Final Case Study - Cal State LA
advertisement

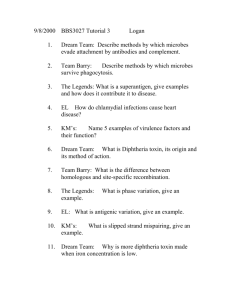
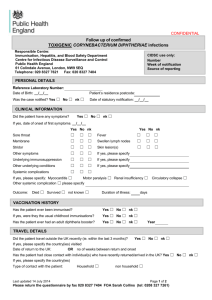
Case Study Pathogenic Bacteriology 2009 Case # 20 Luu, Helen Chiu, Allen Navarrete, Maria Case Summary A 2-year-old male child experienced upper respiratory infection. Anorexia and lethargy was seen. At the emergency room, he had a fever of 39.9°C. Physical examination showed a clear chest, exudative pharyngitis, and bilaterally enlarged cervical lymph nodes. Throat culture was taken and indicated no group A streptococci. Penicillin was given, but worsened and he became increasingly lethargic. He developed respiratory distress when admitted to the hospital. Examination revealed patient was febrile to 38.9°C and had an exudate in the posteriour pharynx that was yellowish, thick membrane which bled when scraped and removed. Patient’s medical history indicated no immunizations received. Key Information Pointing to Diagnosis Site of infection was the upper respiratory, pharynx. Symptoms were anorexia, drowsiness, mild fever, and respiratory distress. Examination showed exudate in posterior pharynx which bled when scraped. Figure 1 was a special isolation medium used to isolate the throat culture specimen. Figure 2 showed a Gram stain of the throat swab. No immunizations received. Diagnosis Pathogen causing infection : Corynebacterium diphtheriae C. diphtheriae is normal inhabitant of the nasopharynx that causes upper respiratory tract illness. Stages of infection in respiratory disease: Figure 1 shows black colonies on tellurite agar. Initial stage: sore throat, low-grade fever; followed by adherent pseudomembrane on the pharynx and tonsils. Later stage: localized damage, bleeding, difficulty in breathing, and mocarditis and peripheral neuritis. Tellurite selects and differentiate amongst Corynebacterium. Figure 2 shows small Gram-positive bacilli that are pleomorphic. Arrangement is palisade or Chinese letters. Figure 1 Figure 2 Classification,Gram Stain Results, and Microscopic Appearance of Corynebacterium diphtheriae Family: Corynebacteriaceae Genus: Corynebacterium Species: diphtheriae Small Gram-positive bacilli that are club-shaped. Arrangement = palisade or Chinese letters Classification based on colony morphology. Subspecies: C. diptheriae mitischodis : black colonies with a gray periphery C. diptheriae intermedius: large, gray colonies C. diptheriae gravis; small, dull gray to black All produce an immunologically identical toxin with gravis being associated with the most severe disease. Gravis grows faster and depletes the local iron supply which allows earlier and greater toxin production. Diagnosis/Isolation/Identification/ of Corynebacterium diphtheriae Gram stain showing gram-positive bacillus with arrangement of Chinese letters Loeffler’s agar slant: An enrichment medium that contains serum and egg to enhance the formation of metachromatic granules in C. diphtheriae. Stained with methylene blue for better visualization. Requires selective media containing tellurite to isolate the organism. Tellurite selects for Corynebacterium and other Gram-positive organisms and inhibits Gram-negative organisms Cystine tellurite: longer shelf life Tinsdale: differentiate amongst Corynebacterium; helps to distinguish other Corynebacterium species (diptheroids) that normally inhabit the nasopharynx. Colonies appear black or gray due to tellurite reduction. C. diphtheria would form brown halos around the colonies due to formation of ferric sulfide on tinsdale agar. Diagnosis/Isolation/Identification/ of Corynebacterium diphtheriae To prove that it can cause diphtheria, toxigenicity of C. diphtheriae strains is demonstrated. Most common in vitro assay is the Elek immunodiffusion test. -Based on double diffusion of diphtheria toxin and antitoxin in an agar medium. - Organism is streaked on the plate. Low concentration of iron is required in the medium which triggers toxin production. - A filter paper strip with diphtheria antitoxin is placed perpendicular to he streak of the organism. - Formation of a toxinantitoxin precipitin band at the zone of equivalence indicates production of diphtheria toxin. Diseases and Pathogenesis of Disease