Diapositiva 1 - EMDR et dissociations
advertisement

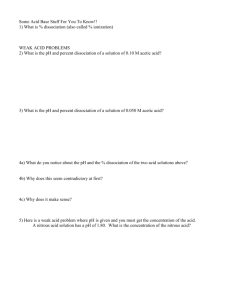
UNDERSTANDING THE RELATIONSHIP BETWEEN TRAUMA AND DISSOCIATION: The contribution of attachment theory and research Giovanni Liotti APC School of Psychotherapy Rome Conference “EMDR and Dissociation” Metz, November 17, 2015 DISORGANIZED ATTACHMENT (D.A.) PREDICTS DISSOCIATION • Two prospective studies support the hypothesis that infant D.A. predisposes to dissociative mental processes in later years (Ogawa et al., 1997; Dutra et al., 2009). • Infant D.A. is by far the more powerful predictor of dissociation with respect to reported later trauma (Dutra et al., 2009). • Dissociation may be rooted in human relatedness more than in purely intra-psychic dynamics (LyonsRuth, 2003). • A proper understanding of D.A. ( slide 3) is propaedeutic in trying to clarify the elusive concept of dissociation and its relation to trauma ( slide 4), e.g. through research on brain connectivity ( slides 5-10) DISORGANIZED ATTACHMENT • In the organized patterns of infant attachment (secure, avoidant and ambivalent) there is no conflict between the the care-seeking system and the survival defense system (freezing, fight-flight and feigned death), that are both activated during the exposure to traumatic events. • Abnormal tensions between the two psychobiological systems are caused by parental violently aggressive behavior that interrupts care-giving or by the helpless attitude of the caregiver in the face of the infant’s expression of fear and pain D.A. • The attachment system comes to involve expectations of danger whenever care-seeking needs are felt DISSOCIATION IS AN ELUSIVE CONCEPT • “Dissociation is an elusive concept, vague, confusing and controversial” (Dell, 2009, p. 225, in Dissociation and the dissociative disorders: DSM V and beyond). • Part of the difficulty in achieving a less confusing and controversial definition of dissociation might lie in the conceptualization of this psychological process as an intrapsychic consequence of psychological trauma. • A key aspect of the current conceptualizing of dissociation is that it is an intra-psychic defense against the mental pain of traumatic memories, disconnecting self-representations related to trauma from conscious processing and memory. • Although this assertion may seem surprising or absurd, there is no convincing statistical evidence that exposure to traumatic events, per se, adversely affects the memory of those events (Kihlstrom, 2005) THE ROLE OF ATTACHMENT PROCESSES IN DISSOCIATION • The finding that dissociation is predicted more by infant D.A. than by traumatic memories invites to explore the relational aspects of dissociation besides the intrapsychic ones related to defense against the mental pain caused by traumatic memories. • It is possible that dissociative processes take place in the brain of people with an history of D.A. mainly within the mental domain of human relatedness, and more precisely during or immediately after the activation of their attachment system. • This hypothesis can be empirically tested by exploring the mind-brain processes related to D.A. WHAT KINDS OF MIND-BRAIN PROCESSES ARE RELATED TO D.A.? • Dissociation involves deficits in cortical connectivity, that can be measured by the procedure called EEG coherence • If these deficits in cortical connectivity could be assessed in people with histories of D.A. immediately after the priming of mental states related to the attachment system, but not before such priming, we may achieve a better understanding of the roots of dissociation in human relatedness (and not only in an individual, intra-psychic, defense mechanism). • The administration of the AAI is believed to be an adequate way of priming the activation of the attachment system in adults. EEG COHERENCE: A REMINDER • EEG Coherence is a computerized measure of the linear synchronization between two signals recorded at different locations of the brain. It is a statistical measure of the average agreement in phase difference (weighted by amplitude) between two signals measured over time. It is specific for each EEG frequency band: α (alpha), β (beta), γ (gamma), δ (delta) and θ (theta). • It is considered a measure of the functional association between two brain regions (cortical connectivity). • Dissociation involves by definition a deficit in the degree of cortical connectivity. EXPLORATION OF CORTICAL CONNECTIVITY IN ATTACHMENT RELATED STATES OF MIND • A research team headed by Benedetto Farina and Anna Maria Speranza is studying cortical connectivity 3 minutes before and after the administration of the AAI in a group of patients with both cumulative (complex) childhood trauma and unresolved states of mind (Ulinked to infant D.A.). This patient group is compared with a control group of adult subjects whose AAI is coded in the “organized” categories (F, E, Ds linked to the organized patterns of infant attachment). • Preliminary results: the patient (U) sample shows a specific type of brain processing of information, suggesting dissociation, immediately after the administration of the AAI. Before the administration of the AAI, cortical connectivity was comparable in the patient and control samples. An EEG coherence study of complex PTSD basal EEG coherence 3 minutes before administering the AAI EEG coherence measured again 3 minutes after ending the AAI 3’ before Base EEG Relaxed wakefulness, closed eyes Skin conductance 3’ after Base EEG Relaxed wakefulness, closed eyes AAI Skin conductance Spectral analysis of EEG frequency (range: 1 – 127 Hz) Spectral analysis of EEG frequency (range: 1 – 127 Hz) EEG coherence EEG coherence Adult Attachment Interview - AAI * Standardized interview for evaluating the state of mind, the metacognitive monitoring and the narrative coherence related to autobiographical memories of past