailments
(cough, cold, fever, gastrointestinal issues) while the dispensary has a doctor that is there to
provide medical check ups. These dispensaries and health posts often don’t function at maximum
utilization rates due to large scale vacancies, disconnect of the staff and the community, and
general ignorance toward quality. While there are always exceptions, due to the overall lack of
facilities and resources given at the primary level, health posts are not universally utilized to
access primary health care.
There are 28 maternity homes run by the MCGM. Maternity homes were meant to be a referral
point from the primary health care systems. In an ideal situation, if a pregnant woman went to a
dispensary for prenatal care, a doctor there would refer her to a maternity home or peripheral
hospital for institutional delivery. However, the maternity homes are suffering under severe
neglect due to lack of equipment, on the site decision making, and quality of care. Additionally,
the controversial practice of charging fees for reproductive and child health has led to an
apathetic view of maternity homes.
Municipal hospitals are meant to be the secondary and tertiary points of care for the patient
seeking healthcare in Mumbai. These hospitals also should be used as referral points, but when
patients have a free range of choices, as is in the MCGM health system, most of the primary
infrastructure is bypassed. There are four major hospitals, 16 peripheral hospitals and five
specialized hospitals. The four major hospitals are also medical colleges which infuse them with
a greater amount of financial resources and recognition than in the peripheral hospitals. The
peripheral hospitals should be a secondary referral point from the primary health care centers;
however, it is also plagued with low resources, centralized decision making, and little attention
on quality of care. If an urgent case is brought to a secondary hospital, it tends to be transferred
to a major hospital, and due to problems in ambulatory care, patients have little chance of
survival.
The various programs include:
Leprosy Program: An initiative to address and contain Leprosy in Mumbai
Tuberculosis Program: To address, treat, educate and eradicate TB
Universal Immunization Program: An initiative to provide children and families in Mumbai with
proper immunizations
Polio Eradication Program: To immunize, treat, and eradicate Polio
National Malaria Control Program: To address and treat Malaria
Mumbai District AIDS Control Society: Educate, disseminate information, provide counseling
and treatment, blood safety, monitoring and evaluation
School Health Program: The SHP aims to provide in school health care for children attending the
schools run by the MCGM
Successes
Managing such a complex system of health infrastructure has yielded successful initiatives. The
School Health Program and Polio Eradication Programs are 2 of them. The main reasons for
success can be communicated through de-centralization of management, networking with
families, creating community understanding around a certain illness and strong leadership.
Among these few successes, there are many areas that need to be improved throughout the
MCGM public health system.
Challenges
All of the aforementioned programs are run in synergy through the jurisdiction of the Public
Health Department. Many of the reasons the public chooses not to access the care is:
The MCGM Health Budget: The budget of the MCGM Health Department (over Rs. 800 Crores)
lacks equity in terms of distribution of resources to the secondary and primary levels of care
Primary health care services are weak in resources and manpower, this leads the general public
to seek healthcare at the tertiary level of care
Secondary Hospitals and Maternity Care are also not well-equipped and suffer from centralized
decision making systems that prevent administration for taking decisions
Tertiary Hospitals are on the receiving end of the high monetary assistance and have to bear the
burden of overcrowding and higher expectations of patients due to the weakness in the secondary
and primary care systems
Inconvenient timings, locations, and a high amount of vacancies have lead to a great degree of
dissatisfaction with the MCGM run services
Lack of emphasis on quality assurance results in apathy from staff as well as patients
Lack of referral systems also lead to a misunderstanding of which services are offered where and
create too much of a free market system for patients that results in overcrowding at the tertiary
level
Reporting and data collection, as evident from the Mumbai health profiles needs to be improved
and expanded with up to date data as well as accurate descriptions of rationale
Competition from the private sector (practitioners and hospitals) also poses a considerable barrier
for underprivileged folks to access the public health system
Lack of public health disaster systems as well as adequate water sanitation and supply also
contribute to problems in access to health care
Overall, the report looks at various successes and challenges of the MCGM public health system.
Through there are many challenges, the good news is that Mumbai has an existing infrastructure
that can contribute to the improvement of how people in the city access the public health care
system. This report gives various recommendations in terms of:
Education and Information Dissemination
Reproductive and Child Health
Medical and Administrative Personnel
Infrastructure
Systems
Coordinating with other MCGM departments
Priorities in Health
The primary step that will be taken will be the initiation of a Bill of Rights for Patients as well as
a Code of Conduct to help education and inform people accessing ALL health care in Mumbai as
to what their rights are and what the expectation is of their behavior.
This report serves as an initial document to signify the NGO Council’s and the MCGM’s
commitment to the health care of the people of Mumbai. This document can be utilized by
practioners, administration teams, doctors, nurses, medical students, NGOs and more. An indepth analysis of the MCGM’s health care system can give all those involved in the field some
insight into the inner workings of Mumbai’s premier public health system in addition to citing
specific areas for improvements. A healthier community can contribute to the overall wealth of
Mumbai, making it healthy, wealthy, and wise.
Accessing Healthcare in Mumbai
Conclusions and Summary
In the last 20 years, there have been few initiatives proposed to improve health for the citizens of
India. When looking at the policies and initiatives proposed by the Central Government, there is
a clear emphasis on improving rural health. However, with the urban poor population rising, the
health needs of the urban poor communities are beginning to exceed those in the rural
communities. The health care crisis of the growing urban poor, especially in Mumbai, represents
a new challenge in providing health care to the masses. The health care of the urban poor is often
worse than or equal to that of the rural poor population. Over 50% of Mumbai’s population of 18
million[23] lives in slums and are part of the growing urban poor. This population is plagued with
uneven access to care, malnutrition, and poor maternal and child health. Therefore, it is critical to
look at the health of Mumbai on a continuum of urban health.
The MCGM (Municipal Corporation of Greater Mumbai) provides medical services through
three levels of care, primary, secondary and tertiary. This includes an intricate network of
teaching hospitals, secondary hospitals, maternity homes, health posts and dispensaries.
Although the infrastructure is complex, there is a multitude of improvements needed to address
the health needs of the urban poor population in Mumbai. The various challenges plaguing the
MCGM health system are growing as rapidly as the population and need to be addressed
urgently. The challenges include:
Human Resources: A large amount of vacancies in the public health department of the MCGM
lead to the apathy of the staff and patients.
Infrastructural: Lack of equipment and services at the primary and secondary level of care; lack
of referral systems to direct patients to the appropriate care level; lack of quality assurance
Systems: Lack of a centralized data system, lack of awareness of existing programs within the
MCGM
Ethical: Dilution of the value and faith in the public health system as a facility for all, not just the
indigent and underprivileged. This is a phenomenon that affects the patients as well as the staff.
Educational: Educational materials for prevention of disease and promotion of health are underutlilized or unavailable, patients do not understand the complexities of their own health
With a confident team, collaborations, and an open attitude toward change, there are many
options for the MCGM health system to become an accessible service for people seeking quality
health care at an affordable price. A no-frills health care system that emphasizes good quality at
the lowest possible cost to the consumer will not only benefit the poor, but also those taxpayers
whose money is being invested in the government run health care system. Working with existing
private providers and NGOs can be beneficial for the MCGM system in terms of decreasing the
burden and using best practices of existing programs.
Utilizing best practices from cities with similar problems to Mumbai will provide some insight
into innovations that could be implemented throughout the existing health systems. While the
problems sometimes seem to vast to deal with, it is important to remember that an
implementation strategy that works on a step-by-step approach will be the ideal method of
slowly improving the system. The MOU between the NGO Council and the MCGM is the
critical agreement that should be kept in mind in the difficult stages of planning and
implementation. This agreement is meant to bridge the gap between the government and the non
profit organizations that provide many needed services to the impoverished. Both have similar
goals, it is now time to devise a better strategy through collaboration.
Recommendations- Brief
A. Education and Information Dissemination
Ensure that a Patient Bill of Rights (enclosed) and Patient Code of Conduct are posted in every
public health care facility being operated by the MCGM
Create a map of Mumbai (in Hindi, Marathi, English, etc) with locations, timings, and services of
each healthy care facility.
Improve primary and secondary health care systems by providing training for quality assurance
at all facilities.
Ensure that educational materials on ALL illnesses and ailments are available in multiple
languages at respective primary and secondary health care levels via posters, pamphlets, and
CHVs.
B. Reproductive and Child Health
Increase awareness about institutional deliveries by collaborating with local women’s groups.
Develop IEC materials relevant to reproductive and child health as well as other relevant
diseases by working with NGOs
Ensure all maternal, reproductive and child health services are free of cost.
Ensure that all municipal facilities are always stocked with medications for pre-natal care (iron,
folic acid etc.)
C. Medical and Administrative Personnel
Increase skills, salaries, and working hours of the Community Health Volunteers and have
CHV’s collaborate with health workers from NGOs
Discontinue the practice of allowing doctors to have private practices while employed by the
MCGM.
De-centralize the management of the primary and secondary health care services
D. Infrastructure
Hire staff to fill vacancies of doctors at the primary health care level (Health Posts and
Dispensaries) to improve the quality of care
Conduct a needs assessment of the infrastructural (both equipment, human resources) gaps in the
MCGM public health system via a survey and analysis to apply appropriate solutions.
Decrease the gaps in infrastructure (staff, equipment, and training) at the primary and secondary
levels of health care
Create a referral system so that people can access the medical services at the appropriate lowest
level.
Utilize the referral system to minimize costs, patient load, and provide better quality treatment
for serious cases.
Create management information systems to store and utilize data, statistics, and health records
appropriately.
Create systems for MCGM circulars to be accessible to all
Revamp the ambulatory system completely to provide emergency care as well as transport.
De-centralize the laboratory system. Ensure all peripheral hospitals have functional labs.
E. Systems
Create a patient feedback system to improve policies, procedures, and services for patients and
for MCGM staff.
Create a Public Health Monitoring Department that meets once in 2 months to plan for upcoming
public health issues (i.e. bird flu, leptospirosis).
F. Coordinating with other MGCM Departments
Introduce adolescent health education through the municipal school system.
Increase citizen participation through a public health citizen committee in collaboration with the
MCGM public health department.
Improve disaster management to minimize public health outbreaks
Improve water supply and sanitation at all slums, this will decrease the amount of diseases in the
area.
G. Priorities in Health
Create a department that addresses issues of respiratory health in Mumbai, this should also be a
division of the school health department
Utilizing the existing DOTS program, increase the priorities of TB management
Implement more programs focused on decreasing IMR and MMR (these should be focused on
nutrition, education, and health of the mother as well as the child)
Create a city-wide campaign regarding Malaria awareness to be promoted during and before
Malaria months
Ensure that all vitamins and supplements are available to NGOs distributing them to children
through various programs
1. Introduction and Background
Through an initiative between the Municipal Corporation of Greater Mumbai (MCGM) and the
NGO council in Mumbai, health was identified as a major priority. This policy report was
written in order to have a better perspective on health in Mumbai. The NGO Council is a
representing body of NGOs in Mumbai seeking to collaborate with local authorities on issues of
priority. The NGO council was formed on August 22, 2005. The Council is comprised over 70
organizations with complementary expertise covering all causes and sectors. The primary
objectives of the NGO council is to work with Government, Donors, NGOs, and other thirdparties to raise awareness and convene to address the important issues effecting the city of
Mumbai.[24] On 12/12/2005, Municipal Corporation of Greater Mumbai (MCGM) has entered
into an MOU with the NGO Council, recognizing that an institutionalized partnership between
municipal bodies and non-governmental organizations (NGOs) / civil society organizations
(CSOs) is critical for promoting Good City Governance. [25]
The MCGM was formed in 1873 as Mumbai’s civic body. Through the multifarious civic and
recreational services that it provides, the MCGM has always been committed to improve the
quality of life in Mumbai.[26] It was under this spirit that the MCGM and part of their team took
the initiative to come into an agreement of partnership with the NGO Council. The MCGM has
signed a Memorandum of Understanding with the NGO Council to begin to discuss the critical
issues, one of the major ones being health.
The general responsibilities in Public Health for the MCGM are specified on the website:
Public Health and Medical Relief Services[27]
The following functions are performed by the staff in the wards under the supervision and
guidance of the Executive Health Officer, the Deputy Executive Health Officer, 4 Zonal
Assistant Health Officers and the Epidemiologist.
1. Prevention and control over communicable diseases.
2. Maintenance of vital statistics regarding births, deaths and occurrence of diseases.
3. Maternity and child welfare services.
4. Medical relief through dispensaries including mobile dispensaries.
5. Regulation of the places for the disposal of the dead.
6. Prevention of adulteration and misbranding of articles of good.
7. Licensing and controlling trades dealing in food and coming under the purview of sections 394
and 412A of the Bombay Municipal Corporation Act
8. Licensing and controlling trades (Other than food establishments)
9. Controlling places of public amusement from public health point of view, namely, cinema
houses, drama theatres, etc.
10. Registration and inspection of Nursing Homes.
11. Licensing of Nurses Establishments.
12. Expansion programme of public health and medical relief services.
13. Other miscellaneous functions
For the efficient discharge of these functions, Greater Bombay has been divided into Wards
which, have been grouped into six zones. Each zone is in charge of each of four Assistant Health
Officers. The table below is an organogram of the current hierarchy at the MGCM Public Health
Department.
Table 1.1 Organogram for the MCGM Public Health Department
For the purpose brevity and focus of this report, we have chosen to focus on very specific aspects
of health care and delivery systems. This includes primary health centers, peripheral hospitals,
maternity homes, health posts, dispensaries; communicable, non-communicable and infectious
diseases; health and hygiene, sanitation, access to water, and environmental health. This report
will exclude registrations of births and deaths, stray cattle, disposal of the dead, and such issues
such as licensing. While all issues are important, this report will only cover the aforementioned
issues as they are directly linked with access to public health care facilities.
2. National Policies in Health Care in India
This section will identify the various policies that have come in surrounding health care
initiatives in India. It is important to look at the national initiatives before we focus on Mumbai,
because these policies can provide the MCGM and the NGO Council with some insight on
national health policy standards and how good governance can help the city move forward to
adherence.
2.1 National Health Policy
The Government of India (GOI) first drafted a National Health Policy in 1983 (NHP-1983). This
policy was created to set a primary objective of Health Care for All by 2000. The establishment
of efficient and effective primary health care systems, especially for the vulnerable: the
underprivileged, women, and children were critical elements of achieving health care for all by
2000. The GOI had set an ambitious agenda for improvement of health of the Indian citizen.
An integrated network of evenly spread specialty and super-specialty services was specified in
the draft. Since implementation of NHP-1983, the national health program was able to achieve
some successes in health care. Smallpox and Guinea Worm Disease have been eradicated from
the country; Polio is on the verge of being eradicated; Leprosy, Kala Azar, and Filariasis can be
expected to be eliminated in the foreseeable future. There has been substantial drop in the Total
Fertility Rate and Infant Mortality Rate. The life expectancy has gone from 36.7 to 64.6 in 50
years. The Infant Mortality Rate (IMR) has been cut in half since 1951. The success of the
initiatives taken in the public health field are reflected in the progressive improvement of many
demographic / epidemiological / infrastructural indicators over time – (Table 2.1).[28]
Table 2.1 : Achievements Through The Years - 1951-2000[29]
Indicator
1951
1981
2000
Life Expectancy
36.7
54
64.6
Crude Birth Rate
40
33
26
Crude Death Rate
25
12
8
IMR
146
110
70
Demographic Changes
Epidemiological Shifts
Malaria (cases in million)
75
2
2
Leprosy cases per 10,000
population
38
57
4
Small Pox (no of cases)
>44,887
Eradicated
Guineaworm ( no. of cases)
>39,792
Eradicated
Polio
29709
265
Infrastructure
SC/PHC/CHC
725
57,363
1,63,181
Dispensaries &Hospitals( all)
9209
23,555
43,322
Beds (Pvt & Public)
117,198
569,495
8,70,161
Doctors(Allopathy)
61,800
2,68,700
5,03,900
Nursing Personnel
18,054
1,43,887
7,37,000
The table above highlights the progression of health infrastructure, demographics, and
epidemiology through 50 years.