Caused by Corynebacterium diphtheriae Normally found in the throats of healthy carriers. Organism can cause: Diphtheria which starts as a local infection of the mucous membrane causing a membranous pharyngitis Cutaneous diphtheria which necrotic lesions with occasional formation of a local pseudomembrane occur. More common in tropical and subtropical areas. Toxigenic strains cause severe disease. Secretes a potent heat-labile polypeptide exotoxin that cause diphtheria. Exotoxin causes diphtheria, not the organism. In order for toxin production to occur: Bacterium must be lysogenized by a bacteriophage that carries the tox gene. Aerobic conditions, alkaline pH of 7.8-8.0, and a low iron level. Diseases and Pathogenesis of Disease Caused by Corynebacterium diphtheriae C. diphtheria toxin: Toxin binds to its cell surface receptor and enters through receptor mediated endocytosis. Acidification of endocytic vesicle allows A to dissociate from B. A enters the cytoplasm and catalyzes the transfer of ADP-ribose from NAD to the eukaryotic elongation factor-2. This results in inhibition of protein synthesis and cell death. Therapy, Prevention and Prognosis of Patient Infected with diphtheria For a patient infected with C. diphtheria, therapy treatment with antitoxin and antibiotics. Goal for both is to kill the organism and stop toxin production. Antitoxin is only effective before toxin enters the cell. The antitoxin neutralizes circulating (unbound) toxin that prevents progression of the disease. Sensitivity testing needs to be done prior to using antitoxin. Antibiotics such as penicillin, erythromycin to eliminate the organism. Usually given for 14 days. Individuals that recover from diphtheria may become asymptomatic carriers of the organism. Transmission is from person-to-person via respiratory droplets. Disease can keep spreading and become epidemic. Rarely from skin to skin contact. Historically, diphtheria has been a deadly disease mainly for children. Patients infected with diphtheria should be isolated for a couple of days to prevent other individuals catching this contagious disease. Therapy, Prevention and Prognosis of Patient Infected with diphtheria Prognosis depends on the size and location of the membrane. Early detection and treatment will eliminate the organism and toxin. The longer the delay, the higher the death rate. If untreated, it is fatal due to airway obstruction, kidney and heart problems. Vaccination Childhood vaccination with diphtheria/pertussis/tetanus (DPT). Primary 3 doses given within half a year with another dose given later more than a year after that. Tetanus-diphtheria toxoid (Td) is also available and recommended as a booster every 10 years. Due to waning antitoxin titers, most individuals have antitoxin levels below the optimal level 10 years after the last dose. Schick SkinTest: Used to test for an individual’s immunity to diphtheria toxin. Done by injecting a small amount of diphtheria toxin intradermally Observance for a local erythematous and necrotic reaction. An erythematous reaction with or without necrosis indicates that there is no antitoxin antiboides to neutralize the toxin and therefore, the individual is susceptible to diphtheria. Primary Research Article Van Damme, P., Burgess, M., 2004. “Immunogenicity of a combined diphtheriatetanus-acellular pertussis vaccine in adults.” Vaccine. 22. 305-308 Two clinical studies were set-up (1 in Belgium and 1 in Australia) to evaluate the immunogenicity of a booster vaccination, using either a dTpa vacine (Boostrix) or a licensed bivalent tetanus and diphtheria (Td) vaccine. METHODS: Randomly, chose 824 people that are over 18 years of age to receive either one dose of Boostrix or a licensed bivalent Td vaccine. No history of diphtheria or tetanus vaccination. No previous exposure to disease, for at least 5 years. Two blood samples, 1 prior to the vaccination and 1 one month after vaccination, were taken to evaluate the serostatus and imunnogenicity of the adults. Used ELISA test to measure antibody concentrations for diptheria, tetanus, and pertussis. Seroprotection for each antibody concentration were as followed: Anti-diphtheria antibody concentrations > 0.1 IU/mL Anti-tetanus