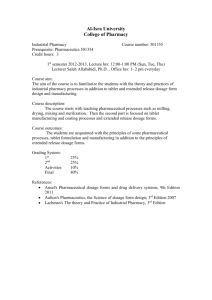
Course – IV Analysis of pharmaceuticals Introduction Drug laws and
advertisement
Course – IV Analysis of pharmaceuticals 1. Introduction Drug laws and schedules, drug and cosmetics act govt. analyst, drug inspector, requirement for approval of quality control laboratories, Administrative bodies for analytical purpose, introduction of new drug summary of different phases of test and approval. 2. Impurities Introduction to pharmacopoeias and monographs, source and type of impurities, tests for purity, limits of impurities, factors considered for fixing, limits and limit tests, limit tests for chloride, sulphate, heavy metal, arsenic, iron and lead. 3. Quantitative assay Indian pharmacopoeial assay, principles of assays of following drugs: Aspirin, Trimethoprim, Aminophylline, Calcium gluconate, hydrogen peroxide, Ascorbic asid, Ferrous sulphate, Thiamine hydrochloride, ciprofloxacir, Insuline. 4. Quality control of dosage forms Brief introduction to dosage forms and their classification, quality control, standards for various dosage forms i.e. Tablet, capsule, parenterals, Injections, powder, Ointments, Creams, Solutions, suspension, Emulsions, Test for sterility, microbiological assay of antibiotics and vitamins, Microbial limit tests, quality control of glass, Plastic, Rubber, containers and closures. 5. Quality control Consept of pharma. Q.C. , In process quality control, statistical quality control. 6. Stability studies. Introduction, pathways of degradation, detection of degradation products, calculation of shelf life, I.C.H. Guidelines on stability studies. Introduction Drugs and cosmetics act 1940 Drugs and cosmetics act was passed in 1940 (10 April), with the main object to regulate import, Manufacture, distribution, and sale (IMDS) of drugs and cosmetics. The act regulates import of drugs into India so that no standard or spurious drugs will be find its way in the country. The act regulates the manufacturing activity by making provisions and rules which provides control over manufacture of spurious or substandard …………………… in the country. The act also provides for the control over manufacture sale and distribution of Ayurcedic, siddha, Unani and Homeopathic drugs. In last few years, cosmetics are widely used in the country and it is necessary to control there quality act therefore, amended to make certain provisions related to cosmetics which regulates its import, manufacture, sale and distribution. The import of certain drugs and cosmetics permitted under licens. All classes of drugs and cosmetics imported into india shall comply with prescribed standards and shall labelled in prescribed manner. The manufacture of all classes of drugs require prior license by licensing authority andlicense also required for sale of allopathic and homeopathic drugs. Each state require to appoint licensing authority to issue or grant licenses for manufacture or sale of drugs and cosmetics control over manufacture and sale exercised by drug inspectors is required. Drug control laboratory instate or central drug laboratory of state provided for analysis of drugs and cosmetics. Drugs and cosmetics provided for condition of licenses of manufacture, sale, distribution of drugs and cosmetics in prescribed manner of labelling and packaging of drugs and cosmetics. All drugs manufactured shall be labelled and packed in a prescribed manner. The act also provide for the establishment of DTAB (Drug technical advisory board) to advice government on technical matter arising out of the administration of act and DCC (Drug consultative committee ) to advice to board and government to secure uniformalality in the administration of the act through out India. Drugs Drug includes All medicines for internal or external use in human being or animals and all substances intended to be use for or in diagnosis, treatment, mitigation or prevention of any disease or disorder in human beings or animals including preparations applied on human body for the purpose of repelling insects like mosquitoes. Such sub. Other than food intended to affect the structure or any functions of human body or intended to be used for destruction of insects with cause disease in human beings or animals. All sub. Intended for use as component of drugs including empty gelatin capsule. Such devices intended for internal or external use in the diagnosis, treatment, prevention of disease or disorder in human being or animals. Ayurvedic, Siddha, Unani Drugs It includes all medicines intended for internal or external use for or in the diagnosis, treatment, mitigation or prevention of disease or disorder in human being or animal and manufactured in accordance with formal described with authorative books of Ayuredic, siddha or unani system of medicine specified in first schedule. Misbranded drugs A drug shall be deemed to be misbranded if: i) ii) iii) It is so coloured, coated, powdered or polished that damage is concealed or if it is made to appear of better or greater therapeutic value than it really is. It is not labelled in a specific prescribed manner. Its label or container or anything accompanying the drugs bear any statement, design or device which make any false claim for the drugs or which is false or misleading in any particular. Adulterated drugs A drug shall be deemed adulterated if: i) ii) iii) iv) v) vi) It consists in whole or in part of any filthy, putrid or decomposed substances. It has been prepared, packed or stored under insanitary condition where byit may have been rendered injurious to health. It’s container composed in whole or in part of any poisonous or deleterious sub. which may render the contents injurious to health. It bears or contain a colour other than prescribed which may use for the purpose of coloring only. It contains any harmful or toxic sub. Which may rendr it injurious to health. Any sub. mixed with it so as to render its quality or strength. Spurious drugs Spurious drug means a drug: i) ii) iii) iv) Imported under a name which belong to another drug. Which is imitation of or is a substitute for another drug or resembles to another drug in a manner to device or bear upon its label or container. The name of the another drug unless planely or conspicuously marked so as to revel its true character and it’s lack of identity with such other drugs. The label or container of which the bears the name of an individual or company perforating to be manufacture of drug which individual or company is fictious or does not exist. Which perforates to be the product of manufacturer of whom it is not truly a product. new drugs i) ii) iii) A new substance of chemical, biological or biotechnological origin in bulk prepared dosage form used for prevention, diagnosis or treatment in man or animals which accept during local clinical triles has not been used in the country for any significant extent and which accept during local clinical triles has not been recognized in the country as effective and safe for purposed claimes. A drugs already approvided by licensing authority for certain claims which is now proposed to be marketed with modified or new claims via indication, dosega, dosage form ( including sustain releases dosage form ) and route of administration. A fixed dose combination of two or more drugs individually approved earlier for certain claims which are now proposed to be combined for the first time in a ratio or if the ratio of ingredient In an already marketed combination is proposed to be changed with certain claims i.e. does dosage form and route of administration. (A new drug shall continue to be as new drug for period of four years from the date of its first approval or its inclusion in Indian pharmacopeia which is ever is