These achievements only represent a fraction of the need that exists in India. Ironically, with a
hike in user charges, proposals of privatization of government hospitals, and increasing
healthcare costs, the year 2000 represented a dynamic turn in the intended goals of NHP1983.[30] The burden of cost of care subsequently has shifted from being the responsibility of the
government to becoming a burden on the patient seeking care. A retrospective analysis of the
NHP-1983 alludes to the fact that the policy may have been over ambitious considering the
infrastructure that existed at that time.
The next National Health Policy was written in 2002, when public health investment was at an
all time low, 1.3% of the GDP in 1990 to .9% of the GDP in 1999 (GOI, 2002). The aggregate
expenditure in the Health sector is 5.2 percent of the GDP. Out of this, about 17 percent of the
aggregate expenditure is public health spending, the balance being what ends up being out-ofpocket expenses.[31] The central budgetary allocation for health over this period, as a percentage
of the total Central Budget, has been stagnant at 1.3 percent, while that in the States has declined
from 7.0 percent to 5.5 percent. The current annual per capita public health expenditure in the
country is no more than Rs. 200.[32]
Table 2.2: Public Health Spending in select Countries[33]
%Population
with income
of <$1 day
%Health
Expenditure
to GDP
%Public
Expenditure on
Health to Total
Health
Expenditure
India
44%
5%
17%
China
19%
3%
24%
Sri Lanka
7%
3%
45%
UK
-
6%
97%
USA
-
14%
44%
The table above demonstrates the public health spending in select countries. India, China, and
America spend the least amount on their public health expenditure.
These statistics indicate why we are at quality level that does not deliver services at a desirable
standard. Under the constitutional structure, public health is the responsibility of the States. The
general expectation is that the State will give the principal contribution to public health care,
with the supplemental support from the Central government.
In this backdrop, the contribution of Central resources to the overall public health funding has
been limited to about 15 percent. According to NHP 2002, the fiscal resources of the State
Governments are known to be very inelastic. This is reflected in the declining percentage of State
resources allocated to the health sector out of the State Budget. In order to significantly improve
the decentralized public health system in the country, there needs to be more resource allocation
from the Central Government budget. If the State public health services, which are a major
component of the initiatives in the social sector are not supplemented with additional support, the
changes in National Health Care will be slow and lack universal access at best. The NHP-2002
has been formulated taking into consideration these ground realities in regard to the availability
of resources.[34]
NHP 2002 expounds that country wide, less than 20% of the population which seeks OPD
services, and less than 45% of those that seek indoor treatment, avail services such as public
hospitals. This low incidence of seeking OPD treatment is due to unsatisfactory factors like time,
workday loss, lack of faith in medication as also the outside medical prescriptions The NHP
2002 firstly stresses the aspect of vertical programming in current public health services
provided by the government; keeping in mind that horizontal programming (health programming
that works within several sectors to accomplish similar goals) would be more cost effective for
the kind of health needs of the population on India.
Secondly, there is an imperative need to upgrade the national and statewide Disease Surveillance
Network. Without accurate disease surveillance and monitoring, the public health system will not
be able to ascertain the accomplishments and challenges of current and past initiatives. Thirdly,
there is a greater need to have more specialists in public health and family medicine, with an
emphasis on public health nursing and access to medication.
Overall, the NHP-2002 document envisions the existence of an organized primary health care
structure. Since the physical features and needs of urban settings are different from rural areas,
there is a need to set a different set of measurable criteria for urban health care. In addition to
improved ambulatory and emergency care, in urban settings, the NHP-2002 emphasizes a 2
tiered healthcare system:
Primary Health Care: 1st Tier; serve a population of 1 lakh, dispensary for OPD and essential
medications
Secondary Health Care: 2nd Tier; a government hospital, where a referral is made from the
primary health centre[35]
Although the NHP-2002 document is quite thorough, it covers just basic objectives in urban
health care for the poor, which are the upcoming communities that will need the attention of the
government. The aforementioned objectives are part of the mandate for improved services in
public health services in an urban setting.
2.2 National Population Policy
The National Population Policy (NPP), drafted in 2000 also includes the critical aspect of urban
health care and its effect on population policy. The NPP 2000 affirms the commitment of
government towards voluntary and informed choice and consent of citizens while utilizing
reproductive health care services, and continuation of the target free approach in administering
family planning services.[36]
The NPP 2000 provides a policy framework for advancing goals and prioritizing strategies
during the next decade, to meet the reproductive and child health needs of the people of India,
and to achieve net replacement levels (or Total Fertility Rates) by 2010. It is based upon the need
to simultaneously address issues of child survival, maternal health, and contraception, while
increasing outreach and coverage of a comprehensive package of reproductive and child heath
services by government, industry and the voluntary non-government sector, by working in
partnership.[37] The NPP document emphasizes the importance of connecting population policy
to health care systems “it is as much a function of making reproductive health care accessible
and affordable for all, as of increasing the provision and outreach of primary and secondary
education, extending basic amenities including sanitation, safe drinking water and housing,
besides empowering women and enhancing their employment opportunities, and providing
transport and communications.[38]
The health related goals of the NPP are defined in a socio-demographic context and include
critical aspects of urban health care:
Address the unmet needs for basic reproductive and child health services through supplies and
infrastructure
Make school education compulsory until age 14
Reduce IMR to 30/1000
Reduce MMR to 100/100,000
Achieve universal immunization
Promote delayed marriage age
100% birth, death, and marriage registration
Attain 80% institutional deliveries, 100% by trained persons
Universal access to information and counseling regarding reproductive health
Contain AIDS
Prevent and control communicable diseases
Integrate systems in medical education and care
Establish family norms
Social sector and family welfare should be merged
Promotion of family norms
The NPP seems to critically look at population policy and health as an integrated system that
needs to be improved in synergy. Social and health problems contribute to the high population
rates which will effects health care systems adversely. These goals also have some degree of
overlap with the goals of NHP-2002.
The NPP has also has set forth some recommendations for improvements in urban health:
Finalize a comprehensive urban health strategy
Facilitate service delivery centers in urban health slums to provide comprehensive basic health,
reproductive and child health services utilizing relationships with NGOs, private sector
organizations, and corporate houses
Promote networks of retired doctors and para/non-medical personnel who may serve as providers
for clinical and non-clinical services for remuneration
Strengthen social marketing programs for non clinical family planning products and services in
urban slums
Specially targeted information, education, and community campaigns for urban slums on family
planning, immunization, ANC etc, and other reproductive health services
Aggressive integration of health education programs with medical and health programs in
environmental health, personal hygiene, nutrition education, and population education
Promote inter-sectoral coordination between departments and municipal bodies dealing with
water and sanitation, industry, housing, transport, education and nutrition
Streamline referral systems and linkages between primary and secondary levels of care in the
urban arena
Link provision of continued facilities to urban slum dwellers in compliance with the small family
norm.
These recommendations fall under the purview of the central and state governments, with both
parties taking some type of responsibility for continued access to health care for the urban poor.
2.3 Report of National Commission on Macroeconomics and Health
The Ministry of Health and Family Welfare, a division of the Government of India, submitted
this report in 2005 with the intention of taking an informative look at the health of the nation.
The terms of reference of the National Commission on Macroeconomics & Health (NCMH),
included among others, a critical appraisal of the present health system — both in the public and
the private sector — and suggesting ways and means of further strengthening it with the specific
objective of improving access to a minimum set of essential health interventions to all. It was
also intended that the Commission would look into the issue of improving the efficiency of the
delivery system and encouraging public-private partnerships in providing comprehensive health
care.[39]According to the NCMH report, the public health system in India is currently
overwhelmed by the co-existence of communicable and infectious diseases, alongside an
epidemic of non-communicable diseases (Cardiovascular diseases, cancer, diabetes, etc). Even
with existing interventions, communicable diseases are expected to decline, but there are further
risks with the emergence of new infections and non-communicable diseases that will need to be
addressed as well.
The NCMH report estimates (based on current data) that by 2015, the number of AIDS cases will
be approximately three times the current level and will be roughly equal to the cases of
tuberculosis (85 lakhs).[40] Additionally, cardiovascular diseases, diabetes, and cancers will
increase by 25% and mental health issues will affect 6.5% of the population.[41] According to the
NCMH report, prevention is the key solution for countries like India that suffer from a lack of
resources. For example:
Integrated approaches for vector control through de-centralized systems are known to reduce
water-borne diseases.
Access to clean water reduces cases of gastroenteritis and diarrhea
Immunizations reduces onset of diseases caused by lack of immunization
Vitamin supplementation prevents certain illnesses such as blindness
As the report is focuses on the macro-economic perspective of health, the NCMH postulates the
three major drivers of health care costs as[42]:
Human Infrastructure: Cost of staffing the health needs of the country
There is currently not enough engagement of Community Health Volunteers
Specialists such as pharmacists, paramedics, and lab technicians are largely unavailable
The reproductive health sector (Nurses, midwives) is underdeveloped and is not able to meet the
demand
Drug Regime: Cost of drugs is an issue
Drugs need to come under price control
The industry is largely un-regulated in India
There are no patent laws to protect the consumer and innovator
Technology Used: Advancing health care to suit the countries needs through the use of
technology
Technological advances in health should be included as part of the budget
Use of modern technology can greatly influence how illnesses are treated in India
The NCMH report discusses the challenges and successes of the state of health care in India, and
cites the following failures in the national health policy:
Weak management: Key factors include centralized decision-making, problems in project
management, low budgets, large scale absenteeism, absence of performance based monitoring,
and conflicting job roles.
Poor governance and role of state: There is very little accountability at the state level and this
leads to lack of good governance.
Lack of strategic mission: There is very little information out there that sets goals for where the
state of national health care should be.
Vertical programming: The preponderance of vertical programming is an enormous waste of
resources and time.
All these aspects of health in India contribute to the lack of access to health care for the citizens
of the country. However, the NCMH report also suggests a way forward, to improve health care
access in India. The various methods they suggest in the report include:
Promoting equity for access by reducing household expenditure on health by experimenting with
different types of funding (health insurance, public-private partnerships etc).
Restructuring the primary health care program to make it more accountable
Reduce disease burden and level of risk
Establish institutional framework for improved quality
Invest in technology and human resources
The guiding principles should be based on accountability, responsibility, accessibility,
adaptability, courtesy and participation.
2.4 World Health Organization Country Profile
The World Health Organization has also analyzed the health of India. According to a report on
India by the World Health Organization (WHO) there are approximately 501,900 doctors in the
country, which equals 5.2 docs per 10,000. This obviously does not include a large number of
doctors qualified in othe systems like Ayurveda, Homeopathy, Unani or Siddha. This is
important as these doctors not only look after a large population in urban pockets and many are
even employed by many private hospitals. The number of nurses/midwives are about 607,
376.[43] Other problems in health resources include a shortage of funds and government medical
training and there are many vacancies in lab techs, radiologists, for diseases like malaria and
tuberculosis.
Further, the external analysis helps assess the major challenges in the health programming.
While overall mortality has decreased, the report states, the living standards are amongst the
poorest in the world. This is primarily due to:
Lack of resources
Lack of a integrated multi-sectoral approach
Insufficient IEC material
Poor involvement of the NGO sector (collaboration rather)
Inadequate lab services
Manually operated health management system
Poor surveillance and poor response
Dealing with non-communicable diseases
Gender disparities:
Decline in female/male ratio:
In 1999 and 2001, the ratio went from 927 to 923.
Violence (domestic and social)
Nutritional deficiencies
56 % children under 5 said to have Iron Deficiency
Integrated Child Development Service is supposed to cover all but is slated to reach 54 million
pre-school children, pregnant and lactating women through mid-day meal programs and
emphasis on nutrition.
Stereotypes and discrimination
Increase in lifestyle diseases for certain populations[44]
A critical issue that is not discussed often is Environmental Health:
Emissions leading to greater degree of respiratory diseases
Agricultural problems
All these increase the risk of vector born diseases
Significant environmental degradation leads to destruction of natural resources
Environmental health is largely not discussed due to the prevalence of non-communicable and
infectious diseases in India. However, environmental health covers a broad range of issues such
as unsafe drinking water; unhygienic sanitation and air pollution significantly contribute to the
burden of disease, particularly in urban settings.[45]
In the same country profile, WHO asserts that in 1998, approximately 5.1% of the GDP was
spent on health care. Overall public expenditure on health was 18% and the WHO assessment of
the problem asserts a situation of getting the funds to the right places. The WHO Country Profile
supports the information on national health policy as reported in this paper. The external analysis
added value through its future vision for health care in India. The goal is to achieve optimal
health for the people, which would allow them to lead socially and economically productive lives
and be in keeping with the principles of a Health for All Strategy. The health care system
envisaged would have a public-private mix, with the latter encouraged to take a greater share of
secondary and tertiary health care services.[46]
Overall, the health policies of India seem to overlap in areas such as access to health, nutritional
deficiencies, lack of resources, high rates of infant and maternal mortality, lack of primary health
care services, lack of expenditure as per the state governments, and the presence of
communicable, non-communicable, and infectious diseases all at the same time. However,
through the NHP-2002, NPP-2002, the NCMH report, and the country health profile of the WHO
collaboratively offer various solutions to the aforementioned challenges in country-wide health
care. While it is clear that there have been initiatives to address health in India, it has primarily
been from a rural perspective. A closer look at the changing population intimates us that the
urban poor are the ones suffering from a new illness: access to health care.
3. The Urban Poor and Health
Although the focus of many of the Central government initiatives for health have been focused
on the rural sector, it is critical to now start exploring the gaps in urban health care. The next
section discusses the future of the urban poor population and access to health care.
3.1 Urban Population growth
Rapid and unplanned urbanization is a marked feature of Indian demography during the last 4050 years. According to the 2001 census, India’s urban population currently accounts for almost
30% of the population (approximately 285 million). This represents a 100 times increase in the
past century and nearly 40% increase during the last decade. The population and the amount of
urban poor are rapidly increasing and contributing to a significant strain on resources. The
unabated growth of the urban poor is leading to what is currently being called the “2-3-4-5
Phenomenon of Population Growth”, which states that the Urban Population is India is currently
at 285 million[47], urban poor are estimated at 70[48]-90[49] million, and the estimated annual
births among the urban poor are 2 million.[50]
3.2 Health Conditions
The health conditions of the urban poor are similar to or worse than the rural population and far
worse than urban averages. High infant and maternal mortality, malnutrition, lack of access to
services, sub-optimal health behaviors, and inadequate public sector reproductive and child
health services. The Environmental Health Project (EHP), a project of USAID has re-analyzed
the (NFHS) National Family Health Survey (1998-1999) in 2003 and found that the health of the
urban poor has been under-estimated up to this point. The tables below have been adapted from
the EHP website. A closer comparison between the problems of the rural population versus the
urban poor gives greater insight into the upcoming challenges in urban health. As the country
shifts to the urban areas, the evidence below demonstrates the need for more of a focus on
improving (access to) urban health care.
Given the fact that government doctors are only 12% of the RCH services, it is clear that the
increasing problems in urban health demonstrate the need for further study and training of issues
in urban health care.
