Pseudomonas aeruginosa, Staphylococcus aureus, and E.coli.
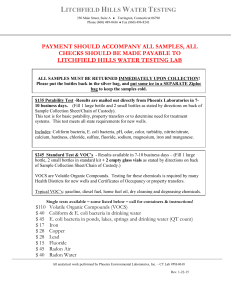
advertisement

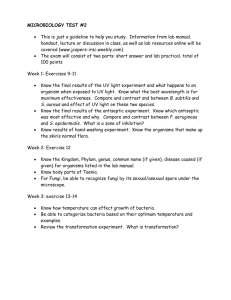
The Effectiveness of antiseptics on Pseudomonas aeruginosa, Staphylococcus aureus, and E.coli. By: Abigail L. Stowell (Animal Science), Amy Poss (Biology), and Amanda Steffens (Biochemistry) Abstract Antiseptics are essential in controlling bacterial populations on the skin surface. The effectiveness of antiseptics is dependent on several properties: fast acting with a prolonged duration of activity, activity against all likely contaminants and pathogens, nontoxic, noncarcinogenic and non-teratogenic (does not cause malformation of embryo or fetus) to host cells, and having minimal systemic absorption. The effectiveness of these antiseptics on gram-positive and gram-negative bacterium differ depending on the antimicrobial action of the drug. The antimicrobial activity of a drug on a bacteria can be inferred by disk diffusion, Minimum inhibitory concentration (MIC), and Minimal bactericidal concentration (MBC) tests. These tests were used to determine the level of activity and the effectiveness of nitrofurazone, iodine tincture and hydrogen peroxide against Pseudomonas aeruginosa (PA), E. coli (EC), and Staphylococcus aereus (SA). The results of these tests demonstrated that iodine was most effective as a bactericidal agent in all three of the bacteria SA, PA, and EC. Methods: Background Iodine tincture (2.4% Sodium Iodide and 47% alcohol) is believed to kill bacteria, by precipitating or congealing the bacteria’s proteins through halogenation with free iodine. This activity can be increased by lowering the pH. Iodine tincture is broad spectrum, meaning it is effective against a wide variety of microorganisms. It has Unfortunately its activity is limited to only 4-6 hrs and its absorption into damaged skin and mucous membranes can increase serum levels 104 times normal levels. If pregnant, this can penetrate the placenta and eventually cause hypothyroidism or goiters in the fetus. (Fig.1) Chemical Formula: K+[I-] Hydrogen Peroxides bactericidal activity is attributed to its oxidizing ability. It is relatively unstable and when in warm conditions tends to degrade into water and oxygen. It is a relatively weak antiseptic and therefore is used primarily for cleansing wounds only. Because of its instability, also has a very short half-life. (Fig.2) Chemical Formula: Nitrofurazone is a bactericidal agent, with a broad spectrum of activity. It is primarily effective against most gram-positive bacteria and facultative gram-negative bacilli. Topical nitrofurazone is not absorbed into the blood to any substantial degree even after extensive use. Sensitive bacterium contain a flavoprotein reductase that causes the transformation of nitrofurazone into a chemical that reacts with proteins. (6). Discussion: Results: Test I. Disk Diffusion Using an inoculation loop and aseptic procedures, a culture of SA, EC, and PA was prepared. The cultures contained thee loops of bacteria and 10 ml of Nutrient broth. After preparing cultures they were incubated at 37°C for 24 hrs. Mueller Hinton afar was prepared using 38g of mix per liter of distilled water. 39 sterile Petri dishes were filled with 20ml of agar per plate. The plates were left to cool and were stored in the refrigerator till used. After the 24hr. incubation period, 13 plates per bacteria were inoculated using a sterile swab and swabbing in a continuous pattern in three directions to form a bacterial lawn. Nine absorption disks for each antiseptic (Neosporin, nitrofurazone, iodine, and hydrogen peroxide) were prepared by soaking them in an antiseptic. Excess antiseptic was either left to drip off or was scraped off using a sterile forceps. The disks were separated out into sterile Petri dishes and allowed to dry in the 37°C incubator for 10 minutes. After drying absorbance disks were placed onto the plate cultures. For each bacteria three absorbance disks of each antiseptic was tested (1 disk/plate). A control using a blank disk was prepared for each bacteria. The plates were incubated again at 37°C and clearance values were taken from each at 24 and 48 hrs (As in Fig. 7). Neosporin was eliminated from further study because of its inability to diffuse on the plates. P. aeruginosa E. coli S. aureus Iodine 10.00 