earlier. Cosmetics RPSSIA – CBPAA It means any article intended to be rubbed, poured, or sprayed on or introduced into or applied to any part of the human body for the cleansin, beautifying, promoting attractiveness, or altering the appearance and includes any article intended for use as component of cosmetics. Misbranded cosmetics A cosmetic shall be deemed to be misbranded if; i) ii) iii) It contains a colour which is not prescribed. It is not labelled in a prescribed manner. The label of container or anythings accompanying the cosmetics make any false or misleading claims. Spurious cosmetics A cosmetic shall be deemed to spurious of; i) ii) iii) iv) Schedules It is imported under a name which belong to another cosmetic. It is an immetation of or is a substitute for another cosmetic or resembles another cosmetic in a manner likely to be look or recives like to be or its label or container. The name of the another cosmetics unless it is plainly or conspicuously marked so as to revel it’s true character and its lack of identity with such other cosmetics. The label or container bears the name of an individual or a company purpowhich is rating to be manufacturer of cosmetics which is fictitious or does not exists. It purporates to be the product of manufacturer of whom it is not truly a product. There are two schedules to the act and twenty seven schedule to the rule. a) Schedules to the act 1) First schedule List of Ayuredic, siddha, Unani books. Ayurvedic – Arogaya, Kalpadrum, Arka Prakashan, Astang. Siddha – Nagmuni, yugi, Karisal. Unani- Karbdin, Quadri, Karbdin Azim, Karbdin Azim, Karbden kabir. 2) Second schedule Standards to be complied with imported drugs and by drugs manufactured for sale, sold, stocked or exhibited for sale or distribution. b) Schedules to the rules 1) Schedule A List of forms used for making application for issuing licenses, granting licenses, sending memorandms, etc. 2) Schedule B Fees for test or analysis by the central drug laboratory or by government analyst. 3) Schedule C Other special product (not to be administered parentally) e.g. drugs belong to digitalis group, irgote, liver extract, first liver oils harmones and preparation containing harmones vaccines vaccines. 4) Schedule C Biological and special products. e.g. sera, so in of serum proteins intended for injection, vaccins for parenteral injections, insulin, antigerms, antitoxins, antibiotics and preparation in the form administered parentraly sterilized syrgical ligetures and sutures ophthalmic preparation. 5) Schedule D Class of exempted drugs which are exempted from certain provisions applicable for import of drugs. 6) Schedule E List of poisonous substance. 7) Schedule F Provisions applicable to vaccines, toxins, antigerms, sera and functioning and operation of blood banks and for preparation of blood products. 8) Schedule FI Provisions applicable to other biological and special product such as vaccines, antigens, tubesulin, etc… regarding there production, testing, storage and packaging etc… 9) Schedule FII Standards for syrgical dressing. For stanardisation following methods are used: i) ii) iii) iv) v) vi) Detect in frabrin Measurement in length and width. Wt. per unit area. Foreign matter Fluore scence Packing labelling storage 10) Schedule FIII Standards for umbilical tapes. 11) Schedule FF Standards for ophthalmic pxeparations. 12) Schedule G Drugs to be given under administration supervision of R.M.P (Registered, medical) e.g. aminoptrine, insulin, phiniramine, syclophosphamid The drugs to be labelled with the word “coution” it is dangerous to take this preparation except under medical supervision. 13) Schedule H Prescription drugs which are required to be sold by prescription of registered medical practitioner (RMP). 14) Schedule J List of diseases and oilments which a drug may not claim to prevent. E.g. blindness, opendisited, lepracy, obesity, aids, cancer, tumours, ditetix, glaucorna, senual, impotensy. 15) Schedule M Good manufacturing practices and requirement of factory plants, premises, etc. for manufacture of drugs. 16) Schedule MI Requirement of factory primices, plants, etc. for manufacture of homeopathic drugs. 17) Schedule MII Requirement of factory primices, plant, equipment, etc. manufacture of cosmetics. 18) Schedule MIII Requirement of factory primices for manufacture of medical devices. 19) Schedule N List of minimum equipment for efficient running of pharmacy. 20) Schedule O Standards for disinfectant fluid. 21) Schedule P Life period of drugs. e.g. Ampiciline (30months in cool places). Cephalexin (24 months), Cobravenum in soln (3 months at 2O C – 5OC, protecte from light), robbege vaccine (3 month at 4O C). 22) Schedule PI Pack sizes of drugs. e.g. Albendazole suspention – 10 ml , vit. A oral drops -7.5 ml projesteron (oral contraseptives tablet), 21 or 22 with or without 7 placebo. 23) Schedule Q List of coaltar colours permitted to be used in cosmetics and list of colours permitted to be used in soaps. 24) Schedule R Standards for condoms made up of rubber latex intended for single use. 25) Schedule S Standards for cosmetics. 26) Schedule T Requirement for factory primices and hygienic conditions for manufacture of Ayurvedic, siddha and Unani drugs. 27) Schedule U Particulars to be shown in manufacturing and analytical records of drug. 28) Schedule UI particulars to be shown in manufacturing records of cosmetics. 29) Schedule V Standards for patent and propntary medicines and for patent and property medicines containing vitamins. 30) Schedule W List of drugs which shall be marked under genetic name only. 31) Schedule X List of habit forming psychoptropic and other drugs. e.g. amphetamine phenobarbital. 32) Schedule Y Requirements and quite lines on clinical style for import and manufacture of new drugs. Administrative Bodies The central government and state government establish or appoint following bodies for efficient running of the act. A) Advisary 1) Drug technical advisory board (DTAB) 2) Drug consultative commity (DCC) B) Aralytical 1) Central drug laboratory (CDL) 2) Government Analyst 3) Drug control lab. In state C) Executive Bodies 1) Licensing authority 2) Drug inspector 3) Customs collector Drug technical Advisory Board (DTAB) Under the provision of the section 5 of the act, central government appoint DTAB to advise central government and state government on technical matter arising out of the administration of this act and to carryout the other functions assigned to it by this act. Drug consultative commity (DCC) this is an advisory commity constituted by central government to advice the central and state government and DTAB on any matter to secure uniformly throughout India in the administrative of the act. Constitutions 1) Two representatives of central govt. nominated by central govt. 2) One representative of each state govt. nominated by government. Central drug laboratory (CDL) The central government established CDL (Kolkatta) under the control of director. Functions 1) To analyse all test, saples of drugs or cosmetics sent to it by a) Customs collector or any authorized officers b) Courts 2) To carry out such other duties as may be entrusted to it by the central government or by the state government with the permission of the central government, after consultation with DTAB. 3) A) in case of the following drugs are classes of drugs, functions of CDL are carried out at central research institute (CRI) casuali and such functions are exercised by direction of said institute. i) Sera ii) Vaccines iii) Toxins iv) Antigens v) Antibodies vi) Solution of serum proteins vii) Antitoxins viii) Bacteriophages The functions regarding oral polio vaccine are exercised by deputi director and head of the