As the urban population expands and health care needs of the urban poor increase, it is critical
for the city and state governments to start focusing efforts on the health of the urban poor.
Mumbai is a perfect example of the growing need for the right to basic health care for the urban
poor population.
4. Mumbai, Maharashtra
Urbanization is one of the most significant processes found in developing countries today.
Maharashtra is one of the most urbanized states in the country with more than 42% of the
population living in cities and towns[51].The population of Mumbai has grown from less than
four million at India's Independence fifty years ago, to about 18[52] million today. The population
of Mumbai is about 18 million, with a density of 4,205 persons per square kilometer. The overall
literacy rate of the city is 77%, which is higher than the national average (82% of adult males
and 71.6% of adult females are literate). The religions represented in Mumbai include Hindus
(68% of the population), Muslims (17% of the population), and Christians and Buddhist (4%
each). The remainders are Parsis, Jains, Sikhs, Jews and atheists.[53]
Mumbai contributes to a large portion of growth and wealth in India. Mumbai contributes 10%
of all factory employment, 40% of all income tax collections, 60% of all customs duty
collections, 20% of all central excise tax collections, 40% of India's foreign trade and Rupees 40
billion (US$ 9 billion) in corporate taxes. A number of Indian financial institutions have
headquarters in downtown Mumbai, including the Bombay Stock Exchange, the Reserve Bank of
India, the National Stock Exchange of India, the Mint, and numerous conglomerates (the Tata
Group, Godrej and Reliance etc).[54] As economic prosperity sets in early 2006, the public health
of Mumbai is starting to suffer due to neglect.
4.1 Health in Mumbai, Maharashtra
In Mumbai, a city of approximately 18[55] million people, over 50% of the population lives in the
slums. With a city’s population expanding at a rate faster than infrastructure to address it, health
is likely to be impacted severely, with the underprivileged communities being the hardest hit. In
Mumbai, urban poverty manifests into informal settlements and slums which have little or no
access to sanitation, water supply, education, and health infrastructure. This dramatic increase in
the population of cities in developing countries has put enormous pressure on services like water,
sewerage, housing and transport.
The infant mortality rate (IMR) in the city is 40% and the maternal mortality rate (MMR) is
14%. The survey conducted by Reproductive and Child Health (RCH) and Centre for Operations
Research and Training (CORT) in 1999 states the sex ratio in the city as 872 females per 1000
males, net migration has contributed 19% to the population growth of the city. The crude birth
rate (CBR) in the city is 16.6 per 1000 and the general marital fertility rate (GMFR) is 108.7 per
1000. Nearly 76% of the children and 42.1% of women in the city are anemic; this percentage in
the slum and non-slum areas is 45.5 and 37.4, respectively. Nearly 50% of the children under
three years are underweight (measured in terms of weight-for-age), 40% are stunted (height-forage) and 21% are wasted (weight-for-age).[56]
According to the Maharashtra Economic Survey 2004-05, the incidence of poverty in the rural
areas of the State dropped from 58% per cent in 1973-74 to 24% per cent in 1999-2000. In the
same period, in urban areas it dropped from 43.9 per cent to 26.8 per cent. At present, the
incidence of poverty is higher in urban areas than in the rural areas.
Of the 2,38,247 children weighed in June 2005 at various anganwadis in Mumbai, 1,066 were
severely malnourished, according to government figures. In 2002, a study conducted by Neeraj
Hatekar and Sanjay Rode of the University of Mumbai's Department of Economics, projected a
floor estimate of least about 750 children dying of malnutrition in Mumbai alone each
year. [57] Further, the rates of malnutrition are higher in the urban poor than the rural average.
When looking at access to health services, the presence of infrastructure seems to make little
difference in how the poor seek health care. Table 3.1 indicates that despite the presence of
infrastructure (hospitals, health posts), only about 43% of the urban poor actually access health
services.
Mumbai is a good example of challenges of health care access for the urban poor. With some of
the finest health care institutions in the country, the urban poor often face health problems that
are similar to those effecting the rural population. The next section provides insight into the
existing health infrastructure in the city of Mumbai.
4.2 Existing Infrastructure in Mumbai
The MCGM’s existing public health system is a stark contrast in infrastructure and utilization.
Under its programs for public health care, the MCGM runs four major hospitals, 16 peripheral
hospitals, five specialized hospitals, 168 dispensaries, 176 health posts, and 28 maternity homes
with a staff of over 17,000 employees. The Corporation also runs three medical colleges. Of the
total 40,000+ hospital beds in the city, the MCGM run hospitals have about 11,900 beds. As
many as 10 million patients are treated annually in the Out-Patient Departments (OPDs) in the
MCGM hospitals.
The largest hospital, the King Edward Memorial Hospital and Medical College, alone annually
treats 1.2 million patients in its OPD. The state government has one medical college, three
general hospitals and two health units with a total of 2,871 beds. Each of the peripheral hospitals
is linked to one of the four super specialty hospitals. The health posts and the dispensaries are
linked to the peripheral hospitals in their respective Wards. These health posts were established
under the World Bank Funded project called IPP-V, and resulted in the set up of the Health Posts
which were meant to serve as the primary link between the citizen and the government.[58]
Mumbai’s health is reported through the yearly report “The Mumbai Health Profile”.
Information from profiles dating 1997-2004 has been used in the following analysis. The first
and most important aspect of Mumbai is the population and its growth. The chart below
represents the growth of the population from 1997-2004.
Figure 4.1 Growth in the Population of Mumbai[59]
According to this analysis, the population has been growing at a rate of (to be added).
The birth rates and death rates are often indicative of the population growth. The reason for over
population remains the high birth rate. Despite the fact that the birth rate has decreased, the death
rate has also decreased. The decrease in death rate can be contributed to better health (for some),
increased nutrition, the growing economy and general evolution of the population. However, the
rate at which the death rate decreased is still not equal to the birth rate. Mumbai’s birth versus
death rate is illustrated in the figure below:
The high birth rate is often correlated with a high infant mortality rate (IMR). Although the IMR
has significantly decreased in the last 50 years, it still remains a major problem for those who
cannot access health care during pregnancy and after birth of a child. Some parents feel the need
to have a safety net in case on or two children die along the way. The figure below represents the
IMR rate in Mumbai:
This table shows that the IMR rates in Mumbai have decreased over the last 7 years.
The current IMR reported by the MCGM is at 35% per 1000 births. However, this is merely the
tip of the iceberg as neo-natal deaths are often under-reported and death rates of children under 5
years old are not evaluated by the MCGM. The infant deaths below 1 year of age for the years
1997-2004 are indicated in the table below:
Table 4.1: Infant deaths of children below 1 year (1997-1999 data unavailable)
2001
2002
2003
2004
7255
7142
7403
6505
Although the numbers are decreasing, it is unclear according to the data, which intervention has
played the largest part in slowly bringing down the IMR.
The Maternal Mortality Rate (MMR) is an indicator of how many mothers are dying after
childbirth. Add information about maternal mortality. The figure below indicates the MMR in
Mumbai.
As Mumbai comes into a new age of economic prosperity, one can postulate that the health of
the city as a whole has suffered in this process. As the urban middle and upper classes have more
choices on where they seek care (mostly high specialty, private institutions) the checks and
balances that kept the MCGM public health department running efficiently are no longer
applicable.
5. Services in Detail
Healthcare in Mumbai is run under the jurisdiction of the MCGM. It functions to provide health
care to the citizens in affordable and accessible manner. Mumbai’s health care system is
probably one of the most elaborate urban health systems in the country. It is unique because it
provides care at three different levels, and functions to (hopefully) provide health care at a
minimum cost to the consumer.
5.1 Functions of the Public Health Department
The Public Health Department of the MCGM not only provides basic health care facilities but
also manages other aspects related to preventive and social or community medicine. The
Department is divided into zonal set-ups for administrative purposes. There are five such zones,
which cover 23 Wards (nine city Wards, eight western suburban Wards and six eastern suburban
Wards). The Deputy Municipal Commissioner handles each zone. Each Ward has a separate
Ward Office and the Ward Medical Health Officer (MHO) heads the Public Health Department
in that Ward. The Department carries out the following activities:
• Registration of births and deaths and maintenance of statistics
• Regulation of places for disposal of dead
• Maternity and child welfare and family welfare services, school health services
• Control of communicable diseases
• Food sanitation and prevention of adulteration of food
• Control of trades likely to pose a health hazard
• Insect and pest control
• Impounding stray cattle, immunization and licensing of dogs
• Regulation of private nursing homes
• Medical relief through hospitals
• Issuance of international health certificates for traveling abroad
• Ambulance and hearse services
• Treatment of contagious diseases
This section is an overview and analysis of the existing MCGM structure in relation to services
and access to health care.
5.2 Dispensaries and Health Posts
There are 168 dispensaries and 176 health posts set up in Mumbai. The health posts were set up
from a World Bank Initiative called IPP-5 (India Population Project 5) which sought to set up
primary health care centers in Mumbai from 1988-1996. When the World Bank pulled out, the
MCGM took the responsibility of the health posts and dispensaries. However, due to various
issues in budgeting, prioritization at the MCGM, and other reasons that are not well-documented,
the quality of services offered at these health posts and dispensaries is not quite meeting the
needs and demands of the public that accesses this system. The health posts provide medications
for DOTS as well as medications for basic ailments (cough, cold, fever, gastrointestinal issues)
while the dispensary has a doctor that is there to provide medical check ups. Unfortunately, these
dispensaries and health posts don’t function at maximum utilization rates due to large scale
vacancies, disconnect of the staff and the community, and general ignorance toward quality.
While there are always exceptions, due to the overall lack of facilities and resources given at the
primary level, health posts are not universally utilized to access primary health care.
5.3 Maternity Homes
There are 28 maternity homes run by the MCGM. Maternity homes were meant to be a referral
point from the primary health care systems. In an ideal situation, if a pregnant woman went to a
dispensary for prenatal care, a doctor there would refer her to a maternity home or peripheral
hospital for institutional delivery. However, the maternity homes are suffering under severe
neglect due to lack of equipment, on the site decision making, and quality of care. Additionally,
the controversial practice of charging fees for reproductive and child health has led to an
apathetic view of maternity homes.
5.4 Municipal Hospitals
Municipal hospitals are meant to be the secondary and tertiary points of care for the patient
seeking healthcare in Mumbai. These hospitals also should be used as referral points, but when
patients have a free range of choices, as is in the MCGM health system, most of the primary
infrastructure is bypassed. There are four major hospitals, 16 peripheral hospitals and five
specialized hospitals. The four major hospitals are also medical colleges which infuse them with
a greater amount of financial resources and recognition than in the peripheral hospitals. The
peripheral hospitals should be a secondary referral point from the primary health care centers;
however, it is also plagued with low resources, centralized decision making, and little attention
on quality of care. If an urgent case is brought to a secondary hospital, it tends to be transferred
to a major hospital, and due to problems in ambulatory care, patients have little chance of
survival. The aforementioned case is especially true in the cases on deliveries and post-partum
emergencies.
5.5 Programs
The MCGM runs a complex set of programs to address the major health issues of the Mumbai. A
government run health department is important for two major reasons:
Controlling Infectious Disease: If public health sector does not work, diseases like malaria etc
will increase
Access to Public facilities: such as ambulatory care and emergency services
The following section describes these programs in detail and provides some insight into how
they are addressed by the MCGM Public Health Department.
5.5.1 Leprosy Control Program[62]
The Leprosy Control Program was started in 1890 and is based out of the Acworth Municipal
Hospital in Mumbai. The services provided by the hospital include inpatient services, out patient
services, peripheral clinics, field work, re-constructive surgery, training, and research. The
Leprosy Control Program has achieved a significant amount of success in Mumbai over the years
and is demonstrated in the table below:
Table 5.5.1.a: Cases and Deaths: Leprosy in Mumbai[63]
1997 1998
1999
2001
2002
2003
2004
Cases
4966 423
629
310
4297
3384
1651
Deaths
4
11
10
11
7
5
5
This table shows that the cases and deaths by Leprosy have decreased significantly in Mumbai
due to the availability of medication.
Though there is no explanation for the fluctuation in numbers over the years, it can be postulated
that treatment and detection methods for leprosy have been improved and implemented by the
MCGM. The decrease in number of deaths demonstrates that treatment programs are working
and there are adequate detection methods in place to address leprosy in Mumbai. This has just
been derived from observation, as there is little conclusive information in the Mumbai Health
Profiles 1997-2004.
5.5.2 Revised National Tuberculosis (TB) Control Program
The Revised National Tuberculosis Program (RNTCP) is a national initiative that is run under
the provision of the Mumbai District Tuberculosis Control Society (MDTCS) since 1999 for the
effective control and smooth implementation of the TB control program. [64] For the
implementation of this program, the MCGM has established:
Six District Tuberculosis Officers
119 Microscopic Centers have been established at municipal dispensaries, hospitals, and TB
clinics
903 DOTS Centers (Directly Observed Treatment, Short-Course- a WHO program) have been
established to help TB patients seek care for TB.
The RNTCP conducts many health awareness activities including health awareness month,
World TB Day, community meetings, street plays and more. MCGM also collaborates with
private providers in their PPM (Public Private Mix) Project. This project was started in 2002
with 2 zones and now covers 5 zones. This program consists of a public- private partnership
between the MCGM and private providers to implement the DOTS and RNTCP. According to
the Mumbai Health Profiles, the following tables represent the cases of TB that were reported:
Table 5.5.2.a: Cases and Deaths: TB in Mumbai
1997
1998
1999
2001
2002
2003
2004
Cases
44536
37707
14424 38238 40009 24620 25888
Deaths
9339
10583
8750
9345
8998
8929
8774
This table shows that the cases and deaths by TB. The number of cases has decreased while the
number of deaths has stayed relatively constant.
It is unclear from these numbers what intervention contributed to the change in cases reported.
The drastic change in numbers is not analyzed as per the Mumbai Health Profiles. It could be
attributed to the implementation of the RNTCP initiative, but does not explain the dramatic drop
in the rates of cases reported in 1999. This calls for further investigation of the results to take a
closer look at the reasons for the changing numbers. The number of deaths attributed to TB has
been on the decline since 2001. The decline rate is (To be added later).
5.5.3 Universal Immunization Program
The Expanded Program of Immunization was launched in the year 1978 for covering all children
up to five years. In 1985, the Universal Immunization Program was launched in 1985 to cover all
the children under one year with all vaccines to achieve the following targets:
Elimination of Neonatal Tetanus by the year 1995
Eradication of polio by 2000
Reduction of 90% cases of measles by 1995
Specific activities include:
Vaccine distribution and maintenance
Collecting data and information
Performance reports
Extended coverage evaluation survey
Extra activities as needed
The chart below takes a closer look at the immunization evaluation report for the BMC for the
most recent year (2004). [65]
Vaccine
Target
Achievement Percentage
Hepatitis B
200591
61,002
30.41%
DPT III (Diptheria, Polio,
200591
196526
97.97%
Tetanus)
Polio III
200591
196114
97.96%
BCG (TB Vaccine)
200591
203397
101.39%
Measles
200591
174009
86.74%
T.T. (M) (Tetanus)
220650
173249
78.51%
D.P.T. (B)
192570
163325
84.81%
Polio (B)
192570
167531
86.99%
D.T. (5) (Diptheria)
226754
156443
68.99%
T.T. (10)
226754
184694
81.44%
T.T. (16)
226754
146324
64.52%
The table above shows the target and achievement rates, clearly, while some met and exceeded
the target, others felt quite short.