attachment experiences * Evokes memories of unresolved attachment trauma in people with DA Attachment Disorganization scoring: (1) 1. incoherence of discourse, memory and thought concerning attachment (2) 2. difficulties in emotion regulation (3) 3. poor metacognitive monitoring (impairment of the higher-order of integrative mental functions during the interview) EEG COHERENCE BEFORE AND AFTER THE AAI • There is no significant difference between baseline measures of EEG coherence before the AAI in the samples later classified U, F, E, and Ds. • This means that the presence of traumatic memories per se does not involve changes in baseline cortical connectivity. • However, after the administration of the AAI, there is a very significant increase of cortical connectivity in the “organized” sample (without differences among the F, E and Ds sub-samples) in three frequency bands (α, β, γ) of the EEG. No such increase is observable in the “disorganized” (U) sample. Comparison between cortical connectivity before and after the AAI [Farina B., Speranza AM et al (2013). Eur Arch Psychiatry Clin Neurosci] DISSOCIATION IS A FAILURE IN THE INTERSUBJECTIVE SHARING OF TRAUMATIC MEMORIES? • These preliminary findings suggest that mental states related to D.A. hinder, at the level of both inner and outer dialogue, the possibility of sharing with an attachment figure the experience of fright and pain linked to traumatic experiences, in the hope of being soothed. This is the relational base for the lack of the increase in cortical connectivity that normally follows the retrieval of personally highly significant early attachment experiences. • In turn, such a lack of the normally expected increase in cortical connectivity may be close to the essence of dissociation. Dissociation may be linked more to particular representations of self-with- other in attachment exchanges (forbidding the sharing of traumatic memories in the hope of being soothed) than to the need of avoiding mental pain. No pain is so severe that it cannot be soothed when it becomes a story to be told to a caring listener, states the Talmudic tradition. When one cannot expect to meet a really caring listener, and expect instead neglect, fear or aggression, the story cannot be constructed either in the mind or in the dialogue. This, rather than an intra-psychic defense against mental pain, is perhaps the essence of both post-traumatic dissociation and unresolved mental states related to attachment AN IMPLICATION FOR CLINICAL WORK • Dissociative and borderline patients may manifest dissociative symptoms and experiences within one or more psychotherapy session • The seeming antecedent is the narrative of a traumatic memory, but sometimes the immediate context is not related to such a narrative • It may be hypothesized that in both cases the manifestation of dissociation is explained by the activation of the patient’s (disorganized) attachment system during the interaction with the therapist (i.e., the patient feels the emotional closeness of the therapist • In order to avoid the deficit in self-reflection linked to dissociation, the therapist is advised to monitor signs of activation of the attachment system in the patient, and avoid that it becomes prolonged INDIRECT SUPPORT TO THIS HYPOTHESIS • … comes from the clinical wisdom on which the guidelines for the treatment of dissociative patients are based • Before attempting to work on the traumatic memories, these guidelines prescribe to construct a solid therapeutic alliance • The therapeutic alliance involves the prevailing activation of a behavioral-motivational system quite different from attachment, namely the egalitarian cooperative system (Cortina & Liotti, 2010; Liotti & Gilbert, 2011). • When the cooperative rather than the attachment system is active in the clinical exchange, the hindrance to the narrative of traumatic memories caused by D.A. is circumvented, so that trauma work and integration of previously dissociated representation of self-with-other can proceed. IMPLICATIONS FOR UNDERSTANDING THE MECHANISM OF ACTION OF EMDR • Besides the typical basic technique aimed at increasing cortical connectivity while priming traumatic memories, the clinical practice of EMDR seems to possess procedures that may minimize the likelihood of a protracted activation of the patient’s attachment system during the trauma work sessions. • This intrinsic attitude of looking for the “right emotional distance” – or the “right degree of emotional closeness” – in the clinical practice of EMDR is in keeping with what the research on the role of attachment disorganization in dissociative trauma-related disorders would suggest as an important therapeutic tool in the treatment of cPTSD. REFERENCES • Cortina, M. & Liotti, G. (2010). Attachment is about safety and protection. Intersubjectivity is about social understanding and sharing. Psychoanalytic Psychology, 27, 410-441. • Dutra, L., Bureau, J., Holmes, B., Lyubchik, A. & Lyons-Ruth, K. (2009). Quality of early care and childhood trauma: a prospective study of developmental pathways to dissociation. J. Nerv. & Ment. Dis., 197, 383– 390. • Kihlstrom, J.F. (2005). Dissociative Disorders. Annual Rev. Clin. Psychol., 1: 227-253. • Liotti, G. & Gilbert, P. (2011). Mentalizing, motivation and social mentalities: Theoretical considerations and implications for psychotherapy. Psychology and Psychotherapy: Theory, Research and Practice, 84: 9-25. • Lyons-Ruth, K. (2003). Dissociation and the parent-infant dialogue: A longitudinal perspective from attachment research. Journal of the American Psychoanalytic Association, 51, 183-213. • Ogawa, J.R., Sroufe, L.A., Weinfield, N.S., Carlson, E.A. & Egeland, B. (1997). Development and the fragmented self: Longitudinal study of dissociative symptomatology in a nonclinical sample. Development and Psychopathology, 9, 855-879.