polio vaccinetsting laboratory of CRI. B) in case of following drugs or classes of drugs functions of CDL are carried out at IVRT (Izatnagar or Multeshwar) auch functions are exercised by director of either institutes. i. ii. iii. iv. C) Antisera Vaccines Toxiodes Diagnostic antigens for veterinary use In case of condoms the functions of CDL are carried out at central India pharmacopeial lab. (Ghazlabad). Suchfunctions are exercised by director of said lab. D) In case of VDRL antigen the functions of CDL are carried out at laboratory of serologist and chemical examiner to the govt. of India (Kolkatta) and such functions are exercised by serologist and chemical examiner of said lab. E) In respect of IUD- Intra Uterine device and feloperings the functions of lab shall be carried out at department of biological engineering, ILT new Delhi and such functions shall be exercised by head of the said department. Government Analyst State govt. by notifying in the official Gazette appoint the govt. analyst under sub. Section of section 20 of the act for the analysis and testing of samples of drugs and cosmetics in the drug control lab. Central covt. May also appoint govt. analyst for specified categories of the drugs or cosmetics under sub. Section 20 of the act. A person to be appointed at the govt. analyst should have no financial interest in the import, manufacture or sale of drugs or cosmetics. Govt. analyst for Ayurvedic, siddha and Unani drugs is appointed by state and central govt. under section 33 G of act. Qualifications A person appointed as Govt. Analyst should have following qualifications. i) ii) iii) Graduate in medicine or science or pharmacy or pharmaceutical chemistry of recognized university with not less than (NLT) 5 years post graduate experience testing of drugs. Post graduate degree in medicines, science or pharmacy or pharmaceutical chemistry of recognized university with NLT 3 years experience in testing of drugs. Associateship diploma of institution of chemistry ( India) with “Analysis of drugs or pharmaceuticals as one of the subject”. And with not NLT 3 years experience in the testing of drugs in a lab under central of 1) Govt. analyst 2) Head of an institution or testing laboratory approved for the purpose by the appointing authority. Provided thata) For the purpose of testing of drugs specified in schedule C, A person to be appointed should produce evidence or satisfactory training in physiology, bacteriology, serology or pathology or pharmacology or microbiology and should have said experience. b) Person to be appointed as govt. analyst should not engage directly or indirectly in trade or business connected with manufacture of drugs. c) For the purpose of examination of veterinary, biological product. The person appointed as govt. analyst should be graduate in veterinary science or general science or medicine or pharmacy with NLT 5 years experience in standardization of biological products or person having post graduate degree in above faculties with NLT 3 years experience. d) The person already appointed as govt. analyst may continue to remain in service if the appointing authority so designed even though he or she does not fulfill said qualification. Duties I) To analyze or tests samples of drugs or cosmetics sent to him by drug inspector or other person and to hrnish the report of the result of such analyst or test. II) To forward to the govt. the report of analytical and research work with a view to their publication at the disuretion of the govt. Procedure on receipt of sample On receipt of package of sample from drug inspector, govt. analyst compares the seal on the package with the speciment impression of the seal received separately and notice conditions of seals on the packet. On completion of test or analyst he supplies to the inspector a report of the analysis in triplicate in form number 13, together with full protocols of the test applied. If purchaser want to analyse or test drugs or analysis in form no.14, a accomained with a presented fees and reports of test or analysis of such drugs or cosmetics is to be supplied to be in form no.14-B. Drug inspector Central govt. or state govt. by notification in official gazzet appointes inspectors having prescribed qualification under section 21 of the act for the specified area. A person to be appointed as drug inspector should have no finantial interest in the import manufacture or sale of drugs or cosmetics. Drug inspector is public servent under section-21 IPC (India Pinal Code). In relation to the Ayurvedic, siddha or Unani druga an inspector appointed by state or central govt. under section 33-F. Qualification A person to be appointed as drug inspector have following qualification. Graduate in pharmacy or pharmaceutical sclence or medicine with specialization in clinical pharmacology or microbiology from recognized university. Provided that for the purpose of inspection of manufacture of sub. Specified in schedule C. a person appointed as drug inspector should have folloing qualification. I) II) III) NLT 18 months experience in mfg. of at least one of sub. Specified in schedule C. NLT 18 months experience in testing of at least one of sub. Specified in schedule C in a approved laboratory. NLT-3 years experience in inspection of organization (brms) mfg. any of the sub. Specified in schedule C. During the coarse of these service as a drug inspector. Powers of inspectors. An inspector may: a) Inspect; i) Any premises where in any drug or cosmetic is being mfg and the means employed for standardizing and testing the drug or cosmetic. ii) Amy premises where in any drug or cosmetic is being sold, stocked or distributed. b) Take samples of any drug or cosmetic i) Which is being mfg or being sold or stocked or distributed ii) From any person who is in the course of conveying, delivering or preparing to deliver such drugs or cosmetic to a purchaser. c) At all reasonable times, with such assistance, if any as he considers necessary i) Search any person, who has secreted about his person any drug or cosmetic in respect of which an oftence has been or is being committed or ii) Enter and search any place in which he has reason to believe that an offence has been or is being commited. iii) Stop and search any vehicle, vessel or other conveyance is being used for carrying any drug or cosmetic in respect of which an oftence has been or is being commited. d) Examine any record register, document or any other material object found and size the same if he has reason to believe that it may furnish evidence of commission of an offence. e) Require any person to produce any record, register or other document. Duties I) II) Duties of inspectors of premises licensed for sale i) To inspect not less than twice in a year all permises licensed for sale of drugs within the area assigned to him. ii) To satisfy himself that the conditions of the licences are being observed. iii) To procure and send for test or analysis imported packages which he has reason to suspect (doubt) contain drugs being sold in contravention of the provisions of the act. iv) To investigate any compliant in writing which may be made to him. v) To institute prosecutions in respect to breaches of act and mles. vi) To maintain a record of all inspections made and action taken by him including the taking of samples and seizure of stocks and to submit copies of such record to controlling authority. vii) To make such inquires and inspections to detect the sale of drugs in contravention of the act. viii) When so authorized by state govt. to detain import of packages which he has reason to suspect contain drugs, the import of which is prohibited. Duties of inspectors in relation to mfg of drugs i) To inspect NLT