The interpretation of these numbers demonstrates that while there are some significant successes
in the MCGM Universal Immunization Program (UIP), there are still some gaps in targets that
are yet to be reached.
For example, in 2004, there were 4584 cases of Infectious Hepatitis (reported) and 92
deaths[66] in Mumbai. The table below represents the cases and deaths in Mumbai of hepatitis:
Table 5.5.3.a: Cases and Deaths: Hepatitis in Mumbai
1997
1998
1999
2001
2002
2003
2004
Cases
3455
2929
2526
3627
3810
3488
4584
Deaths
207
192
184
135
78
51
92
This table shows that the cases and deaths by Hepatitis in Mumbai. It is unknown if it is
Hepatitis A or B.
These deaths could have been prevented if the achievement rates of Hepatitis B vaccines were
better. (Will clarify if we are talking about Hep A or Hep B) Although the deaths are not so high,
the number of cases is enough to create concern and demand some type of intervention. It should
be noted that this initiative was started in March 2003 and needs some time to actualize its goals.
Clearly, the UIP has achieved some significant success in the areas of DPT (Diptheria, Polio,
Tetanus), Polio, and BCG (Tuberculosis vaccine), but still needs to meet international standards
for Hepatitis, Tetanus and others.
5.5.4 Polio Eradication Program
The Polio Program is a part of the Universal Immunization Program. The Pulse Polio Program
(PPP) has achieved a 97.6% [67]rate for vaccinations. The Pulse Polio Program is an
administration of extra Oral Polio Vaccine does to all children irrespective of their immunization
status if they are below 5 years of age. This program has achieved significant success due to an
aggressive media campaign and drive.
5.5.5 National Malaria Control Program (NMCP)
The NMCP pursues malaria control through parasite control (surveillance branch) and vector
control. The purpose of the surveillance branch is to detect malaria cases from the community
and treat them immediately. In addition to health awareness to people, the NMCP also utilizes 3
methods of surveillance[68]:
Active: House to house survey of fever patients
Passive: Blood samples of all fever cases are taken by medical personal of the MCGM
Mass Surveillance: Looking at high risk communities more broadly
Although in 2004, malaria deaths were cited at 23[69], the number of reported cases was 13,522.
This cites a need for greater action in prevention, not just in monsoon season, but in all seasons.
5.5.6 Mumbai District AIDS Control Society (MDACS)
MDACS is a program that was started in 1998 as an initiative of the MCGM. MDACS functions
as an over-seeing body to all the programs related to HIV/AIDS in the city of Mumbai. MDACS
has several activities including:
Establishing and tracking of STI/RTI services
Condom Promotion
Targeted Intervention
IEC
Youth and AIDS
Voluntary Counseling and Testing Centers (Confidential)
Prevention of Parent to Child Transmission (PPTCT)
Blood Safety
Care and Support
Training and Surveillance
Monitoring and Evaluation
Inter-sectoral Collaboration: Work Place Intervention
Through MDACS there are clearly a large amount of interventions focused to address and
control HIV/AIDS in Mumbai. The tables below give some indication of cases and reported
deaths according to the health profiles of the MCGM:
Table 5.5.6.a: Cases and Deaths of AIDS reported in Mumbai[70]
1997
1998
1999
2001
2002
2003
2004
Cases
180
384
3682
1909
2018
4445
3190
Deaths
25
66
100
178
179
889
278
This table shows that the cases and deaths by AIDS in Mumbai. The cases and deaths remain
inconsisten with little explanation.
These numbers also seem to bring about some questions as to why there is such a fluctuation of
reported deaths between 2002-2004. The WHO reports that HIV has a 0.9% prevalence in India.
The numbers from Mumbai do not corroborate with the national statistics for many reasons.
(Explain reasons here)
5.5.7 School Health Program (SHP)[71]
The SHP is a critical component of community health care. As school-going children comprise
approximately 20% of the population, it is important to promote health awareness amongst them
and their families. The objectives of the school health program include:
Promotion of positive health
Prevention of diseases
Early diagnosis, treatment, and follow-up of defects
Awakening of health consciousness in children
Provision of a healthy school environment
To achieve these objectives, the SHP provides a mix of health assessments, curative services,
rehabilitation, follow-up, healthy child and school competitions, child to child/family/community
programming, immunization, first aid and emergency care, statistics, training and other activities.
These programs reach approximately 5 lakh children per year through Std. 1, 3, 5, 7, 9.[72] The
school health program is run jointly under the health department (which is responsible for
administration) and the education department (which is responsible for logistics).[73] Each year,
the SHP plays a critical role in helping children access health care. Through
parent/teacher/community meetings, the idea of community health is re-enforced in these
children to underscore the important role everyone plays in a healthy community. Additionally,
due to the nature of follow-up in the SHP, children are able to get treatment without creating a
stressful situation in their family.
The SHP works with 7 special school clinics at Nair, Nair Dental, K.E.M., Sion, Cooper,
Rajawadi, and Bhagwati hospitals. During 2003-2004, the SHP program has admitted between
41,980 and 35,991 children into these specialty clinics, respectively. The SHP has also been
beneficial for the screening of TB and Polio and picked up such rare conditions such as
Rheumatic and Congenital Heart Disease and such illnesses. Additionally, the extensive health
education program reached out to parents, teachers, nurses, and awarded health trophies to
deserving children and schools. The School Health Program is an innovative method of
providing healthcare to children who are from impoverished populations.
5.5.8 Respiratory System Diseases
One omission from the MCGM health programming is Respiratory Systems Disease, which, as
demonstrated in the table below, are presenting an increasing health threat for residents of
Mumbai
Deaths
Reported
1997
1998
1999
2001
2002
2003
2004
Respiratory
7270
7377
7332
7223
2412
8293
8174
Disease
This table shows the deaths reported by respiratory disease from 1997-2004.
The table above illustrates a disturbing trend in the city, the rapid rise of deaths of respiratory
problems. Due to the fact that there are many infectious and communicable/non-communicable
diseases that need to be addressed, respiratory disease has been reported, but there are no
interventions reported in the Mumbai Health Profiles. It is important to note that, these are the
deaths reported, and most likely represents a fraction of the actual cases of respiratory disease.
By respiratory diseases, we are specifically referring to asthma, bronchitis, upper respiratory
infections, etc. According to a study conducted in the D-West ward by the American Journal of
Respiratory and Critical care medicine, the asthma prevalence in the Mumbai sample (3.5%
based on physician diagnosis, but 9 to 12% when including symptomatic subjects without
diagnosis).[74] With an under-reported 9 to 12 prevalence (number of cases of the disease at a
specific time) of respiratory ailments, there is a greater need for some intervention by the
MCGM. An NGO called the Oasis Foundation claims the air is so bad in Mumbai, it is
equivalent to smoking 40 cigarettes per day.[75]
In another report by the Environmental Health Department of the MCGM, it was estimated that
43.3% of the population has reported some type of a respiratory illness (this can be asthma,
bronchitis, allergic rhinitis, and chronic obstructive pulmonary disease).[76] This only
underscores the imperative need for more of a focus on respiratory care for a population that is
literally choking on its environment.
6. Successes
6.1 School Health Program
The School Health Program (SHP) is a good indicator of a successful initiative of the MCGM.
One of the main indicators of their success is the fact that they have a very long vacancy rate.
Out of 37 positions, only 5 are vacant.[77] This statistic seems acceptable compared to the high
rates of vacancies at the MCGM at this time. There are several other reasons that contribute to
the success of this program.
Decision-Making Process: Since this program falls under the jurisdiction of the Public Health
Department as well as the Education Department, it enjoys a more independent decision-making
process. This helps management take the lead in certain situations and can lead to greater
innovations within the program
Staff Continuing Education: The SHP encourages doctors to continuously be learning throughout
their employment process. Staff are encouraged to go to workshops, trainings, and courses. This
keeps staff stimulated and helps them apply new strategies to the way they treat their patients.
Immediate Follow-Up: If a child is not well and needs urgent care, the doctors are able to refer
them to clinics immediately. There is no worry about the family taking the time and care to go to
a hospital, wait, and seek care there itself.
Administration Team: The administration team seems to be up to date with everything. Weekly
reports are required in addition to meetings, updates, and follow-up. When staff feel accountable
to someone, they are more likely to perform their job well.
These are just a few of the examples of what works in the School Health Program. Overall, it
seems that de-centralized decision making, continuing education, timely follow-up and strong
leadership can make a program that sees up to 5 lakh children per year a success.
6.2 Polio Eradication
The eradication of polio was also a successful initiative of the MCGM. Through the National
Pulse Polio Campaign, Mumbai has achieved success due to the publicity and easy dosage. The
Pulse Polio Campaign asserts that any child, regardless of immunization status, should receive a
drop of polio. Community Health Volunteers (CHV’s) have been a critical aspect of this
campaign, by going door-to-door in various communities to ensure that everyone is receiving the
required dosage. The national emphasis has made a difference to bring together the entire nation
around the focus of polio eradication. The same amount of dedication, for other illnesses, could
also be utilized to eradicate other preventable diseases in Mumbai.
7. Services
It has been quite challenging to find clear outlines of the range of services and programs
provided by the MCGM. According to the Executive Health Officer (EHO), the MCGM is
constructing guidelines for provisions of health services in the following areas:
1 dispensary/health post per 50,000 people within 1.5 km.
1 facility with a maternity ward for every 150,000 people within 3 km.
1 general hospital for every 350,000 people within 5 km.
Each of these facilities corresponds to the three-tiered (primary, secondary, tertiary) healthcare
system initiated by the Government of India. The dispensary, the primary health care center, is
expected to provide treatment for fever, cold, etc. and provide outreach services, MCH
vaccinations.
The following guidelines are recommended for areas with a population of 25,000 - 50,000:
1 female doctor
1 public health nurse
3-4 nurse midwives
3-4 male M.P.W
1 Class IV (woman)
1 computer/clerk
1 voluntary women health workers – 1 for every 20,000 people
Laboratory
Sterilization, M.T.P, vaccines
Areas with populations greater than 50,000 need to be divided into two areas with populations of
under 50,000 in each. According to the same report, primary health care consisted of the
following services:
Outreach services
Population Education
Information, motivation about family planning
Health Education
Environmental sanitation
Personal Hygiene
Communicable diseases
Nutrition
M.C.H. & E.P.I
Preventive Services
Immunization
Ante-natal, Post-natal and infant care
Prophylaxis against anemia
Prophylaxis against Vitamin A deficiency
Presumptive treatment of malaria
Identification of suspected cases of leprosy and tuberculosis
Filariasis
Infant Feeding
Family Planning Services
Nirodh, conventional contraceptives and oral pills
I.U.D. insertion
Sterlization and other M.T.P. Services via referral to hospital or through mobile vans
Curative
Fist aid during accidents and emergencies
Treatment of simple ailments
Supportive Services (Referral)
High risk maternity cases
Sterilization and M.T.P.
Diagnosis and treatment of tuberculosis and leprosy
Laboratory services for diagnosis o malaria matter requiring doctors services/hospitalization
Reports and Records
Preventive services
Family planning acceptors
Vital events
Morbidity and Mortality in respect of:
Malaria
Tuberculosis
Leprosy
Diahrroeal diseases
Maintenance of family cards for population covered
Through various policies and guidelines, the MCGM realizes the urgent need for having
accessible and community based services for those that access public health care. However,
when it comes to implementation of these services, there are several challenges that impede the
utilization of municipal-run health care facilities. The following challenges are some of the major
barriers to the provision of equal distribution of health care services to the underprivileged
population of Mumbai.
7.1 MCGM Health Budget
As per the Municipal Corporation Act, the MCGM is primarily concerned with providing
preventive health care services in the city. However, the current focus seems to be leaning
toward curative care in a major way. In the following budget, it is evident that the majority of
funding goes to tertiary and secondary care.[78]
Rs. In Crore
Capital Works Plant and
Revenue
(Civil)
Machinery
Total
1. Public Health
Department
2. Medical Relief and
Education (Including
Medical Relief and
Medical Education)
3. Measures to Control
Environmental Air
Pollution
98.4
3.7
75
102.1
599.4 (537 Medical
Relief)
(62.4 Medical
Education)
62.7
45.6
707.4
3.7
11.2
69.3
4.4
Total
701.5
66.3
46.2
813.3
Clearly, the budget illustrates the above point as the budget for curative services and medical
education are nearly 7/8ths of the entire budget of the MCGM health program. The cost of
medical relief is greater in comparison with the cost of preventive services. However, for the
sake of the budget, it all falls under the category of “Medical Relief”. Additionally, because
medical education is mainly subsidized, many colleges can not collect revenue from the medical
colleges, as may be the case in other countries. This point can be validated when looking at the
top four 3rd-tiered hospitals[79]:
Hospital Name
KEM Hospital & GSM College
LTMG Hospital & College
BYL Nair & TNM College
Nair Hospital & Dental College
Total of Major Hospitals
Revenue
114.1
93.2
70.9
7.4
Rs. In Crore
Total
137.5
124.1
111.7
9.7
383
When we look further at the budgets of the special and periphery hospitals, we get a better idea
of where the priorities lie in the funding of medical institutions:
Name of Special & Peripheral Hospitals
Rs. In Crore
1
Bhajekar Hospital
1.4
2
ENT Hospital
3.0
3
Eye Hospital
1.7
4
K.B. Bhabha Hospital Bandra
15.9
5
K.B. Bhabha Hospital Kurla
8.4
6
Mun. General Hospital Ghatkopar
19.9
7
Bhagwati Hospital
14.4
8
MTA Mun General Hospital
8.9
9
Cooper Hospital
21.8
10 DN Mehta Hospital Chembur
4.1
11 VN Desai Hospital, Santa Cruz
8.9
12 MW Desai Hospital, Malad East
4.6
13 VD Savarkar Hospital, Mulund
3.4
14 MGH Barvenagar Hospital
3.6
15 SK Patil Hospital Malad East
1.7
16 Centenary Hospital, Kandivali
3.7
17 Centenary Hospital, Govandi
6.7
18 Mahatma Jyotiba Phule Hospital, Vikhroli
4.7
19 Siddhartha Nagar, Goregaon
3.4
20 BSES Mun Gen Hospital, Andheri West
2.7
Total
138.9
Many of the peripheral and secondary hospitals listed above are located in the suburbs, while the
4 major hospitals are located on the south side of Mumbai. This presents many challenges for
those that end up having to seek care at secondary and primary institutions. Infectious Disease
and Tuberculosis hospitals also do not get priority in terms of funding[80]:
Name of Hospital
Rs. In Thousands
1
Katsurba Hospital
14,37,07
2
GTB Hospital
17,65,48
3
RDTB Clinic Dadar
41,70
4
Shamaldas Gandhi Marg TB Clinic
30,74
5
Balaram Street TB Clinic
23,33
6
TB Clinic, Khar
93,04
7
Nawab Tank, TB Clinic
27,16
8
Acworth Leprosy Hospital
1,40,03
Total
35,58,55
And finally, the category of “others” which loosely covers health posts, maternity homes, and
dispensaries is at the bottom of priority list.[81]
Name
Rs. In Thousands
1
Maternity Homes, Children Welfare Services etc
59,03,21
2
Dispensaries
20,58,71
3
CHMS (PH)
3,54
4
Central Analytical Lab
29,02
Total
79,94,40
6
Public Health Department
98,39,60
7
Measures to Control Environmental Air Pollution
3,69,70
The figures above demonstrate that there are several gaps in terms of priority in funding to the
various health initiatives of the MCGM. A close look at the budget shows a major gap in the
primary, secondary and tertiary levels of care.