antibody concentrations > 0.1 IU/mL Cutt off for pertussis was 5 E1.u/mL Primary Research Article RESULTS: From the blood sample collected prior to vaccination, about a quarter or more of the test subjects were seronegative for antibodies against diphtheria, tetanus, and pertussis. From the blood sample collected 1 month post-vaccination, almost all individuals had seroprotection for both diphtheria and tetanus. Individuals vaccinated with Boostrix were also seropositive for the pertussis antigens PT, FHA, and PRN. Primary Research Article CONCLUSIONS: Even with childhood vaccination programs available in these countries, this shows that a portion of the adults in both Belgium and Australia is seronegative for antibodies against diphtheria and tetanus antitoxin. After one vaccination, individuals had antibody concentrations for the diseases that were above seroprotection limits. Despite the recommendation of getting vaccinated for the infectious diseases, this study comes to show that many individuals are either not up-to-date with getting a booster shot or have never been vaccinated before. Individuals are susceptible to the diseases and can become an epidemic problem once again. Vaccination for DPT wears off over time and in order to prevent the spread of this infection or get infected, booster shots must be taken at least every 10 years. Take Home Messages Disease includes diphtheria that starts as a local infection of the mucous membrane involving an exotoxin. High yields of toxin are synthesized only by lysogenic bacteria under iron deficiency conditions. Cutaneous diphtheria also seen but mainly in tropical areas. Typical symptoms are symptom low-grade fever, malaise, inflammation, edema, and exudate pharyngitis. Pathogen is the diphtheria toxin that the organism produces which can disseminate in the bloodstream and lymph nodes. Diagnostics include looking at site of infection, followed with culture swab to perform Gram stain, isolation on selective agar containing tellurite, and followed with in vitro or in vivo tests (ie. ELEK plate) to show presence of toxigenicity. Therapy is based on sensitivity testings followed by treatment with antitoxin and antibiotics. Prognosis depends on the size and location of the membrane. Early detection and treatment is crucial. Delayed treatment or no treatment can lead to more severe, fatal infections and even death. Prevention is DPT vaccination followed with a booster Td vaccine every 10 years. Transmission is spread by respiratory droplets from person-to-person. Threat is severe in children, unimmunized individuals, low levels of immunity individuals and frequent travelers. References "Diphtheria (Corynebacterium diphtheriae)." Menopause and all about Health and Beauty. 01 Mar. 2009 <http://www.drlera.com/bacterial_diseases/diphtheria_.htm>. "Disease Listing, Diphtheria, Technical Information | CDC Bacterial, Mycotic Diseases." Centers for Disease Control and Prevention. 06 Oct. 2005. 09 Mar. 2009 <http://www.cdc.gov/NCIDOD/DBMD/DISEASEINFO/diptheria_t.htm>. Efstratiou, Androulla, et.al. "Current Approaches to the Laboratory Diagnosis of Diphtheria." The Journal of Infectious Diseases 181 (2000): S138-145. Frassetto, Lynda A. "Corynebacterium Infections: Overview - eMedicine Infectious Diseases." EMedicine The Continually Updated Clinical Reference. 30 June 2008. 09 Mar. 2009 <http://emedicine.medscape.com/article/215100-overview>. Leboffe, Michael J., and Burton E. Pierce. A Photographic Atlas for the Microbiology Laboratory. 3rd ed. Englewood: Morton Company, 2004. Mahon, Connie R., George Manuselis, and Donald C. Lehman. Textbook of Diagnostic Microbiology. 3rd ed. Philadelphia: Saunders, 2006. Mattos-Guaraldi, Ana Luiza, et. al. "Diphtheria Remains a Threat to Health in the Developing World - an Overview." Mems Inst Oswalda Cruz 98 (2003): 987-93. McQueen, Nancy. “Corynebacterium,” 2009. Todar, Kenneth. "Corynebacterium diphtheriae and Diphtheria." Online Textbook of Bacteriology. 2008. 09 Mar. 2009 <http://www.textbookofbacteriology.net/diphtheria.html>. Van Damme, Pierre, and Margaret Burgess. "Immunogenicity of a combined diphtheria-tetanusacellular pertussis vaccine in adults." Vaccine 22 (2004): 205-308.