twice a year, all permises licensed for mfg of drugs and to satisfyhimself that the conditions of the license are being observed. ii) In case of establishments licenced to mfg products specified in schedules C and C1 to inspect; a) The plant and the process of mfg. b) The means employed for standardizing and listing the drug. c) The methods and place of storage. d) The technical qualification of the stuff employed. e) All details of location, construction and administration of the establishment likely to affect the potency and purity of product. iii) iv) v) To send forth with to the controlling authority at the each inspection a detailed report indicating the conditions of licence being observed and conditions which are not being observed To take samples of drugs mfg on the premises and send them for test or analysis. To institute prosecution in respect of breaches of the act and rules. Impurities Pharmacopoeia The word pharmacopeia is derived from the Greek words pharmacon- drug or medicine,poieo to make. Pharmacopeia is the standard book published by recognized authority containing with all information regarding particular drug (storage conditions, molecular wt., B.P., M.P. adverse effect, limits for the impurities like S, Cl, As,So42The term pharmacopeia was first used in 1580 in book on drug std. printed in Bergamo, Italy. After that number of national pharmacopoeia published by various European pharmacopoeias (EP), London pharmacopoeias (LP). Indian pharmacopoeia have been published, one each in 1955, 1985 and 1996. There were also four addendums in 1960,1975,1990,1992. Pharmacopoeias are published to have uniformity in the composition, purity and potency of medical sub. To avoid confusion. When newly discovered drugs, have been proved of sufficient value, they may be included in new edition of pharmacopoeia as supplement sub. Which are proved to be undesirable are removed from pharmacopoeia The first international pharmacopoeia was published by WHO (World Health Organization volume I) and in 1955 volume II. The object of this was to provide uniform in which world avoid the confusion caused by different national standards, strength and names. History of Indian Pharmacopoeias The govt. of Indian, through its letter number 2338 H©/43 dated 26th Jan. 1944, directed the drug technical advisory board to list the drugs used in Indi, which are not mentioned in British pharmacopoeia and also a standard to be proscribed to maintain uniformality and chemical test to be used to established identily and purity. The govt. of India published the first list of I.P. in 1946 at supplement to British pharmacopoeia. The IP. List contain about 180 monograph and number of appendecis prepared on the line on B.P. The first edition of I.I. complied and published in 1955. The supplement was published to the first edition in 1960. The monographs, appendix and general notes as prepared by working group and finally by the committee. Where that published in form of the third edition of pharmacopoeia of India in 1985 by the govt. of India. The govt. of India, ministry of health and welfare dated 12th Aug 1991 reconstituted the I.P committee for period of 5 years for preparation of fourth edith of I.P. in 1996 by thr govt. of India and recent edition was published in the form of 5th edition in 2007 by the govt. of India. The list of pharmacopoeia and some of the std. reference books of common use in India are; i) ii) iii) iv) v) vi) vii) India pharmacopoeia (I.P.) British pharmacopoeia (B.P.) (USP) united state pharmacopoeia European pharmacopoeia (E.P.) International pharmacopoeia (I.P.) Mercqindx. Indian pharmacentical codex (I.P.C.) Monograph A drug or compound included in the latest edition of pharmacopoeia is said to be official substance in the country of pharmacopoeia and the section dealing with official drugs in detail is known as monograph. It gives a detail systematic account of the drug. The monograph may give some or all of the following details of an official compound. 1) Titles: This is the approved name of the drug or its preparation. When the chemical composition of the sub. is known, molecular formulae and molecular wt. are given chemical names have been provided in monograph. These are the name sanctioned and employed by IUPAC. 2) Description: description in relation to the chemical is relative general in nature. This gives a physical description of sub. like crystalline or amorphous nature, colour, odour taste, etc. 3) Identification: Tests for identity are provided only as an aid to identification. These are usually based on qualitative tests for identifying the sub. colour reactions, precipitating tests, gas evolution are commonly employed for identification. 4) Minimum standards of purity : The limits are expressed numerically, he upper and lower limits of purity so that its range consists of two values themselves and intermediate values but no values outside the limits. The limit stated in pharmacopoeia are based on data obtained in normal analytical practice. 5) Dosage: dosage mentioned in the monograph are intended for general guidance. Generally, if not stated, the average range of quantities which are regarded as substance for adults when administration are given. Usual strength may be given for pharmaceutical dosage forms which is most commonly marked dosage strength. 6) Solubility: the statement on solubility are not std. or test for purity but are provided primarily as information. When the quantitative solubility test is given under stds, the 7) 8) 9) 10) 11) 12) drug should comply with all these requirements. Statements of solubilities are indicated by a descriptive phrase and are intended to apply at 20 to 30O. Approx. solvent volume in ml for 1 gm of solute. I) Very soluble less than 1. II) Freely soluble from 1 to 10. III) Soluble from 10 to 30. IV) Sparingly soluble from 30 to 100. V) Slightly soluble from 100 to 1000. VI) Very slightly soluble from 1000 to 10000. Storage: the sub. and preparations are to be stored under the conditions that prevent contamination and as for as possible, to avoid deterioration. Precautions that should be taken in relation to the effects of the atmosphere, moisture, heat and light are indicated. Specific directions are given with respect to temp. the conditions are defined as; Cold – Betn 2O and 8O. Cool – Betn 8O and 25O. Warm – Betn 30O and 40O. Excessive heat – any temp. above 40O. Containers: It is the devise that holds the chemical. The container should not interact physically or chemically with the chemical placed in it so as to alter the strength, quality or purity of the chemical beyond the official requirement. Container can be light resistant container, well closed container, tightly closed container, hermitically sealed container depending upon the chemical to be packed in it. Labelling: In general , labelling of drugs and pharmaceuticals is governed by drugs and cosmetics act. In certain cases, additional information which must be started on the label is mentioned in the monograph. Limit of impurities: limit tests are important to determine the permissive limits of tolerance. These tests are designed to identify and control small quantity of impurity. They usually involve simple comparison opale scence, colour or turbidity with that of standard prescribed in pharmacopoeia. By this test, we can find whether an impurity is within a specified limit or not. Physically constants: physically constants are the ch acteristics properties useful for identification and maintain nce of stds of purity and hence they are included in monograph. These constants include M.P., B.P., refractive index, optical rotation, light absorption, viscosity, particle size, polymorphism, etc. mentioned in pharmacopoeia for standardization of pharmaceuticals. Quantitative assays: The assays and tests are the standards prescribed by pharmacopoeias. The analyst is not precluded from employing an alternate method if he is satisfied that the method which he uses will give the same results. But in the event of doupt or dispute, pharmacopoeial methods are considered to be final. The procedures of assays are applied to the analysis of materials used in paharmaceuticals. There are various methods of qualitative analysis such as: 1) Chemical methods, volumetric, Gravimetric, Gasometric. 