A budget analysis can demonstrate the trends in fund allocation and expenditure as part of the
MCGM.
Budget analysis:
Source- Budget Estimates A, 2005-2006, as prepared by Municipal Commissioner, BMC
Appendices to Budget Estimates A, Revenue Income and Expenditure (combined) 2005-2006, as
prepared by Municipal Commissioner, BMC
For- Public Health Dept., comparisons being made between budgeted estimates of 2004-2005
and 2005-2006
The increase in income for the budget estimate from 2004-2005 to 2005-2006 is given as Rs.
252.47*, whereas the increase in expenditure for the budget estimate from 2004-2005 to 20052006 is Rs. 443.53. Deficits for sure with exp. almost double the amount of income.
Budget estimates for the yr. 2005-2006 have increased w.r.t. 2004-2005, but mostly under salary
and administrative component. For example- General Superintendence- almost doubled; under
Rabies Control, Licensing of dogs; under Medical Relief and Education for King Edward
Memorial Hosp. Figures on page H-158 gives a better picture for it. The wages since 1999-00
until now have increased by almost 100% and form the major chunk of total exp. when
compared to others (other budget analysis tools can be employed to highlight the above point).
Page- H-159 shows ‘wages’ under the head of “Controllable Expenses” that have actually grown
in an uncontrollable fashion, whereas the increase in “Obligatory Expenses” mentioned above it
has not been much.
Budgeted estimates for repairs (as part of General Superintendence, under Rabies- increase by
ten times); for Medicines, Instruments and Inoculations (under Epidemics) and for Equipment
(under Medical Relief and Education for King Edward Memorial Hosp.- increase by 100%)have
also increased significantly. The thing to be noted is that while all these increments are being
made on paper, are they also being materialized or do they continue to be on paper only.
The budgeted amount to be invested for equipment (under Vector, Pest and Rodent Control) has
been reduced by almost Rs. 200, 000.
Budgeted amount under Rabies Control for ‘payment for sterilization of dogs’ has gone down by
Rs. 300,000.
The exp. under has decreased from Rs. 200,000 to a mere figure of Rs. 30,000.
The summary and concise form of detailed estimates given at page no. H-160 clearly shows that
the estimates for 2005-2006 when compared to that of 2004-2005 have been on a decline for
most of the elements of Public Health Expenditure, though it has also increased for others. To
mention a few heads where it has declined- Epidemics; Vector, Pest and Rodent Control;
Laboratory; Dispensaries (under Medical Relief and Education) etc. Examples where the
increase has taken place- Rabies Control; Life Guard Services at Juhu, Versova, Hospitals,
Maternity Homes etc.
7.2 Primary Health Care
Primary care is supposed to be the first point of access for the citizen. If primary health care
institutions are at the bottom of the priority list, then they will be treated similarly by the
consumer or patient. In Mumbai, the major issues around utilization of the public health care
system are quality of care, convenience, costs, distances, apathy among staff, and wide-spread
vacancies. As a result, people living Mumbai fail to access primary care services and proceed to
the tertiary level hospitals and private vendors for all their care, even that which is normally
addressed at the primary care level. This leads to overcrowding at the city’s third tier hospitals,
which have comprehensive services and better quality of care. According to a study conducted
by CEHAT (Centre for Enquiry into Health and Allied Themes) demonstrates that despite having
better health care services, people residing in Mumbai do not have proper access to health care as
32% of ailments remained untreated[82].
The MCGM’s described functions for dispensaries and health posts are described below:
Functions of Dispensaries:
Clinical management on OPD basis.
Immunization- polio, DPT, Measles, Tetanus, Toxid, Typhoid.
Preventive services.
In upgraded dispensaries- Laboratory services- Urine, stool, HB blood, and Malarial parasite.
(Out of 163 dispensaries- 60 are upgraded).
Health Education to the patients attending the dispensaries.
Medical examination of Municipal employees. On the whole, dispensaries, preventive, curative
services to the patients.
Functions of Health Posts:
Conducting baselines surveys of the community (of about 65,000 population) residing with in the
given geographical area.
Enlisting the eligible couples, motivating them for adoption of small family norms and providing
them with outreach services for contraception.
Immunizing children against the 6 vaccine preventable diseases viz. children tuberculosis,
diphtheria, tetanus, pertussis, poliomyelitis and measles through fixed center based and camp
approaches.
Preventing and treating case of nutritional anemia in mother and children by distributing ironfolic acid tablets & syrup.
Vitamin A syrup to all children as prophylactic doses for Vitamin A deficiency.
Oral Rehydration salt packets to children of under-five age group suffering from diarrhea
Conducting Growth Monitoring Program for children of under-five age group.
Giving health education to all slum-dwellers.
Detection and treatment of cases of Leprosy, Tuberculosis, AIDS and Malaria.
Registration of unregistered births and deaths.
Detection of new home births and the motivation of such mothers to get their babies immunized.
Establishing effective Management Information System including proper record keeping and
timely reporting.
Developing and efficient referral system.
According to leading public health experts, improving primary care is the best method to
promoting health and preventing disease in countries with high populations and low
resources.[83] During a non- research based study of a primary health center in Chembur,
Mumbai, the author found that the majority of the patients coming there were either coming for
TB medication (42%) or basic health problems 53% (fever, cough, cold). Out of 19 people
surveyed, only one person complained about the process of sending a patient to a hospital, then
health post/dispensary, then hospital again. The majority of patients (73%) were satisfied with
the quality of health care because the doctor was good.[84] This comment was most always in
relation to the doctor and the effectiveness of the medicines. An analysis of MCGM dispensaries
in two wards at Mumbai showed that an average of 85 patients are treated every day, clearly
indicating high level of utilization of dispensaries as well. The other alternative source is private
health-care sector which is relatively inaccessible to the poor but also characterized by poor
quality infrastructure and manpower and was found to be indulging in profit motivated medical
malpractices.[85]
It is clear that the public health services in Mumbai are certainly utilized; however, it is the
quality of the care that should be addressed. While the research demonstrated that the people
going to the dispensaries and health posts were satisfied by the services, there are other wards
that are plagued with vacancies at curative level positions. For example, an interview of the K
east Ward Officer (also a doctor) revealed that out of 11 positions for medical officers, there are
currently 9 vacancies.[86] Staff dissatisfaction is high among the Community Health Volunteers
(CHV’s). The CHV’s were retained after IPP-V ended to serve as the “eyes and ears” of the
MCGM- performing such duties as immunization campaigns, home visiting, family planning
education, and more duties as required. Of the CHV’s I met, all of them complained of salaries
that were too low. These CHVs make up to Rs. 900 per month, which in contrast to the onus of
their work is too low, and if the burden of community health outreach must fall upon them.
Other examples of challenges at health posts and dispensaries include a visit of Dr. Janaki Desai
to a dispensary on Antop Hill with a group of foreign visitors. “I saw the doctor use a dirty, old,
un-sanitized needle to give the patient an injection. On top of that they were asking the visitors
for money to help support the health post”.[87] Dr. Desai heads the NGO the Niramaya Health
Foundation. The organization’s main focus is to provide health education and promote the
concept of prevention. “Due to the inadequate services provided by the MCGM, our clinics have
turned into the OPD’s instead of centers for promotion of good health and prevention of disease.
We hope to work more collaboratively on these issues.”[88] Dr. Desai also mentioned that their
NGO provides iron supplements (supplied by the MCGM) to young women, and these vitamins
have been “unavailable” for the last 6 months. The challenges of utilizing the public health
system is currently presenting a challenge for those who are trying to work within the system.
In contrast, in other wards and areas of Mumbai, some citizens prefer to access care by a private
provider. In the K East Ward, public preference for outpatient care services from a BMC facility
in the CEHAT study “Un-met Need for Public Health Care Services, in Mumbai, India” was
very low (14 per cent) when compared to that for inpatient care services. Here the majority of
households reported to seek treatment from the private sector (82 percent). As mentioned earlier,
there are only 11 public dispensaries in the area, which is grossly inadequate to meet the demand
for OPD care services of over 800,000 people residing in this area. Given the larger and
physically more accessible presence of private doctors, people are likely to prefer services from
private providers rather than seeking care from public health-care services outside the locality,
where “time” and “travel” costs are higher. Here the main worry is about the identity of private
providers in this low-income locality as many of the practicing doctors in the locality are likely
to be non-qualified practitioners and /or doing cross practice.[89] The reasons cited in this study
for choosing private care cited “offers good quality service” as the main reason. However, in
terms of affordability, the same respondents said they would prefer to go to a public facilityhowever, due to lack of doctors and general unavailability; they had to seek care at a private
practitioner.[90]
Clearly, while the primary health care system does have many strengths, it is plagued with issues
of quality and access due to inconvenient timings, widespread vacancies, and lack of motivation
of staff.
7.3 Challenges at Secondary Hospitals and Maternity Homes
As is evident in the MCGM budget, the secondary (also referred to as peripheral hospitals) and
maternity homes do not receive adequate resources to support their respective institutions. The
budgeted allocation of 20 secondary hospitals is equal to the entire budget of KEM Hospital. In a
city that is expanding toward the suburbs, it is critical that the peripheral hospitals are also
prioritized in terms of development and offering of services. According to Dr. Sanjay Nagral, a
physician at Jaslok and Bhabha Hospital (Bandra), certain systems create inefficiency at
secondary hospitals. One is, despite the service, the perception is that government related health
services are always bad. Secondly, part of the problem is the bad attitude of the staff:
They think the patients are poor, so they deserve bad treatment
Senior staff reinforces this problem
Staff is genuinely inefficient
This is very true at the peripheral hospitals
Even proper seating arrangements at the OPD could ease the tension that is created by long
waiting time and staff inefficiencies[91]
Maternity homes are also not utilized properly, as surveys from the CEHAT study found that
seven to eight per cent of deliveries in Mumbai are still home deliveries. About 40% of the
population utilizes the public sector for antenatal services. According to Dr. Armida Fernandez,
founder of SNEHA, an organization working collaboratively with the MCGM to improve public
health care for Maternal and Child Health, According to Dr. Fernandez, the IMR in Mumbai is
40/1000 and the amount of neonatal deaths: 25/1000. Shockingly, the MMR in India is
equivalent to that in Mumbai (410/100,000). Clearly, there is a greater need for improvement of
care at the secondary level as well as the primary health care level.
7.4 Third Tier Hospitals
The third tier sector hospitals, KEM, Nair, Sion, and Nair Dental are known world wide for the
breadth and depth of their services. KEM is the flagship institution of medical education and
public facilities in Mumbai. These institutions provide comprehensive care, from general
medicine to cardiac surgery under their care. On the website for KEM, it states “The medical
college (school) provides training to about 2000 students in undergraduate, postgraduate and
super-specialty medical courses; in undergraduate and postgraduate physical and occupational
therapy; Masters and PhD courses in various allied specialties. A nursing school is also
maintained by these institutions. With about 390 staff physicians and 550 resident doctors, the
1800 bedded hospital treats about 1.8 million out-patients and 68,000 in-patients annually and
provides both basic care and advanced treatment facilities in all fields of medicine and
surgery.”[92] Clearly, colleges and hospitals of this caliber benefit greatly from the subsidization
of their services by the MCGM.
As is evident from the MGCM budget, the majority of the financial resources of the public health
department are allocated to these four major hospitals. In fact, their endowment makes up
approximately 7/8th (86%) of the entire public health budget. It is important to note that because
these are also medical colleges, the government in part, is also subsidizing the medical education
of students attending these colleges. Subsidizing medical education is hardly a new phenomenon;
however, the chances of the future physicians from these colleges integrating into the community
to fill the much needed gaps are minimal. The table below illustrates how minimal the medical
education fees truly are:
ALL FEES ARE FOR A TERM OF 6 MONTHS at Seth GS Medical College:[93]
First MBBS
Rs.10,100
Second and Third MBBS
Rs. 8,100
Postgraduate Medical degree courses (MS,MD,MCH,DM etc)
Rs.14,800
Postgraduate Medical diploma courses (DVD,DMRD etc)
Rs. 14,800
BSc
Rs. 1750
MSc
Rs. 5475
PhD
Rs. 6275
The table above demonstrates how minimal the fees are for medical students.
Although KEM and the other medical colleges are quite competitive at the entrance point, the
fees are not really a barrier for those seeking medical education; even the completely poor fall
into various scholarship categories. As a result, the medical education or the cost of it is not a
critical point of contention for the student. Additionally, students and residents have their own
opinions about the state of the public health system:
“The secondary hospitals have no facilities.”
“We cannot practice without proper equipment and that is the major problem with the health
posts and dispensaries”.
“I would not prefer to work at a government facility if I had the choice”.[94]
These were the words of the residents interviewed at a general OPD in a hospital/medical school
by the author. The residents spoke of the challenges they had heard from the field and implied
that they would rather go into private practice or a fellowship than stay to practice in health
clinics. When asked how much they spent on their medical education, many stated that between
scholarships, waivers, and government quotas, many of them did not have to pay anything for
their medical education. Clearly, there is a gap between curative medicine and preventive
medicine in the Indian medical system.
It is known among doctors and faculty that Preventive and Social Medicine (PSM) is like the
step-child of Indian medicine. PSM is not widely developed or even understood by the doctors
who have that qualification. Additionally, the financial value of a doctor practicing PSM is also
quite low. Therefore, the idea of PSM, which is essentially public health, is brushed aside for
more curative services. However, the value of such a practioner, especially in communities and
clinics, would be invaluable for improving the health indicators of the urban community at large.
The undervaluing of PSM has led to a great divide between preventive and curative medicine at
the practical level at 3rd tier hospitals and medical colleges.
Another aspect that has paralyzed the public hospital system, especially at the 3rd tier, is the
opportunity for professors to have a private practice in addition to their work at the hospital. This
not only takes away precious time that could be spent in the community or doing trainings, but it
sets a bad example for young residents and interns about the purpose of a publicly funded
healthcare system. Additionally, as beneficiaries of the public system, their profits should not be
utilized for personal purposes. While the original creators of the policy may have been thinking
otherwise, this policy ultimately can be detrimental to the public health system.
Also on the website, is the list of salaries for the various posts at the hospital:
Position
Salary
Resident
Rs. 6500-8000 per month
Lecturer
Rs. 15,000 per month
Associate Professor
Rs. 18,000 per month, provisional quarters
may be provided.
Professor
Rs. 25,000 per month, provisional quarters
may be provided.
With salaries lower than what most people make at the bustling call center industry, it is no
wonder that doctors are not opting for government positions in health.
Finally, the biggest challenge at the third tier is not just the low school fees, private practices,
lack of emphasis on PSM, or low salaries- it is the lack of a referral system that leads to the
overcrowding of these hospitals. These hospitals are overcrowded with people coming for simple
ailments (cough, cold, fever, backache) that can be addressed at the primary care level.
Another non-scientific survey[95] was conducted in the general OPD of KEM hospital by the
author of 20 people visiting the GOPD for health care. Sixty-five percent came from areas that
had government hospitals and facilities: Wadala, Ullhasnagar, Malad, Bhyendar, Andheri, New
Mumbai, Bhandup, Sewri, and Govandi. Patient’s less serious ailments were cold and cough,
high blood pressure, acidity, dizziness, fever due to no access to cleaning water, and respiratory
infections. These conditions could easily have been cured at the primary health care level, at a
municipal dispensary or health post. When asked why they chose to KEM over their local public
health post or dispensaries, the answers varied from not knowing about local services to
dissatisfaction with quality of care. Overall, the majority of those coming to KEM came because
the doctors were good and the treatment was effective.