mm 12.67 mm 9.67 mm Hydrogen Peroxide 17.37 mm 18.67 mm 17.33 mm Nitrofurazone 15.53 mm 10.67 mm 25.00 mm Test I. Disk Diffusion discussion (Table 1 and Graph 1): The disk diffusion test provided evidence that iodine and hydrogen peroxide maintained consistent results among all three species bacteria. Nitrofurazone demonstrated the greatest degree of effectiveness on SA (gram-positive). Our results showed that Nitrofurazone was less effective against PA and EC (gram-negative bacteria). Hydrogen peroxide had the greater clearance on gram-negative bacteria, than did iodine and nitrofurazone. Iodine and nitrofurazone illustrated variable diffusibility on Mueller-Hinton agar. The nitrofurazone had an extremely high standard deviation, while iodine and hydrogen peroxide’s clearance values were more consistent. This could be due to nitrofurazone’s relatively gel-like physical state at room temperature, and could possibly affect its diffusibility and hinder the experimenter’s ability to maintain equal concentrations of antiseptic on the disks. Average Table 1. Average Zone of inhibition (mm) after 24 hour incubation Test II. MBC Discussion: The MBC results were disregarded because the bacterial growth in the broth was too large of an amount to affected by the antiseptics used. An actual human wound would most likely never contain the large amount of bacteria we had in our test tubes. Under realistic conditions, one would place antiseptics on the wound before it would ever reach such large quantities of bacteria within 24 hours. 35.00 30.00 25.00 (Fig. 3) Chemical Formula: O NO2 CH=N-NHCONH2 The bacteria used in the experiments were Pseudomonas aeruginosa, Staphylococcus aureus, and E.coli. Pseudomonas aeruginosa (Fig.4) is a Gram-negative, aerobic rod. They are common inhabitants of soil and water, but can also be found on the surface of plants and animals. This bacteria is an opportunistic bacteria. If given the chance it can cause urinary tract infections, respiratory system infections, dermatitis, soft tissue infections, and a variety of systemic infections, particularly in patients with severe burns, cancer and AIDS patients who are immunosuppressed. The bacterium is respiratory and never fermentative, it can grow in the absence of O2 if NO3 is available as a respiratory electron acceptor. Pseudomonas aeruginosa is often observed growing in "distilled water" which is evidence of its minimal nutritional requirements. Its optimum temperature for growth is 37° . This bacteria is also know for it’s resistance to antibiotics. It’s resistant to so many because of it’s permeable barrier provided by its outer membrane lipopolysaccharide. It also maintains antibiotic resistant plasmids (rfactors) which can be passed on to later generation. Staphylococcus arueus (Fig.5) is in the Bacterial family Micrococcaceae, and are Gram-positive spherical bacteria that form clusters that look like grapes. Each spherical cell is about 1 micrometer in diameter. Staphylococcus arueus form large yellow colonies in rich mediums. It can grow at a temperature range of 15-45 degrees calculus, however the most rapid growth is at temperatures near that of body temperature. S. aureus is a nonmotile, nonsporeforming facultative anaerobe, which produces lactic acid upon fermentation of glucose. S. aureus is considered a potential pathogen. It can be found in humans in nasal passages and on skin and mucous membranes. S. aureus is a leading cause of soft tissue infections, and is a major cause of hospital acquired infections of surgical wounds and needle sticks. S. aureus also causes toxic shock syndrome (TSS), food poisoning, pneumonia, meningitis, and boils. Escherichia coli (Fig.6) is a common gram-negative, rod-shaped intestinal bacterium. It grows at about 37 degrees Celsius and is very viable in many environmental conditions such as changes in pH, chemicals, and temperature. It is a facultative anaerobe which can ferment acid and lactose. E. coli lives in a mutualistic relationship with humans and other warm blooded animals where it survives in the GI tract. It is the predominant facultative organism in the human GI tract. It is a useful bacterium for the analysis of water for fecal contamination. E. coli can cause gastroenteritis or urinary tract infections, and is a common cause of food poisoning. E. coli can be contracted through