2) Instrumental methods. 3) Microbiological methods. 4) Biological methods. 13) Category: It represents an application of the test known pharmacological action of the article or of its active constituent. In case of pharmaceutical aids it may indicate the more common usage of the article. The statement is not intended to limit in any way the choice or use of the article not to indicate that it has no other activity or use. Quality control A quality of product is same of all its properties and characteristics relating to its efficiency, safely, acceptability for meeting a specific therapeutic response. Quality control is a day to day process of controlling the quality of incoming raw material including packaging material and containing through out the production and packaging operation, testing of finish product, documentation up to distribution. In short a planed system activities constituent followed to pure quality product in the market is quality control. Importance 1) Q.C. of department of pharmaceutical company assure purity and safety of medicine and thus protect the public health. 2) Q.C. helps for preparing new drugs application setting up of standards of drugs. 3) It enable the machines setting adjustment and modification of process and machinery. 4) It helps to keep up the quality of product during manufacture. 5) It also AIDS in locating and identifying the process results and detects product and helps control to the control scrap and cirplus. 6) It helps continuous production of quality product and better utilization of labour and material. 7) It also give idea to louer constituent of product by maintaining its quality. 8) Control quality in addition also provide and improved technically know how the product development. Impurities Definition Impurity is undesirable foreign material which may be toxic or may not be toxic present in pharmaceutical sub. Impurity is the sub. or the matter which does not form a part of medicinal or pharmaceutical sub. or drugs. Chemical purity emplies feedom from drug impurity but a state of absolute purity is not obtainable. Source 1) Raw material used in the manufacture traces of raw material may come in the final product. e.g. i) Source of some sodium compounds in NaCl. So trace of chloride may be present in them if not prepared carefully. ii) Metallic zinc may be present in Zn2o sample as Zn2o can prepared by heating metallic zinc. iii) NaCl prepared from rock salt which almost certainly contains traces of na, Mg compound. iv) Cuso4 prepae from comer pyrate may contains traces of iron. 2) Process used in manufacture i) Tap water is inriably used in the process. This tap water may contain cl, ca and mg which may come in sub. which is to be manufactured so the limits of these impurities have been prisorited in large number of pharmaceutical sub. ii) used in mfg. of certain chemicals. e.g. KI is mfg. from I2 and alkaline KOH. Iodine used is obtained from kelp a sea weed. When sea weed is burn some cynogen may be form so pharmacopeia prescribed limits test for cynide in KI and NAI also. Because of wide used strong acids in mfg. of medicinal sub. chloride and sulphate ion are very commonly occur in impurities, so test for an ions are generally included in pharmacopoeia. 3) Material of the plant The equipments or intensiles use in mfg. process are constructed out of metals like Cu, Al, Fe, Zn, Ni, and Sn or stainless steel. Due to solvent actions of the material of the plant. The traces of materials are introduced as impurities in the compound. The water pipe and steel pipe nay contain lead and hence pharmacopoeia prescribed limit test lead or heavy metals H2SO4 in mfg. by lead chamber process and so whenever chamber H2SO4 is used lead may be present as an impurities. 4) Inadequate storage i) Filth- stored product may contaiminated with dust, the body of insects and even animal. ii) Decomposition of product during storage many chemical subs. Undergo changes or decomposition dueto careless storage. e.g. a) due to careless storage FeSO4 is slowly converted into Fe2O by air and moisture. b) Surgical Solution of chlorinated soda due to riorates upon exposture. It is to be stored in well closed ambered coloured bottle in cool place. iii) Solution of KOH absorbed Co2 an exposture to air and heat action on lead glass. It should be stored in well stoppered bottles of green glass which is lead free. iV) Microbial contamination: liquid preparation and screen for topical application to ……………………….broken skin or weaker membrane are liable to bacterial mould and fungal ……………………….contamination from atmosphere. Types of Impurities Following types of impurities are commonly present in the pharmaceutical sub. or preparation. 1) The impurities which produce toxic effect on bodies if present beyond the limit e.g. pb, As, impurities. 2) Impurities which are harmless but if present beyond the limitsin pharmaceutical substances, lowers the active strength of that substance e.g. impurities of Na salt in potassium salt. 3) Impurities which if present beyond the limit affect storage property of produces pharmaceutical. 4) Impurities causing technical difference by using subs.in which it is present. E.g. presence of carbonate impurity in NH3 SOLn . 5) Impurities such as taste, odour or colour or appearance which are easily detectable by a senses and make the sub. anaesthatic or unhygienic. e.g. i) phenolic impurities present in sodium alkaline afterits colour. ii) traces of Mg salt in NaCl renders it damp and changing its appearance. Limit test Limit test are quantitative or semiquantitative test designed to identify and control small uantities of impurities which are likely to be present in the sub. these limit test involves simple comparison of opalescence, turbidity, colour and stain with standards prescribed in pharmacopoeias. The standards for apalescence, turbidity, colour or stain are fixed. In these limit test the extent opalescence, turbidity, or colour produces influenced by the presence of other impurities present in the sample and also variation in time and method of performance of the test. Hence the pharmacopoeia do not prescribe numerical values of the limit in this test. Hence the limit test are the test which are performed to know wheather the impurities in the drug below the limit or beyond the limit. Limit test for chlorides The limit test for chloride as been based on the simple reaction betn Agno3 and soluble chlorides to obtain AgCl which is insoluble in dilute nitric acid. The silver chloride produced in the presence of dil. NHO3 makes the test solution turbid, the extent of turbidity depending upon the amount of chloride present in the sub. is compared with a standard opalescence produced by addition of AgNO3 to a std. Solution having a known amount of chloride and the same value of dil. NHO3 as used in test Solution . If the turbidity form the sample has been less than the std. turbidity, the sample will pass the limit test and vice versa. A ml B ml 75 75 50 50 25 25 Nessler Cylinder White tile Method for the limiting test for chlorides IP 1985 Specified wto of the sub. is dissolved in water or the Solution is prepared by special treatment as directed in the pharmacopoeia and transferred to a Nessler cylinder A. to the Solution 1 ml of NHO3 is added and volume made up to 50 ml with water. Then 1 ml of AgNO3 Solution is added and Solution stirred. Cl- + AgNO3 NHO3 AgCl + NO3- Keep aside above Solution for 5 minutes. Simultaneously, for std. opalescence, place 1 ml of 0.05845 percent w/v Solution of nacl in Nessler cylinder B and add 1 ml of dil. HNO3, make up the volume to 50 ml with water and add 1 ml of AgNO3 Solution . stir with glass rod and set aside for 5 minute. The opalescence produced by the sample should not be greater thab std. opalescence. If the opalescence from the sample has been less thab the std. opalescence, the sample will pass the limit test. 