“Good Doctors, and good facilities for patients”, Housewife, Wadala
“I went to a private hospital and the doctors were rude. I came here and the doctors spoke to
me nicely”, Housewife, Ullhasnagar
“Doctors and facilities are good. Those who leave here, leave well” Male, Parel
“Treatment is done well, and they take time and do good. In the village, they give an injection,
and it doesn't work well. It is good. Its not easy to handle that many people”, Driver, Rajapur
Village
“If you come 1-2 times you get better relief. The procedure has become a little complicated, it
used to be better when people were prioritized based on illness”, Saleswoman, Bhayendar. She
also added that she is unaware of the public services offered near her home.
Overall, there was a major lack of awareness of the existing public health services offered near
their home, and a major perception that the doctors treated them with more respect at KEM than
anywhere else. The average amount of money spent going there for just travel averaged at about
Rs. 56 per person. This can be half of one day’s wages for daily laborers, and the waiting time
can surely cost them another day’s pay. Of course, this does not include the amount of money
they may have spent seeking health care from alternative sources of treatment. One woman
claimed to have spent Rs. 1000-1200 on her care in a private facility to no avail, and then
someone recommended she come to KEM. This study was conducted to get a sense of why
people chose to come so far to seek care. At the end of everything, more than the actual
treatment, it was the fact that the doctors were attentive, focused, spent time listening to each
patient, and generally had an affable manner about them.
Although this is quite similar to what was observed in the municipal dispensary, some of the
interviewees’ biggest complaints were that the doctors in the dispensaries did not treat them with
respect and dignity. The affable manner can be related to several different issues:
The residents are fairly young and were able to work with peers of a similar age group
KEM has each and every facility that is required for a doctor to come up with a proper diagnosis
The residents expressed that the emphasis on quality came from the senior management,
underscoring the administration’s commitment to quality of care
There was a good team environment where the work was distributed evenly and senior doctors
were very supportive to the juniors
Through this observational analysis, it seems that most people want someone who can speak to
them nicely and help them out with whatever ailment they are having. They don’t mind waiting,
or traveling for days, they just want respect and affability.
The other side of this survey is that due to timing problems, many of the doctors were present
during the interviews. This could have skewed the results of the survey as perhaps the patients
did not want to seem ungrateful. In fact, some of these patients arrive at the hospital so desperate,
any form of care that results in better health is helpful. While the responses do show a positive
image of the hospitals, it is important to remember the conditions under which the survey was
conducted. It is also important to remember that this was just a small survey of the patients and is
not meant to be indicative of the entire population that utilizes it.
While this example is just of one of the best institutions in Mumbai, another municipal teaching
hospital- Sion (and LTMG Medical College) often bears the geographical brunt of the influx of
patients bypassing the primary health care system. Since Mumbai is an island city and has
developed toward the suburbs, the majority of the 3rd tier hospitals ended up in the southern part
of Mumbai. This creates major barriers to access in care due to the distance and time involved in
reaching these hospitals from the suburbs. Sion hospital provides a break in that geographical
barrier from the suburbs to “town-side”. As a result, Sion hospital bears the burden of most
emergency cases, transfers from peripheral hospitals, casualties, and most aspects of urgent care.
As a result, Sion’s services are compromised due to work-overload on physicians, scarcity of
resources, and difficulty in managing overcrowding.
Clearly, there are many complicating factors regarding efficiency and access at municipal
hospitals in Mumbai. Even though services are of high quality at 3rd tier hospitals, they are still
plagued by issues of overcrowding, lack of referral systems and non-utilization of primary health
care services. It is important to understand the detrimental effect an uneven distribution of
services ends up having on the entire public health system. Indeed, due to some of the
compromised conditions (financial and otherwise) at primary and secondary levels, the system
itself encourages uneven access to health care.
7.5 Inconvenient Timings
The MCGM’s timings for health posts and dispensaries are generally 9am-4pm. This is often an
inconvenient time for people who are employed. Leaving work and spending an unspecified
amount of wait time can contribute to the frustration with public health facilities.
7.6 Locations
As it was alluded to previously, the major 3rd tier hospitals are located in the southern part of
Mumbai, while the city has expanded toward the suburbs in the north and east. This is common
urban phenomenon known as urban sprawl, is leading to compromised access to public health
care and is increasing the market for private practitioners (both qualified and un-qualified). In
the surveys conducted of the KEM OPD ward, many of the patients that came from various
distances were unaware of the locations or services offered near their home. Apart from the ones
who had a negative perception of it, many claimed to not know the locations of the government
health facilities. This happens for many reasons:
Due to extremely large populations to be covered by community health volunteers (1 per a
population of 60,000), each home that is supposed to be visited is often not
Since word of mouth is the most common method of reaching out to communities, the lack of
awareness propitiates throughout the community
If people know of a 3rd tier hospital that is effective, they will bypass the primary health care
system regardless of proximity.
Additionally, there was no map of Mumbai that had explicitly drafted the locations, timings, and
doctors at each health facility. A pamphlet of that nature would be useful to promote the
availability of government health care services.
7.7 Vacancies
Wide spread vacancies continue to plague the MCGM health system. In K East Ward, as
mentioned previously, there are nine vacancies out of eleven positions for Medical Officer’s of
Health. This is in an area that already suffers because of the lack of the municipal hospital in the
ward. When the survey was conducted at KEM General Out Patient Department, the residents
working there also mentioned that they were not interested in working at municipal dispensaries
due to lack of resources and facilities. The general disposition of the MCGM public health
department seems rather apathetic in relation to the high rates of vacancies. It seems to be an
acceptable norm that should just be accepted. This further complicates the case for expecting
patients to seek primary health care. If a patient goes once or even twice and the doctor is not
there or has left early, it becomes a dysfunctional health care center for them. Further, due to a
hiring freeze due to budget problems a few years ago, there were no positions filled.
There are several reasons for wide-spread vacancies at MCGM. First, the salaries for doctors are
not at a standard of living that would be appealing to many young doctors and the older doctors
that have been MCGM position for years often wait to retire to get benefits. Secondly, there are
no incentives for working at a community service level. Thirdly, there are hardly enough
facilities at primary and secondary level that make a doctor feel like they can diagnose/treat a
condition without having to refer the patient to a tertiary institution for further investigation.
Finally, given the financial remuneration is so limited for doctors, many would prefer to start
their own practice or work in a private institution.
7.8 Quality Assurance
Quality Assurance or quality of care does not mean sophisticated or exclusive care, but is
concerned with fully meeting the needs of those who need the service the most, at the lowest cost
to the organization, within limits set by higher authorities. Quality of care is cited as the main
reason the interviewees at the KEM GOPD chose to travel to KEM for their care. One hundred
percent of the patients mentioned the doctors are facilities were good. The doctors spoke to them
nicely and the treatment was effective. One woman mentioned that it was “very clean” as
compared with other hospitals she had been to. These correlated with the residents’ comments
that the facilities and resources available to them helped them serve the patients better.
Additionally, the presence of systems and availability of “one stop servicing” is extremely
beneficial. Because KEM has everything from X-ray facilities to MRI’s, patients don’t need to
seek care elsewhere.
In summary, Quality Assurance, as a concept is a systematic way of ensuring and maintaining
“quality” of services and has proved useful globally. Quality of care has 3 dimensions:
Client’s perspective: What do clients expect from the health services?
Professional’s perspective: Do services follow health care provider’s professional standards?
Management or Administrative perspective: Are the resources being used productively? Are the
services efficient?
Through a collaborative initiative between the MCGM and XXX project, an action research
project was implemented in 2 wards: H East and G North. This included 17 health posts, 16
dispensaries, 2 maternity homes, and 1 secondary hospital.
The focus of the project was to look at providers as agents of change. The project was limited in
terms of its interaction with the community, primarily because the project was aiming to reach
the community through the providers. The overall goal was to ensure quality health services for
women within the context of reproductive rights and health. The objectives were:
Improve, strengthen, and increase quality and range of health care services for women at all
levels
Enable women to have access to gender sensitive and user friendly services
Develop and build capacity of staff at 2 wards, training, monitoring and evaluation, and health of
women
This project worked closely within the MCGM structure with senior decision makers and health
managers in planning and intervention. Also the project focused on the capacity building of staff
in counseling, communication skills, training skills etc. The project also promoted quality
assurance and monitoring and evaluation.
This quality assurance system was implemented over 4 years and the team took every initiative
to ensure proper planning and implementation:
Workshops, planning, experimentations and interventions
Advocacy
Research
And in order to make sure everyone felt involved in the process, they established committees to
serve as links to the system, conducted participatory research and gave feedback, took all efforts
to ensure administrative support, and involved key persons from the MCGM. The main issues
that needed to be addressed were:
Information needs of clients
Attitudes of staff toward clients
Communication process between staff and clients
Diagnosis and prescriptions given by CHVs and ANMs (Auxilliary Nurse Midwives)
Training and supervision of staff
Referral process
Use of routine data
This project was very well planned, but was not accepted by the staff and administration teams
as it was thought of as a foreign concept. The project was opposed from many sides, and most
people claimed to not receive enough support from senior staff. The project did accomplish some
formidable goals, including two manuals for clinical guidelines in reproductive health for both
makes and females and a referral process that is described in the next section.
7.9 Referral Systems
The nature of the way people in Mumbai access public health care facilities would be greatly
improved if there were a referral system in place. In most countries, if a patient needs to see a
provider for a specialty, they must go through their primary care provider first. However, in a
system where the public is free to access health care at any level, the primary health care system
in bypassed and the patient heads straight to the tertiary or specialty care. When patients choose
to seek care at their own discretion, resources for primary and tertiary care are wasted and
tertiary resources are exhausted. This was evident in the KEM General OPD survey, where many
of the patients came for such common health issues such as fever, cold, cough, backache and
dizziness. If these patients had gone to their primary health care facility, it would have saved
both the hospital and the patients time and money. A referral system was tried and tested at
MCGM by the Women Centered Health Project. The process is described below:
An effective referral system would ensure optimum utilization of the three tier health care
delivery system of the MCGM and therefore use the available resources:
I. Objectives of the Referral System:
To ensure appropriate utilization of available resources
To ensure accessible, affordable health care services
To ensure patient and provider satisfaction
II. Pre-Requisites of an idea referral system:
Well defined levels of health care services based on availability of specialty services
Standard referral protocols
Administrative guidelines agreed upon by appropriate authorities governing various levels of
health care facilities
A well defined and well implemented feedback system
Focus on client and client centered in nature
Involvement of public as well as private sector
Strategies to enforce compliance
II. The proposed system for MCGM
This was looking at a well defined three tiered system with health posts and dispensaries at the
primary level, secondary hospitals, maternity homes and post partum centers as secondary and
teaching hospitals. The way it was proposed to work was that the priority would be given to the
referred patient. Patients being referred were getting a specially designed slip and would be
afforded benefits at the primary level.
This entire process did not work in the end because some of the staff were not clear about the
referral slips, this led to further patient dissatisfaction, people were unclear about how the system
was supposed to actually make things better.
This process is also being implemented through an NGO called SNEHA (Society for Education,
Health and Action for Women and Children). CINH (City Initiative for Neonatal Health) is a
collaborative initiative between the SNEHA, the International Perinatal Care Unit (IPU), UK and
the Bombay Municipal Corporation (BMC), CINH uses participatory techniques to involve
community members in urban slums and municipal health service providers to achieve:
• Improvements in maternal and newborn care practices and care seeking
• Provision of high quality antenatal and postnatal care at public health posts
• Continuous quality improvements for maternal and neonatal services at maternity homes and
hospitals
CINH has three essential components:
Improving public health systems
Improving maternal and neonatal health outcomes at the community-level
Developing these supply and demand interventions into a replicable model for urban slum
settings
A four-pronged approach will address these essential components:
Improvement in the quality of maternal and neonatal health care in all levels through the
development of a formal referral system in the BMC. This includes implementation of clinical
and administrative protocols for referral and transfer. To ensure sustained change, the
Appreciative Inquiry model will be used in addition to supportive supervision techniques.
The participatory development of antenatal, postnatal and neonatal (APN) service package for
health posts was developed to build support at the community level.
The use of action-research cycles with community groups to improve maternal and neonatal
health outcomes. This low-cost intervention trains local facilitators to lead community groups
through a process of identifying local challenges in maternal and neonatal health and evolving
workable strategies.
The development of evidence-based models for urban slums by building action research projects
with a strong evaluation component. Each intervention is participatory and includes capacity
building for sustainability. [96]
As CINH is being implemented throughout various public health care facilities in Mumbai, it is
important to look at it as a replicable model that can be utilized universally throughout the
system. Such a model can lead to greater efficiency as well as increased quality assurance
throughout the process.
7.10 Lack of Awareness
Lack of awareness covers a range of categories, lack of awareness of the patients regarding the
availability, locations, and timings of government services; lack of awareness within the staff
about quality assurance and quality of care; and lack of awareness of the multi-dimensional
aspect of the MCGM’s programming. There is no availability of a map in of the health services
being offered in each area. This leads to the general lack of awareness of services offered by the
MCGM. Patients feel there is a free range for them to access services anywhere, regardless of the
inconvenience. Staff are also largely unaware of the overall goals for quality services and
perform on a “fire-fighting” strategy, in which only the exigent issues are addressed, and there is
little adherence to ongoing strategy planning and setting up goals and work plans. Finally, it just
seems that there is a great disconnect between the different aspects of MCGM programming.
While some programs get national level priority (Polio and TB), some of the other programs like
environmental health and primary health care delivery through the CHV’s is not set as a priority
for funding. Although these programs are multi-dimensional and could be inter-sectoral, the
programming tends to run in a vertical fashion, all working toward goals without thinking of the
benefits of a more horizontal approach toward programming.
7.11 Public Health Disaster Management
In light of the recent outbreak of avian influenza, the MCGM needs to have a separate cell that
deals with public health disasters and outbreaks of diseases. If there is a cell that monitors public
health outbreaks around the world and tracks them before they reach Mumbai. Having a team
whose expertise is public health disaster management would be beneficial to the public health
department. This team would consist of media persons, public health experts, hospital
administration team, doctors, nurses, pharmacists, and community health workers. In this
situation, the outbreak needs to be attacked through a multi-dimensional approach:
A media person can be in charged of the reports that go out to the press. In its current state, the
communication between the media and the MGCM is antagonistic with plenty of skirting the
blame.
Public health experts can help figure out medical and preventive strategies to address the
outbreak. Currently, various staff from many departments have been pulled from other work to
address this issue. There is no real assessment of how far Mumbai bas been affected, thus
creating a state of panic and fear.
A hospital administration team is critical to setting up an operation to deal with the possibility of
a public health outbreak. The hospital beds to be used for quarantine as needed should be
decided beforehand as well. This team can be responsible for carrying out administrative and
laboratory tests as needed.
Doctors and Nurses are needed to help any urgent needs related to people who have already
contracted the illness. These providers should be vaccinated (if possible) before hand to all
illnesses that pose a threat.
Pharmacists can ensure that medications needed for the outbreak are available and not expired.
They should ensure enough stock just in case an outbreak is likely.
Finally, community health workers are needed to help keep the community educated and not
panic; especially the communities that live in large slum populations. The MCGM has put out
pamphlets regarding the Avian Flu, however, they are only in Hindi and Marathi, thus excluding
a large part of the slum-dwelling populations and impoverished communities.
Addressing issues during a time of disaster are never smooth, no matter how well planned out the
process is. However, adequate planning and team preparation can help decrease the “learning”
that happens along the way. In other words, disaster management teams should be adequately
prepared beforehand so that while some things may require thinking on the spot, other processes
can go according to standard procedure.