undercooked contaminated beef, drinking contaminated water or unpasteurized milk, and by person to person through hand to mouth contact. Bacterial Lawn Growth Zone of Inhibition(mm) Zone Of Inhibition 20.00 Iodine Hydrogen Peroxide 15.00 Nitrofurazone 10.00 5.00 Diameter in mm (clearance value) Fig.7. Bacterial Plates for Disk Diffusion EC plate with Hydrogen Peroxide 0.00 P. aeruginosa E. coli S. aureus Bacteria Used Test II. MBC test on pregrown bacteria cultures. Ten cultures of each bacteria SA, EC, and PA was prepared using 5ml of nutrient broth and three loops of bacteria. The cultures were then incubated at 37°C for 24hrs. Eight sterile Mueller Hinton Agar dishes were prepared using 20ml of agar per dish and allowed to cool. Three 24hr nutrient broth cultures of each bacteria tested was used per antiseptic. In the first culture 1ml of an antiseptic was used, in the second .5ml of the same antiseptic was used, and in the third .25ml of the antiseptic was used. This was repeated for the other two antiseptics being tested. One culture per bacteria was left as a control group. The samples were then reincubated for 24hrs at 37°C. After incubation of the test tubes the plates were split into quadrants and streaks of each test tube was done. The plates were then incubated for 24hrs at 37°C and the presence of growth was observed and noted. Graph 1. Average Zone of Inhibition (mm) after 24 hour incubation 1ml/5ml NA Cidal Growth Turbidity Pseudomonas aeruginosa Iodine E. coli Conclusion: Staphylococcus aureus Pseudomonas aeruginosa Hydrogen Peroxide E. coli Staphylococcus aureus Pseudomonas aeruginosa Test III. MIC and MBC tests Nitrofurazone For each bacteria, ten test tubes with 5ml of nutrient broth were inoculated with three loops of 24 hr. nutrient broth culture. Three of these inoculated tubes were used per antiseptic. In test tube 1, 1ml of antiseptic was added. In test tube 2, .5ml of antiseptic was added, and in test tube number 3, .25ml of antiseptic was added. This was repeated for each of the antiseptics. One sample of each bacteria was kept as a control. The antiseptic cultures were then incubated at 37°C for 24 hrs. After incubation samples were observed for turbidity. The samples that did not demonstrate turbidity were used for the MBC test. .05 ml/5ml NA Cidal E. coli Staphylococcus aureus Growth Turbidity Pseudomonas aeruginosa Iodine E. coli Staphylococcus aureus Pseudomonas aeruginosa Hydrogen Peroxide A streak plate was taken for each of the non-turbid bacterial samples. The streak plates were incubated for 24hrs at 37°C. After the 24hr incubation period the presence or absence of growth was noted and the data was analyzed. E. coli Staphylococcus aureus S. aureus Overall, the results support the hypothesis that iodine is the most effective bactericidal agent in the presence of moisture. This suggests that iodine is the best choice to use as an antiseptic for wounds. Hydrogen peroxide diffuses considerably and works fairly well in limiting the number of bacteria present, but does not have a high degree of bactericidal activity when water is present. Previous research suggests that while hydrogen peroxide makes a good cleaning agent, its bactericidal action is very weak. Nitrofurazone controls S. aureus (gram positive) quite well, but its effectiveness is diminished considerably in the gram negative bacteria tested. When testing the various antiseptics using the disk diffusion methods diffusibility issues were faced. Neosporan, which originally was an antimicrobial agent tested was completely unable to diffuse on the agar. Iodine also demonstrated less ability to diffuse in the Mueller-Hinton agar. Further experimentation using Nutrient Agar and possible several others would allow for analysis of the effects of Agar on the disk diffusion results. Pseudomonas aeruginosa Nitrofurazone E. coli Staphylococcus aureus P. aeruginosa Test III. MIC and MBC discussion (Table 2): In some respect the MIC and MBC test better simulated a cutaneous infection that an individual would experience after injury. The cells were allowed to cluster together, had free motion in a fluid medium, and concentrations of the antiseptic were diluted. The antiseptics were installed in a moisture rich environment that would imitate the interior of a wound with blood or pus. In PA and SA hydrogen peroxide demonstrated