𝑁𝑎𝐶𝑙 + 𝐴𝑔𝑁𝑂3 ⃗⃗⃗⃗⃗⃗⃗⃗⃗⃗⃗⃗ 𝐻𝑁𝑂3 𝐴𝑔𝐶𝑙 ↓ + 𝑁𝑎𝑁𝑂3 Test Solution Standard Solution Specified sub. (1g) + 10 ml H2O. 1 ml of 0.05845 % w/v solution of NaCl + + 1 ml of HNO3 dil. 50 ml in Nesslers 1 ml of HNO3 dil. 50 ml in Nessler cylinder A + 1 ml of AgNO3 solution cylinder B + 1 ml of AgNO3 solution. Opalescence Turbidity Opalescence Turbidity The Opalescence in sample & std. solution are compared by keeping the Nessler’s cylinder against proper background & observing side by side. Limit test for Sulphate Principle The limit test for sulphate is carried out on the basis of reaction betn barium chloride and soluble sulphates in prescence of dil. HNO3. Then, the comparison of the turbidity produced by a given amount of sub. is done with a std. turbidity obtained from a known amount of sulphate and same volume of dil. HCL have been added to both the Solution . the barium chloride test Solution in the I.P. has been replaced by barium sulphate Reagent which is have been added to increase the sensitivity of the test. Methods for limiting test for sulphate. A Solution of specified quantity of sub. is prepared in water or prepared as directed in the pharmacopoeia in Nessler cylinder and 2 ml dil. HCL is added except where HCL is used in preparation of Solution .Dilute to 45 ml with water add 5 ml of BaSO4 reagent, stir immediately with glass rod and set aside for 5 min. in order to produce std. turbidity place 1 ml of 0.1089 % w/v Solution of K2SO4 and 2 mil of dil. HCL in another Nessler’s cylinder, dil. To 45 ml with water and add 5 ml of BaSO4, stir immediately and set aside for 5 min. the turbidity produced by the sample Solution should not be greater than the standard turbidity. If the turbidity produced by the test Solutionhas been less thn std. turbidity the sample would pass the limit test for sulphate. SO42- + BaCl2 HCL BaSo4 + 2Cl- Test solution Standard solution Specified sub. (1g) + 2 ml HCl dil. To 45 ml + 1 ml of 0.1089% w/v Solution of 5 ml Solution of BaSo4 K2So4 + 2 ml HCl + H2O dil. to 45 ml + 5 ml BaSO4 Turbidity Turbidity Limit test for iron Principle The limit test for iron is based on the reaction of iron in ammonical Solution in presence of citoic acid, with thioglycollic acid when a pale pink to deep reddish purple colour is formed due to ferrous compounds. The colour produced from a specified amount of sub. from the test is compared by viewing vertically with a std. (Ferric ammonium sulphate). If the colour from Solution.is less dark than the std., then the sample passes the test. Ch2CL.COOH + KSH CH2CSH) COOH+ KCL This test is very sensitive. Interference of other metal cations is eliminated by making use of 20% citric acid which forms a complex with other metal cations. Method A Solution.is first of all obtained from a specified amount of sub. it is then taken in Nessler cylinder and to it 2 ml of 20% citric acid Solution. T.S. and 2 drops of thioglycollic acid are added. The Solution.are mixed made alkaline with a Solution.of iron-free ammonia and dil. To 50 ml mark and with water. The colour optained is compared with a std. prepared from 2 ml of std. Solution. of iron, with 40 ml of water in a Nessler cylinder following the same procedure as for the test Solution.. Ch2SH Ch2SH Fe2+ + 2 + 2 OOC + 2H+ Fe COOH Thioglycollic acid. COO HSH2O Ferrous thioglycolate. If the colour produced by test Solution has been less than that of std., the sample passes the limit test for iron. Test solution Sample + 40 ml of H2o + 2 ml of 20% w/v 20% Citric acid + 2 drops of thioglycollic acid, Standard solution 2 ml of std. Solution of iron + 40 ml water + 2 ml of w/v citric acid + 2 drops of thiogly colic acid, Solution Solution mixed, made alkaline with ammonia ml, made alkaline with ammonia and adjust to 50 and volume adjusted to 50 ml, allowed to allowed to stand and colour developed viewed Stand and colour developed viewed veotically and compared with test Solution. vertically and compared with std. solution Limit Test for Arsenic Principle The pharmacopoeial test is based on the fact that arsenic in the arsenious state can be easily reduced to arsine gas (AsH3). When his gas is passed over mercuric brornide paper, it produces a stain, which ranges in colour from yellow to brown, the intensity and length of which are proportional to amount of arsenic. Reduction of the Arsenic to arsine, both in the standard and sample may be achieved by the combined action of zinc, acid, stannous chloride, potassium iodide. The arsine is carried over by hydrogen to the mercuric bromide or mercuric chloride papers which are supported in test apparatus. When the sample is dissolved in acid, the arsenic present in the sample gets converted to arsenic acid which gets reduced by reducing agents to arsenious acid. The nascent hydrogen formed during reaction, further reduces arsenious acid to arsine which reacts with mercuric chloride paper giving yellow stain. H3AsO3 + 3H2 ASH3 + 3H2O Arsine H3AsO4 + H2SnO2 Arsenic acid H3ASO3 Arsenious acid H3ASO3 + H2SNO3 Arsenious acid + 3H2 ASH3 + 3H2O Arsine The depth of yellow stain on mercuric chloride paper will depend upon the quantity of arsenic present in sample. Apparatus It is having a wide mouthed glass bottle of 120 ml capacity having mouth of about 2.5 cm in diameter. This bottle is fitted with a rubber bung through which passes a glass tube, 20 cm long having an external diameter of about 0.8 cm and internal diameter of 0.65 cm. the tube is considered at its lower end extremity of about 1 mm and there is blown a hole not less than 2 mm in diameter. The upper end of glass tube has been fitted with two rubber bungs, each having a hole bored centrally and exactly 6.5 mm in diameter. One of the bugs has been fitted to upper end of tube while second bung has to be fitted upon the first bung in such a way that mercuric chloride papes gets exactly sandwiched between the central perforation of the two. The bungs are kept in close contact by using band or spring clip in such a manner that gas erored from bottle must have to pass through 0.65 mm internal circle of mercuric chloride paper. Rubber bungs Mercuric chloride paper 200mm long glass tubes with 8mm external diameter 6.5mm internal diameter 2mm hole for gas During test, the evolving gases have been passing through the side hole, the lower hole serving as an exit for water. The apparatus has the standardization of area of mercuric chloride paper which is exposed to action of arsine gas. Limit test for lead Principle Dithizone in chloroform is able to extract lead from alkaline aq. Solution as a lead dithizone complex (red in colour). The original dithizone is having a green colour in chloroform while the lead dithizone is having a violet colour. The intensity of the colour of complex in chloroform, has been compared with a std. volume of lead solution, treated in the same manner. The lead present as an impurity in sub. gets separated by extracting an alkaline solution with a ditizone extraction solution. The