7.12 Water supply and sanitation
To be added
7.13 Challenges from the Private Sector
According to a World Bank Study, nearly 82 per cent of all health spending in India is
private.[97] The increasing competition of the private sector of health care combined with a larger
disposable income of the middle class has resulted in loss of patients from the public to the
private sector.
These patients cannot necessarily afford the exorbitant cost of the private health care facilities,
but are willing to go into debt or risk their financial security to seek care in the private sector.
The reputation of public health services, unfortunately have become so negative that those who
can, and even those who can’t, will opt to seek care in a private facility. According to Dr. Sanjay
Nagral, “this was not the case 20-25 years ago, because back then people did access the BMC
services”. At that time, the private sector was also not as developed. This also helped keep the
system in check, as everyone from politicians to plumbers were accessing the system. Today the
average middle-class person or upper class person doesn’t think to use the BMC’s services. Even
the poor re-consider it at times. Even though there are segments of the private sector which are
too expensive for the average middle class to afford, they will still seek care there.
According to Lokshahi Hakk Sanghatana, a democratic rights organization, said in its report,
`Creeping Privatization in Public Hospitals in Mumbai — Private Profit, People's Loss'[98], that
public hospitals come forward and administer care during times of social strife such as natural
calamities, riots and outbreak of diseases, while private hospitals do not. The report claims that
the MCGM is moving toward privatization at most of the municipal health facilities. According
to the report, privatization of health facilities has been taking place in many ways — hospitals,
services such as blood banks, dialysis centers and intensive coronary care units (ICCUs) have
been handed over to NGOs or private entrepreneurs. If there are no private funds available, the
report says, and then the expansion projects are generally unavailable.
The MCGM collaborates with some private practitioners for tuberculosis treatment, but other
private practioners do not report having the same treatment regimen across the board for TB
treatment. These types of partnerships need more transparency and communication so the health
outcomes of the patient are not affected negatively. Further, out of approximately 40,000 hospital
beds in Mumbai, the MCGM holds about 10,000, which means that over 3/4ths of the beds are
under the jurisdiction of the private sector.
Newer complications are due to arise out of the latest trends in medical tourism. With foreigners
investing their dollars and pounds in private health care in India, the hospitals will make a lot of
money, no doubt, but again the poor will remain without quality or quantity in terms of available
services. According to a report in the Hindu magazine, “Only seven years from now, the most
optimistic industry forecast posits, medical tourists hosted by India can pump Rs. 10,000 crores
into our economy. An estimated 1,50,000 such visitors a year already spend about Rs. 1,500
crores in India for treatment.”[99] The major question everyone is asking is, what does this mean
for the impoverished citizens of Mumbai. Although private hospitals have obligations for their
not-for-profit status under the Public Trust Act to provide healthcare free to the extent of 20 per
cent of their resources, there is no accountability or follow-up for this provision. As a result, the
poor don’t even see private care as an option, thus the frustration ends up coming out on the
public healthcare system.
7.14 Reporting and Data Collection
The Mumbai Health Profile is put out every year (approximately) in order to give an update of
the health programming and accomplishments. What is missing from the report is an analysis of
the numbers reported. It seems very haphazard that the numbers are just reported without any
indication of what could have led to an increase or decrease. For example, there are no
explanations for why the TB numbers have fluctuated so much over the years. One can assume
that the different policies that have been implemented may have contributed to it, but the report
itself does not make a connection between the interventions and the numbers. The reporting
process is a critical part of showing the successes and challenges of the MCGM.
Another aspect of the MCGM that needs to be revised is data collection. For example, the School
Health Program is a successful intervention, but the data is not centralized so that there can be
effective epidemiological monitoring of growth, malnutrition, rates of TB and other illnesses,
and follow up. In order to decrease the paper burden, it is important to establish a global
information system that allows staff to input data and allows universal access to it from all
MCGM facilities. A centralized, computerized data system could result in increased efficiency of
the process. This would in turn improve the reporting process as well.
8. Appendices
a. Patient Bill of Rights
Each place posting the Patient Bill of Rights needs to affirm the following statement.
"We, the staff and the administration of {health facility} declare the following Bills of Rights
for the patients of this medical facility. As per the Municipal Corporation of Greater Mumbai, we
declare that staff and administration of {the health facility} have read and understood the
following rights of a patient and hereby agree to all the terms listed below. If you have any
questions or complaints, please contact {Name of accountable person at health facility} or {name
of accountable person at BMC}."
To be treated with dignity irrespective of their caste, class, sex, religion, and disease
To have a list of exact services available and corresponding fees (for supplies, bandages, etc)
To have a visible map of the hospital (in Marathi, Hindi, English, and other languages)
To have a list of emergency services such as blood banks and ambulatory services listed in
Marathi, Hindi, English and other languages
To know and understand the procedures involved
To be given a reasonable time frame for the treatment and receive a proportional discount in fees
for all services after the upper limit of approximation is over and treatment needs to be continued
To have a comprehensive (various tests, blood work, x-rays, room tarrifs, operations, consulting
fees, etc) costs associated with seeking medical care
To receive prompt and courteous care
To be informed about the documentation needed for treatment
To have minimal documentation for emergency cases
To receive Reproductive and Child Health Services free of cost at public health facilities
To receive medications and vaccinations from the local public health post or dispensary
To get medical services which are within the capability of the medical facility
To obtain from the doctor complete information concerning the diagnosis, treatment, and
prognosis in language the patient can understand.
To receive necessary information from the doctor such as long-term effects, side effects etc.,
before giving any prior consent to a medical procedure and/or treatment
To receive the records or a certified copy that gives the details of the disease, treatment, and
follow-up necessary at the time of discharge
To refuse the suggested treatment and be informed of the medical consequences thereof
To receive medical care in well-equipped and sanitized conditions
To receive quality care from competent medical professionals
To select doctor’s of one’s choice when possible
To obtain a second opinion
To privacy during medical check-ups
To be assured that all communication and records will be kept confidential
To educational information about medical problems eg. via a library, IEC materials, etc.
To receive a bill cum receipt after the payment is made
To be enabled to pay hospital fees on a payment plan
To have access to a non-hospital staff member appointed to address complaints as soon as
possible
To have the contact information of the responsible person (both at the hospital and head office)
to register a complaint or give feedback
To have adequate waiting space
To allow relatives to have flexible visiting hours
b. Patient Code of Conduct
Patients are also responsible for their personal and environmental well-being. The following
code of conduct emphasizes the responsibilities of a patient while seeking medical care.
As a patient:
You should provide the doctor with accurate and complete information about his/her medical
history, past illnesses, allergies, hospitalizations, and medications
You should report the changes in your medical changes
You should ask for clarity if the doctor’s prescription and diagnosis seem unclear
You should follow the doctor’s treatment plan
You should pay your medical bills promptly
You should follow hospital rules and regulations
You should have realistic expectations of what the doctor can do for you
You should help your doctor help you, if something isn’t working, be clear and the doctor can
advise alternative care
You should participate actively in your own medical care (in terms of awareness and
preventions)
You should ask the doctor questions to clarify any doubts or misconceptions in your mind
You should treat the doctors with respect
You should not ask doctors for false bills or certificates for any reason
c. Probable Value of the Report
In this section, the author has outlined how the report can be of value to the different existing
bodies in the city of Mumbai. The report was not only created for the MCGM, but also for all the
other proponents of health care in Mumbai. The following section details to value to each
constituency:
MCGM: This report should be seen as an objective analysis of the existing programming at the
MCGM. In addition to giving suggestions, the report also highlights the various successes of the
MCGM’s health programming. It will be of value in several aspects:
Assist lawmakers in allocating funds to priority areas
Provide insight to those responsible for programming in terms of areas of improvement
Increase the efficiency of the MCGM public health department
Increase the reputation of the MCGM’s health services in the city
Prove as an impetus that demonstrates the MCGM’s priority of the health of the people of
Mumbai
Intimate the top-level management as to the priority areas in various departments
Apprise mid-level management of the awareness of the lack of resources
Inform lower-level staff of the value of their work and increase worker morale
NGOs: Non-Governmental Organizations working in Mumbai are working to provide health care
to the same citizens that are also the responsibility of the MCGM. This report can help bring the
two groups together to not replicate programming in high-need areas and pave the way for NGOMCGM partnerships. NGO’s can cite the information in the report as representative of the
enormous need for improved health care systems in such a large and densely populated city.
Donors: With Corporate Social Responsibility representing the progressive era of charitable
giving, it is important for donors to also be aware of the issues that are effecting the communities
that benefit from their time, money, and resources.
Citizens: In a city like Mumbai, the average citizen doesn’t think about health care unless it is a
situation of urgency or crisis. This report will make citizens aware of the issues in health care
that effect all those seeking care through the government health sector.
Medical Students, Physicians, and Health Professionals: In light of the recent strike of the
doctors in Mumbai, it is also important for policy makers to understand the perspectives of those
working on the ground. This report helps shed light on the needs of physicians and avenues for
improvement in their occupation.
Media: The MCGM health department is often the recipient of negative publicity by the medial.
The information in the report can offer some information as to the inner workings of the MCGM
health department and what the media can do to support the improvement of these systems.
Overall, the report provides an in-depth analysis of the existing programs, challenges, and
successes of the MCGM health department. Looking at the history of health policy in India, it is
evident that there has been little emphasis on improving the health of local citizens in recent
years. The report attempts to create a common area for discussion and improvement of health
systems within this city. With good basic infrastructure, there are many avenues that can be
pursued if the aforementioned parties join together to work on a healthy Mumbai.
d. Training Activity for the BMC
Organizing and Managing Urban Health Services:
Identify the guiding principles of the municipality- If they are not explicit, they should be
drafted.
Example: Is the guiding principle equity of access, ensuring a simple, basic minimum package of
health care is accessible to all?
Is collaboration between health and other sectors, such as education a guiding principle?
Purpose of the Municipality:
Is it to provide appropriate and affordable primary health services for the entire city population?
Or is it to provide for the poor, and to facilitate private service provision for higher income
groups?
Assess the internal environment
Are the resources available? (Staff, money, infrastructure)
The current structure and stated function of the government services
Various service tiers
Needs careful delineating
Evaluate the External Environment
Current national policy, with direct respect to direct provision of service compared with
promoting and regulating the private sector
Direction of decentralization
National policy for health sector financing
National norms setting service standards or configurations
Level of flexibility within the BMC in interpreting these policies
Goals and Objectives
Use these to formulate a strategic plan
Broad objectives
Operational objectives
Key areas to consider:
Current decentralization policies altering government and administrative structures,
The debate over government health service tiers
Relationship between government and private sector
Institutional development to improve managerial capacity in government health services
*Private sector notes:
-The quality of care of private providers varies a lot from very high to very low.
-In low income areas, care is often of low quality
-Even if private providers are more polite, the quality of care is not necessarily better
-Private providers are driven by market forces
-Preventive measures are often neglected
*Governments have a definite responsibility to ensure a minimum quality of care to protect the
population from the adverse effects of healthcare:
Healthcare is important because it relieves suffering
Healthcare is dangerous, especially if inappropriate therapies are given.
Governments can consider voluntary accreditation of the private sector.
e. Integrating public health issues into the LACGs
With the recent success of the LACG’s for the littering rules and other community issues, it is
important to use this resource to address issues of public health as well. The type of activism
coming from these groups can be well-utilized as a springboard for other community problems
that need the focus and energy of an organized constituency.
The following ideas can be incorporated:
Circulate a brief summary of the Public Health Policy Document
Each LACG can identify its area of priority and take up a particular issue in health (i.e. child
health/school health, health of pregnant mothers etc)
This can be a yearly campaign for the LACGs to work with the local MCGM health
centers/dispensaries
The Bill of Rights and Code of Conduct can be promoted through these groups as well
f. Apex Health Committee
Possible Members:
Dr. Ratna Magotra, Former Cardiac Surgeon at KRM
Dr. Janaki Desai, Niramaya Health Foundation
Ms. Dipika Banerjee, Program Director, AVSAR
Role of Committee:
The role of the committee will be focused on:
Promoting the relevant recommendations in the report
Being the voice for public health issues for the NGO Council
Approving appendices and annexures for other health topics not yet covered in the report (mental
health, sanitation & water issues, etc)
Meeting once a month to monitor progress of the MCGM on proposed issues (i.e. new
programming, follow up, recommendations etc.)
g. Author’s Note
Although the concept of public health dates back to ancient times, the practice is something
relatively new and upcoming in the world space. The idea of conducting an analysis of the health
care system in Mumbai was not only challenging, but a part of this growing awareness of public
health as a critical force in the medical/health world.
The challenges I encountered while writing this report taught me a lot about public health and its
applications in India, a nation with so much potential. Going through all the health policies of
India, identifying the key areas of importance, summarizing 200-400 page reports, meeting with
people that were either very willing to help or willing to make it harder and finally meeting the
patients who came the hospitals, health posts etc to seek medical care. The challenges greatly
outweighed the benefits of writing such a report.
The most important question we should ask at this point is: why wasn’t a report like this written
years ago? Unfortunately, this seems to be a trend in global public health, with decreased
funding and low priority given to health systems and public health. All things are inter-connected
here- how 26 July 2005 effected health to the recent striking doctors- in terms of the long-term
affect of negligence on the importance of providing high quality medical care for the masses. I
hope that this report can add value to the hard work of NGOs, MCGM, and all the other groups
involved in bringing health care to the masses.
Overall, this project was of great value to me and I hope it serves as a springboard for those
wishing to promote the benefits of good public health systems in Mumbai and all over the world.
Thank you for entrusting me with such a task.
Meenakshi Verma
March 2006
Appendix 1
Questionnaires
Mumbai Public Health Policy Framework
Questionnaire for Utilization of Tertiary Health Care Services
Date:
1. Age
2. Location
3. Address
4. Occupation/Education
5. Why did you come here for your
medical services?
6. What stopped you from seeking
care close to your house?
7. How much did it cost you to come
here today?
8. If the services were closer to your
home, would you access them?
9. If you feel comfortable, can you
share your health problems with us?
10. What do you like about the care
here?
Comments or Concerns:
Data Number:_____
Entered:_________
Mumbai Public Health Policy Framework
Questionnaire for Utilization of Primary Health Care Services
Date:
1. Age
2. Location
3. Address
4. Occupation/Education
5. Why did you come here for your
medical services?
6. Do you ever seek care at a hospital,
why?
7. How much did it cost you to come
here today?
8. If you feel comfortable, can you
share your health problems with us?
9. What do you like about the care
here?