the least turbidity. When plating these cultures for the MBC test, growth developed in all three concentrations. This could be due to the lack of the ability to penetrate all cells in the medium, for example, cells that may “clump” together. This clumping process would decrease the surface area of the bacteria cell that is in contact with the antiseptic, therefore decreasing the antiseptics effectiveness. It could also be due to the antiseptics degradation in the presence of a high degree of water activity or in high moisture environments. Nitrofurazone’s MIC for SA was somewhere between 1ml and .5 ml. For PA and EC, nitrofurazone demonstrated very little effectiveness at any of the tested concentrations. Prior research demonstrated that nitrofurazone, although broadspectrum is effective primarily in gram-positive and facultative gram-negative bacteria (6). When testing the MBC for the 1ml concentration of nitrofurazone there was substantial growth present, this showed that although the concentration was high enough to substantially inhibit growth, it was not strong enough to demonstrate a complete kill of the sample. This could also be due to the “clumping” phenomena discussed previously. Iodine was the most effective bactericidal agent. It killed all of the bacteria (gram positive and gram negative alike) at concentrations of .5ml and 1ml. Growth was observed at .25ml of antiseptic. This demonstrates that the MBC for this agent is between .25ml and .5ml. E.coli 0.25 ml/5ml NA Cidal Growth Turbidity References 1. Pseudomonas aeruginosa Iodine Fig. 4. Scanning electron micrograph of the common soil bacteria Pseudomonas aeruginosa. Image © James A. Sullivan, CELLS alive! Fig.5. Scanning electron micrograph of Staphylococcus aureus http://www.bact.wisc.edu/Bact330/lecturestaph Iodine E. coli 2. Staphylococcus aureus Fig.6. Electron micrograph of E. coli cells http://www.slic2.wsu.edu:82/hurlbert/micro101/pag es/Chap2.html#two_bact_groups Staphylococcus aureus Hydrogen Peroxide Pseudomonas aeruginosa 3. E. coli 4. 5. Hydrogen Peroxide Pseudomonas aeruginosa Nitrofurazone Hypothesis: Iodine is used extensively as a antiseptic for surgeries, wound care, and sanitizing equipment. The bactericidal activity of iodine is very high and is not species specific (broad-spectrum). Previous research suggests that iodine tincture is the most effective bactericidal antiseptic tested. Hydrogen peroxide has very poor bactericidal qualities, and Nitrofurazone, although it has a longer half-life it does not have as large of an antimicrobial spectrum. E. coli 6. Staphylococcus aureus 7. 8. Table 2. MIC and MBC test results 9. Nirtofurazone 10. 11. Fig.8. Photo documentation. 12. Broga , Arthur . E. coLi and Their Human Environment. 1991. Woodrow Wilson Biology Institute. 18 Apr. 2004 <http://www.accessexcellence.org/AE/AEPC/WWC/1991/e.coli.html>. Escherichia coli. 2001. WVLC. 18 Apr. 2004 <http://wvlc.uwaterloo.ca/biology447/DistanceEd/assign2000/bates-yarkie/assig nment2.htm>. Hydrogen peroxide (PIM 946). Ed. DR. M. Ruse. Dec. 1997. INTOX meeting. 18 Apr. 2004 <http://www.inchem.org/documents/pims/chemical/pim946.htm>. Iodine Topical. 1998. WholeHealthMD. 18 Apr. 2004 <http://www.wholehealthmd.com/print/view/1,1560,DR_325,00.html>. Iodine (Topical). 22 Feb. 1994. Thomson MICROMEDEX. 18 Apr. 2004 <http://www.uspdqi.org/pubs/monographs/iodine-topical.pdf>. Kaiser, Christel, D. R. McCalla, and Antoon Reuvers. "Mode of Action of Nitrofurazone." Journal Of Bacteriology 104 (1970): 1126-1134. Stehulak, Nancy. Staphylococcus aureus: A Most Common Cause, HYG-5564-98. 18 Apr. 2004 <http://ohioline.osu.edu/hyg-fact/5000/5564.html>. Sullivan, James A. Pseudomonas_aeruginosa. http://www.cellsalive.com/cover3.htm, CELLS alive! 18 Apr. 2004 Todar, Kenneth. Pathogenic E. coli. 2002. UW-Madison. 18 Apr. 2004 <http://www.bact.wisc.edu/Bact330/lectureecoli>. Todar, Kenneth. Pseudomonas aeruginosa. 2002. University of Wisconsin-Madison Department of Bacteriology. 18 Apr. 2004 http://www.bact.wisc.edu/Bact330/lecturepseudomonas Todar, Kenneth. Staphylococcus. 2002. UW-Madison . 18 Apr. 2004 <http://www.bact.wisc.edu/Bact330/lecturestaph>. Woodward, Dr K. N. 775. Nitrofural (Nitrofurazone) (WHO Food Additives Series 31). 11 Nov. 1997. Veterinary Medicine Directorate. 18 Apr. 2004 <http://www.inchem.org/documents/jecfa/jecmono/v31je07.htm>.