interference and influence of other metal ions etc have been eliminated by adjusting the optimum pH for the extraction by employing ammonium citrate. Potassium cyanide, hydroxylamine hydrochloride reagents, etc. Method (A solution of the of the sample is prepared as directed) A known quantity of the sample Solution is transferred to a separating funnel. To it 6 ml of ammonium citrate, 2 ml of potassium cyanide and 2 ml of hydroxylamine hydrochloride are added, followed by 2 drops of phenal red and the Solution is made alkaline by adding an ammonia Solution . this is then extracted with 5 ml portions of dithizone Solution until it becomes green. The combination of dithizone extracts are shaken for 30 sec., with 30 ml of 1 N HNO3 and the chloroform layer is discarded. To the acid Solution 5 ml of std. dithizone Solution is added along with 4 ml of ammonium cyanide and Solution shaken for 30 sec. The colour of the chloroform layer in case of sample being tested should not be of deeper shade of violet than of control which is made with a volume of pb Solution equivalent to the amount of lead permitted in sample under examination.during the preparation of a sample Solution an appropriate preliminary treatment is given, so as to get Pb in the Solution , without any interfering sub. or ion. All reagents used under the test must be free from lead and have been designated as PbT regents in pharmacopoeias. Limit test for heavy Metals Principle The limit test for heavy metals has been based upon reaction of metal ion with hydrogen sulphide, under the prescribed conditions of test causing formation of metal sulphides. The test Solution is compared with a std. prepared using a lead solution (as heavy metal). The usual limit as per I.P. has been 20 ppm. The I.P has adopted three methods for limit tests to heavy metals. The the method I is used for sub. which gives a clean colourless Solution under specified conditions. Method II is based or used for those sub. which do not give a clear clourless Solution under the test conditions specified for method I. method III is used for sub. that give clear colourless Solution in NaOH medium. Method I: This method is this method is based or applicable for the samoles which give clear colourless Solution under specified conditions of testStandard Solution (A) Take 2 ml od std. lead Solution by pipette in Nessler’s cylinder and dil it with water to produce 25 ml. Adjust the pH betn3 to 4 with dil. Acetic acid ‘sp’ or dilute ammonia Solution ‘sp’ Dilute with waterto about 35 ml. mix. Test solution (B) Take 25 ml of Solution which is prepared as per the procedure given under respective monograph from I.P. in Nessler cylinder. Adjust the pH betn3 to 4 by adding dil. Acetic acid ‘sp’ or dil. Ammonia Solution ‘sp’ Dilute with water to about 35 ml mix. To the above cylinders A and B each containing td. Solution and test Solution respectively. Add 10 ml of freshly prepared H2S. Mix well. Dilute with water to 50 ml. Allow to stand for five minutes. The colour produced in test Solution is not darker than that produced in std. Solution. Method II: The standard Solution can be prepared in same way as in method I. Test Solution may be prepared by weighing specific quantity of sub. As per monograph in crucible. Moisten the sub. With H2SO4. Ignite on a low flame till completely charred. Add few drops of HNO3 and heat to 500O . Allow to cool, add 4 ml of HCl and evaporate to doyness. Moisten the residue with 10 ml of HCl and digest for two minutes. Neutralize with ammonia Solution and make just acidic with acetic acid. Adjust pH 3 – 4 filter if necessary. Adjust volume of filtrate to 5 ml in Nessler’s cylinder. Add 10 ml of H2S Solution , dilute to 50 ml with water and compare colour with std. Solution . Method III: The std. Solution could be prepared by using 2 ml std. lead Solution , adding 5 ml dil. NaOH Solution and making volume to 50 ml with water. For the test Solution taker either 25 ml Solution prepared as per monograph or take specified quantity of sub. , dissolve in 20 ml water and add 5 ml dil. NaOH and make up volume to 50 ml. To each of above Solution in Nessler’s cylinder add 5 drops of sodium sulphide Solution . mix and setaside for 5 min. The colour produced by test Solution is not darker than std. solution. Test of Purity Test for purity is the test for the presence of impurities and fix the limits of tolerance for these impurities. Some of the tests performed for testing impurities are: 1) Colour, Odour and taste; when other tests for purity are not available. Then the tests of Odour, colour, etc are used. They are useful in determining wheather sub has been reasonably pure, hygienic , etc or not. 2) Physico – chemical constant: Solubility of sub. In different solvent, determination of M.P. and B.P for organic substance, optical rotation for optically active sub. and refractive index for liquids, have been some reliable values which can reveal the purity of sub. Determination of acid value, iodine value, saponification value, ester value, etc for vegetable oils have been general constants and a variation in their value, signifies the presence of impurities. 3) Acidity, Alkalinity, and pH: sub. Prepared from chemical reaction which are involving acids and alkalinity often have considerable amount of acid or alkali as an impurity. Hence, test fir acidity or alkalinity have been of a great help for determining the extent of impurity. The solutions of certain sub. Are having a definite pH, at a given conc. The presence of impurity will cause a change in pH. 4) Humidity: Estimation of moisture or humidity content of som crude drugs provide valuable information about the conditions of their storage and inturn about their therapeutic potency. 5) Cations and Anions: Many synthetic drugs both organic and inorganic may be prepared using strong acids like HCl, H2SO4, HNO3,, etc. The presence of chloride and sulphate ion have been common. Tests of ion (anions) are usually carried out especially in testing synthetic organic compounds. Similarly tests for Sodium, ammonium (cations) are usually carried out to detect impurities in organic compounds. 6) Insoluble constituents or Residue: A sub. Which in pure state gives a clear Solution with a given solvent produces a turbid Solution in presence of insoluble impurity. The measurement of opalescence helps to indicate the extent of impurities and thus providing good check on purity of soluble sub. 7) Ash, water, insoluble ash: Determination of ash in crude vegetable drugs, organic compounds and some organic compounds, service a good indication about extent of impurities of heavy metals and minerals in Dature. In certain cases, water-insoluble ash is also determined to ascertain water-insoluble heavy metals or mineral types of impurity. 