10. How long was your waiting time?
Comments or Concerns:
Data Number:_____
Entered:_________
Appendix 2
Health Post Survey Results- Vashi Naka Health Post, Chembur
Ag Sex Locati Occupati Educati Q1
e
on
on
on
A 35 Fema VNHP housewif none
cold,
le
e
fever,
cough
B 12 Male VNHP Student
4th
TB
C 18 Fema VNHP Student
le
11th
comm
fever,
cough
D 55 Male VNHP Business 10th
E 20 Fema VNHP Makes
le
ganpati
statues
F 17 Fema VNHP None
le
G 25 Fema VNHP None
le
5th
H 17 Fema VNHP None
le
7th
Q2
Q3
Q5
Q6
goes to
Mah
hospital
sometimes
Only
diagnosis
was there
No
Free Medicine
is good
no
Free Medicine
is good
Rs. Medicine
10 is good
Waited for 1 hour
Free Medicine
is good
and it
works
Waited for 1 hour
Waited for 1/2
hour
Free Everything No wait time
is good
Free Medicine Waited for 1 hour
and check
up is good
4 year
Went to
Free Gave
Waited for 1/2
old child shetabdi
medicine hour
has TB hospital and
but
felt kicked
waiting to
around
see if it
feels he
works
doesn't
know what
is going on
medically
with the
child and
no one is
giving him
a straight
answer
Boil on No
Free Medicine Waited for 1/2
neck
is good
hour
10th
TB
12th
fever,
cough
Goes to
private
doctors
sometimes
vomitin no
g,
diarreah
Waited for 1 hour
I
27 Fema VNHP None
le
10th
J 29 Male VNHP None
5th
K 55 Male VNHP None
none
L 35 Male VNHP Plumber 6th
M 26 Fema VNHP None
le
6th
N 22 Fema VNHP None
le
none
O 64 Male VNHP None
5th
P 18 Male VNHP None
none
Q 26 Fema VNHP None
le
5th
R 7
none
Fema VNHP None
le
children comes to
Free Doctor is
have
dispensary
good,
fever
first, then to
medicine
hospital
is perfect
TB
no
Free Medicine
makes a
difference
TB
Goes to
Free Facility is
Shetabdi
good
sometimes
TB
No
Free Doesn't
know
stomach No
Free Everyone
illness
here is
and
good
fever of
children
Fever,
Private
Rs. Its ok
cough, providers
20
cold
TB
Somaiya
Free Good
because he
gets his
medication
s on time
TB
No
Free Doesn't
know
Children Rajawadi
Free 1st time
are not Hospital
here, if it
well
works, she
will come
back
Girl has Went to
Free Care is
a huge Sion
better
boil
Hospital
and they
told him to
come here
TB
No
Free Medicine
is good
S 15 Fema VNHP None
10th
le
T
Appendix 3
KEM General Out Patient Department Survey Results
Ag
e Sex
Occupatio Educati
Address n
on
Q1
Q2
Q3 Q4
Q5
Waited for 1/2
hour
No wait time
No wait time
No wait time
waited for 2
hours
No wait time
No wait time
No wait time
No wait time
No wait time
No wait time
Q6
N/ Fema
A le
Wadala
N/
A Male Wadala
Fema
13 le
Worli
Housewife N/A
Carpentar
N/A
9th
7th
Fema Ullhasna
30 le
gar
Housewife 5th
Sakinak
a,
N/
Andheri Embroider
A Male (E)
y Worker N/A
No cure
despite
repeated
medicine
s
No relief
Referred
by a
private
doctor
Patient
had
already
taken
treatemen
t from a
BMC
health
post but
was not
cured.
Went to
Goyal
hospital,
didn't
make a
differenc
e,
although
it was a
private
hospital,
it didn't
make a
differenc
e, also
the
doctor
spoke
rudely
local
doctor
advised
him to go
to the big
Not
improved
despite
treatment
Not
improved
despite
treatment
30 No
Fever, Good Doctors, and
Backac good facilities for
he
patients
Believes KEM
Fever, cures Malaria
no
better than other
access centers, good
to clean investigation
water
services
16 Yes
Cough,
vomitin
g, fever
and
chills
20 No
No health
facilities
close to
home (that
she was
aware of) 50 Yes
Did not
know if
there are
BMC
facilities
30 Yes
Good doctors and
lots of good
facilities are
available
Chest
pain,
Doctors spoke to
fainting her nicely
Doctors, and he
doesn't know
about the
investigation
N/A
facilities
hospital
Fema Grant
24 le
Road
Not
workin
New
Shipping
32 Male Mumbai Company
46 Male Parel
Factory
Worker
Rajapur
36 Male (Village) Driver
6th
Went to
Nayyar
hospital,
but that
was not
helping,
so she
came to
KEM
12th
Company
friend
said to
come to
KEM
N/A
10th
close to
his home
Services
not good
at health
post, the
problem
was more
severe
than they
could
handle
She came here
from other people
telling her it was
Migran good, Nayyar was
e
good but the
headac medicine was not
hes
working
20 Yes
Indira
Gandhi
hospita
l is
there,
but the
faciliti
es are
not so
70 good
Hernia
Everything is good
here. Good people
and doctors
Fever,
cold
Doctors treated
him well, his
mother also comes
here
Doesn't
know any
other
facilities
No health
posts near
his home
He had a (that he
fever and was aware
a cold
of)
0
No
Yes,
there
are not
In the
many
village,
service
his BP
s in the
went up
village.
and he
Even if
had to
Not many
someo
come to health
ne gets
KEM for services in
sick,
further
the village
they
tests.
(475 km
have to
Jijaji sent from
25 travel
him.
Mumbai) 6 95 km BP
Treatment is done
well, and they take
time and do good.
In the village, they
give an injection,
and it doesn't work
well. It is good. Its
not easy to handle
that many people.
Fema Bhayend Saleswom
30 le
ar
an
12th
Tried at
2-3
private
hospitals,
nothing
helped
Fema
Houseclea
40 le
Andheri ning
7th
Municipali
ty hospital
is there,
but they
don't give
enough
Dizziness attention
Fema Matunga Works for
50 le
Road
a company 11th
Feels Sion
and KEM
are the
Dizziness same.
Lower
45 Male Parel
Bus
conductor 10th
Fema
Not
59 le
Bhandup workin
60 Male Parel
Not
working
7th
10th
Lump in
finger
Lives in
the
village,
but came
here for
care
Shoulder
pain and
stomach
problems
No public
care (that
she is
aware of)
This is
closest to
his house
If you come 1-2
times you get
Yes,
better relief. The
left
procedure has
home
become a little
at 7am,
complicated, it
nothin
used to be better
g close
when people were
to her
prioritized based
20 house Acidity on illness
Yes.
There
is a
doctor
at the
munici
pal
hospita
l, but
he
Treatment is
hardly Lymph effective and
50 comes nodes doctors are good
Yes,
all the Dizzine
current ss,
ones
frozen Doctors are good
are
shoulde and money is
8 private r
saved
Primar
y
health
center
is just
for
Lump
basic in
0 care
finger Doctors are good
N/A
0 No
Came
from the
village, so 40
doesn't
0 No
General
pains in
knee,
hip, and
chest
Should
er pain
and
stomac
Everyone talks
well and I like the
hospital
Doctors and
facilities are good.
Those who leave
here, leave well
know
about PHC
29 Male Sewri
Driver
Fema Elephisti Not
30 le
ne
working
Fema
35 le
Worli
48 Male Malad
Not
working
Tailor
8th
7th
10th
5th
Service
s
There are
current
municipal
ly are
hospitals,
good,
but no
but
doctor
doctors
facilities
are not
but not
availab
Headache gone there 10 le
There is a
clinic on
Saini
Road, but
only goes
there for
immunizat
Backache ions
0 No
Doctor
s are
better
here,
There are
rupees
(Facilities)
are
Health is but small.
comple
not good Its ok.
10 te here
There is a
Yes I
KEM
would.
branch in went to
There
Malad,
the PHC in
is an
but
Borivali
ease to
medicine but there
the
is not
were
10 service
available, problems 0 s here
h
proble
ms
Headac
he,
dizzine
ss
Treatment is good
Doctors are good,
cleanliness, and
care is good. Other
hospitals Nayyar
Backac and Sion are not
he
clean
Cough
and
Pnemo Full treatment is
nia
good
Baby
has a
respirat
ory
infectio
n
Doctors are good,
except sometimes
the care is
compromised
II. Best Practices
Utilizing best practices from other cities with similar challenges in terms of healthcare can
improve the health outcomes of the city of Mumbai. The following section further analyzes
several of these best practice models.
a) Participatory Budgeting in Porto Alegre, Brazil[100]
Until the beginning of the 1980s, Porto Alegre experienced accelerated population growth, which
left one third of its population with only marginal access to urban infrastructure. In 1989 a large
proportion of the population lived in non-legalized areas, in shacks without drinkable water,
sewerage systems or paved streets. Local government decided on all municipal investments,
without any consultation of residents. However, the city's income, which was based on taxes
collected, was not adequate to finance even a minimum of public works needed to sustain
development.
Participatory budgeting was introduced as part of the political platform of the Labour Party in
1989 to involve the residents in setting priorities for public works; ensure a more equitable
distribution of municipal investment; promote transparency in municipal activities and reduce
opportunities for corruption; and increase popular participation in municipal government.
Following its introduction the program gained strength as the public gained more experience in
decision making and as tax reforms strengthened municipal finances.
The program has developed into an international model of participatory government. The general
rule that applies is that there is a direct connection between the spending in the local
neighborhoods and what motivates people to attend meetings. If you don’t attend a meeting for
your district, chances are that your road light won’t be working. Since participatory budgeting
began in Porto Alegre in 1991, over $700 million has been invested in basic urban infrastructure,
including water supply, sanitation, road improvements and public lighting. An opinion survey at
the end of 1997 showed that 85 percent of city residents either had been active in the budgeting
process or considered the investments to be highly relevant to their circumstances.
In 1990, when the program started, people thought it wouldn’t work, so only 1000 people
participated. In 1999, over 40,000 people were participating. The concept is simple, Porto Alegre
is divided into 16 districts for purposes of the budget. A council is created in each district as a
space for citizens to meet and discuss spending priorities. Meetings are open to anyone who
would like to attend. Citizens set two priorities: district and citywide spending. District spending
focuses on specific public works projects in the neighborhood, such as paving streets or
improving sewer systems. Citizens identify three priorities, with funds allocated based on
population size and need. Need-based allocation of funds means that poorer neighborhoods
receive more money than wealthy ones.
World Bank study found substantial quality-of-life improvements in Porto Alegre:
Between 1989 and 1996, the percentage of the population with access to water services rose from
80% to 98%.
Those served by the municipal sewage system increased from 46% to 85%.
The number of children enrolled in public schools doubled.
In poorer neighborhoods, 30 kilometers of roads were paved annually.
Tax revenue increased by nearly 50 percent, a fact the World Bank attributes to “transparency
affecting motivation to pay taxes.”
The MCGM is plagued with issues of transparency and disclosure regarding how decisions are
made in the domain of health. It may be worthwhile to explore small levels of participatory
budgeting and see how that might be of value to the citizens that utilize the public health sector.
b) Cambodia’s Non Profit Path to Health Care
Cambodia’s public health care system was plagued with some of the same issues that limit the
potential of the MCGM Public Health Department. Large scale absenteeism, vacancies, and
corruption caused massive under-utilization of the public health care system. However, the
government decided to take a low-cost approach to improving health care for the poor by
contracting international or local non profits to run the health centers and hospitals at a fraction
of the cost. The approach is catching on in a growing number of poor countries around the world,
from Bangladesh and Afghanistan to Congo and Rwanda, to Bolivia and Guatemala, reaching
tens of millions of people.
These contracted services have allowed international donors and concerned governments to cut
through dysfunctional bureaucracies - or work around them, and to improve health care and
efficiency at modest cost. In Cambodia, the nonprofit groups - all of them international - are
instilling discipline and clarity of purpose in a health care system enfeebled by corruption,
absenteeism and decades of war and upheaval. They have introduced incentives to draw
Cambodia's own doctors and nurses back into the system. Patients, especially the poorest ones,
have followed in droves. The international NGOs are paid based on performance, based on their
ability to achieve immunization targets, decrease Infant Mortality Rates, and make sure women
are getting prenatal care and following up with institutional deliveries.
Although Mumbai does not seem to be at the same level as Cambodia at this time, there can be
potential benefits to having foreign NGOs setting up and running operations to improve
efficiency and subsequently transitioning to a local team.
c) Subsidized Health Care in the Philippines[101]
The Makati Health Program (MHP) was designed to provide residents of the city of Makati in
the Philippines earning monthly incomes less than US$156 access to quality health care.
However, when the program was evaluated in 1986, they found that people in that income
bracket were unable to afford the health care provided by the MHP. The local government of
Makati partnered with the private sector partner, Makati Medical Center and two NGOs.
The program has afforded beneficiaries access to services such as major surgeries in one of the
best private hospitals in the Philippines. In 2000, over 50,000 cardholders were treated at the
Makati Medical Center, with bills totaling US$ 3.3 million. Under the terms of the expenses
sharing scheme, the city government of Makati shouldered US$1.9 million while Makati Medical
Center contributed US$1.4 million.
Together with the local government's initiatives in preventive health care, the Makati Health
Program has contributed to declines in the mortality rate and improvements in morbidity rates
across all ages. Makati is one of the few cities in the Philippines that provide subsidized quality
health care to its constituents.
The idea of health subsidies can be a good idea for the MCGM Public Health System. Utilizing
the networks of private hospitals in the city, there can be value added if both the government and
the private sector actively participate in improving health care for all.
All the different initiatives mentioned above are merely suggestions for improving aspects of the
MCGM health systems. Clearly, the process of implementing different strategies is going to be a
challenge, but the use of best practices from other institutions should be a good starting point for
those positive about changing the system.
Works Cited
Understanding our Civic Issues, The Bombay Community Public Trust, Health Services in
Mumbai, 2004.
Public Private Partnerships for Improving Health of Children in Urban Slums,
Dr. Siddharth Agarwal, Urban Health Resource Center, 2005.
“Unmet needs for Public Health Care Services in Mumbai, India”, T.R. Dilip and
R. Duggal, Asia-Pacific Population Journal, 2004.
“Mumbai’s Invisible People”, The Hindu, November 2005.
“Maternal Care in India Reveals Gaps Between Urban and Rural, Rich and Poor”, Population
Reference Bureau, July 2003.
“The USAID/India Urban Health Program: An evaluation of activities to date and
recommendations for the future”, October 2005.
World Health Organization South-East Asia Regional Office, Vol. 3 Issue 2, September 2003
Health Concerns and Organizing Health Care Delivery to Urban Slums, Dr. Siddharth Agarwal,
Urban Health Resource Center, 2005.
Health Delivery and Health Wants In Mumbai Slums, India, Centre for Water Policy and
Development, University of Leeds, Date Unvailable.
Country Health Profile- India, World Health Organization, 2002.
National Family Health Survey, Maharasthra, March 2000.
Report of the National Commission on Macroeconomics and health, Government of India, 2005.
US AID Health Report, 2002.
Personal Interviews with Dr. Sanjay Nagral, Dr. Khandare, Dr. Ambe, Dr. Thanekar, Dr. Usha
Ubale, Dr. Janaki Desai, Dr. Armida Fernandez, Ms. Leena Joshi, Mr. Ravi Duggal, Dr. Ratna
Magotra
National Health Policy 2002 & 1983
Moving Toward the Right to Health Care, CEHAT, 2005/
BMC Health Profiles 1997-2004.
National Health Policy 2002.
http://phm-india.org/pdf/hungerwatch/draft_guidelines_starvation.pdf
http://www.maharashtra.gov.in/english/ecoSurvey/ecoSurvey1/economySurveyShow.php
www.blonnet.com/2005/11/16/stories/2005111601821300.htm
www.hindu.com/2006/01/01/stories/2006010104671200.htm
www.hindu.com/thehindu/mag/2005/04/17/stories/2005041700060100.htm
www.worldbank.org/
www.earthinstitute.columbia.edu/images/TheLancet_slum_dwellers.pdf
www.hindu.com/2005/11/03/stories/2005110304381100.htm
www.mezomorf.com/health/news-19949.html
www.indianpediatrics.net/feb2004/137.pdf
Urban Health Resource Center: http://www.uhrc.in/
WHO Newsletter: http://w3.whosea.org/extrelations/pdf/vol3-2/RD%20mess.pdf
www.swissre.com/INTERNET/pwswpspr.nsf/alldocbyidkeylu/BMER-5GBLEN?OpenDocument
www.wikipedia.org/wiki/Mumbai