8) Organic Impurities : The test are necessary to know the impurities in process of production for those sub. Which have been either significant in use of medical compound or which serve as a criteria for its freedom from other impurities. Quantitative Assay Assay An assay is an analysis done to determine the presence of sub. and amount of that sub. Or pharmacological potency of a drug. Assay of Aspirin Title; Acetylsalicylic Acid. (Mol. Wt 180.16) COOH O O – C - CH3 CgH8O4 Aspirin is 2 – acetorytenzoic acid. Category, Analgesic, antipyretic, antirheumatic, antirheumatic, antithrombotic . Dose; As analogesic and antipyretic, 300 – 600 mg four to six times a day. As antirheumatic, 1 to 2 g four to six times a day up to 10 g daily. As antithromobotic 75 mg daily. Description Colourless crystals or white, crystalline powder, odourless or almost odourless. Solubility; Freely soluble in ethanol (95%), soluble in chloroform and ether, slightly soluble in water. Principle: The determination aspririn is based on back Titration. The back titration is followed when the direct titration is not possible. This method is used for weak acids or weak base. In the assay sample is dissolved in ethanol (96%) because of its low solubility in water (1 in 300). Alkaline hydrolysis of aspirin is carried out with a known excess of std. alkali Solution and residual (excess) alkali Solution is back titrated with std. HCl Solution using phenol red as indicator. Black determination is required to minimize the errors. Phenol red having pH range betn 6.8 – 8.9. It has yellow colour in acidic and red colour in alkaline pH. Back titration reading substracted from black reading gives amount of NaOH required to hydrolyze Aspirin. Chemical Reaction COOH COONa 1) + 2 NaOH + CH3COONA + H2O OCOCH3 ON 2) NaOH + HCl NaCl + H2O Assay Weigh accurately about 1.5 g, dissolve in 15 md of ethanol (95%), add 50 ml of 0.5 M NaOH, boil gently for 10 min., cool and titrate excess of alkali with 0.5 HCl using phenol red indicator. Repeat the operation without the sub. Being examined. The diff. betn the titrations represents the amount of NaOH required. Each ml of 0.5 m NaOH is equivalent to 0.04504 g of CgH8O4. Aspirin Tablets Usual strength: 75 mg, 150 mg, 300 mg, 600 mg. Storage: store in tightly-closed containers in a cool, dry place. Standards: Aspirin tablet contains NLT 95% and not more than 105% of stated amount of Aspirin (CgH8O4). Assay: Weigh and poweder 20 tablets. weigt accurately a quantity of powder equivalent to 0.5 g of Aspirin, add 30 ml of 0.5 M NaOH, boil gently for 10 min., cool and titrate excess of alkali with a 0.5 M HCl using phenol red Solution as indicater. Repeat the operation without the sub. Being examined. The difference betn titrations respresents the amount of NaOH required. Each ml of 0.5 M NaOH is equivalent to 0.04504 g of CgH8O4 Assay of Ascorbic Acid Title: Vitamin C,L-Ascorbic acid (Mol.wt. 176.13) Ascorbic acid is (R) – 5 – ((S) -1, 2, dihydnonyettyl) -3, 4- Dihydrony -5(H)-Frran-2-one. CH2OH H C OH O O HO OH C6H8O6 Category: Vitamin (Antiscorbutic) and pharmaceutical aid (Antioxidant). Dose: Prophylactic, 25 to 75 mg, daily, therapeutic NLT. Description: Colours crystals or white to very pale yellow crystalline powder, odourless. On exposure to light it gradually darkens. Solubility: Freely soluble in water, sparingly soluble in ethanol (95%), insoluble in chloroform and ether. Principle: Assay of ascorbic acid is based on oxidation- reduction (Iodometric) titration. Iodometric titration refers to titration with a standard Solution of iodine. It is quantitative oxidation of ascorbic acid to dehydroascorbic acid with iodine solution, Ascorbic acid (Vitamin C) rapidly reduces iodine to iodide and can form the basis of a direct titration of Vitamin C with a starch as an indicator. A Solution of iodine is aq. Iodine has an intense yellow to brown colour, starch reacts with iodine in presence of iodine to form an intensely blue colour complex which is visible at very low conc. Of iodine. The great merit of starch is that it is inexpensive. As it forms water insoluble complex with iodine, the indicator has to be added comparatively late in titration, sometimes just before end point. Chemical Reaction CH2OH CH OH CH2 OH O O CH OH O O +2HI + I2 OH OH O O Assay Weigh accurately about 0.1 g and dissolve in mixturs of 100 ml of freshly boiled and cooled water and 25 ml of 1M H2SO4 . Immediately titrade with 0.5 M iodine using starc indicator until blueviolet colour is abtain. Each ml of 0.05 N iodine is equivalent to 0.008806 g of C6H8O6. Ascorbic Acid Tablet Usual strengths – 50 mg, 100 mg, 500 mg. Storage – store in tightly-closed, light resistant containers avoiding contact with metals. Standards – Ascorbic acid tablet contain NLT 95% and not more than 115% of the stated amount of ascorbic acid (C6H8O6). The tablets may contain permitted colouring and flavouring agents. Assay – weigh and power 20 tablets. weigh accurately a quantity of the power eq. to 0.15 g of ascorbic acid and dissolve as completely as possible in mixture of 30 ml of water and 20 ml of 1 M H2SO4. Titrate with 0.1 M ceric ammonium sulphate usinf ferroin sulphate Solution as indicator. Each ml of 0.1 M ceric ammonium sulphate is equivalent to 0.008806 g of C6H8O6 . Assay of calcium Gluconate Title – calcium gluconate is calcium D-gluconate monohychate. Category – Calcium replenisher. Dose – orally up to 15 gm daily in divided doses. By intramus- cular or slow intravenous infection, 1 to 2 g. (500mg of calcium gluconate is approximately eq. to 2.3 M mol of Ca++). Description – white, crystalline powder or granules. Solubility - sparingly soluble in water but freely soluble in boiling water, insoluble in ethanol (95%). Storage – store in well- closed container. Principle – This a complexometric titration. Disodium EDTA is used as a complexing agent, (mordant black II) Eriochome, black T is used as indicator. With calcium ions alone, no sharp end point can be obtained with Eriochome black indicator and transition from red to pure blue is not observed. Therefore, a known volume of 0.05 M MgSO 4 Solution is added to sample before titration. The magnesium ions are not complex by EDTA in presence of calcium ions since the Ca-EDTA complex is more stable than that of Mg-EDTA and Mg-indicator complex is more stable than calcium indicator complex but less stable than Mg-EDTA complex. Therefore, during titration, the EDTA react first with free calcium ions then with free magnesium ions and finally with magnesium indicator complex. When all the calcium ions have been complexed, then the Mg indicator complex breaks, liberating free Mg ions which forms complex with EDTA. Since the Mg-indicator complex is wine red in colour and free indicator is blue (app. At pH 10)the colour of Solution changes from wine red to blue at endpoint. Use of ammonia – NH4Cl Solution – 1) The free indicator has blue colour of pH 10 and complex has red colour at pH 10 below pH 6.3 and above 11.5, dye has redish colour, so use of buffer with pH 10 is essential. 2) pH has marked effect on stability of complex formed since the reaction of metal ion M h+ with ligand EDTA involves production of acid and reaction being reversible, appropriate buffer of alkaline range are employed. If acid is not neutralized and removed, complex will break. Chemical reaction – Ca++ + H2Y2Mg++ + EDTA2Ca + Mg – EDTA CaY2- +2H+ Mg – EDTA Ca – EDTA + Mg++ Assay – weigh accurately about 0.5g and dissolve in 50 ml of warm water, cool, add 5 ml of 0.05M MgSO4 and 10 ml of strong NH3 Solution and titrate with 0.05M disodium edetate using mordan black II mixture as indicator. From the volume of 0.05M disodium edetate required substract the folume of MgSO4 solution added. Each ml of remainder of 0.05M disodium editate is eq. to 0.02242g of C12 H22 Ca O14, H2O. Calcium Gluconate Injection Usual strength – the eq. of 500mg and 1g of calcium gluconate is 5ml. the eq. of 1gm of gluconate in 10ml. (A 10% w/v solution of calcium gluconate containes app. 0.45m mol of Ca++ per ml). Assay – to an accurately measured volume eq. to 0.5g of calcium gluconate add 50 ml of water and complete the assay. Add 5 ml of 0.05M MgSO4 and 10 ml of strobg ammonia solution andtitrate with 0.05M disodium edetate using mordant black II as indicator. From the volume of 0.05M disodium edetate required substract the volume of MgSO4 solution added. Each ml of remainder of 0.05M disodium edetate is equivalent to 0.02242g of C12 H22 Ca O14, H2O. Assay of Ferrous Sulphate FeSO4 . 7H2O Mol0.wt. 278.01. Category – Haematinic. Dose – prophylactic, 300 mg, therapeutic 600 to 900 mg daily, in devided doses, (300 mg of FeSO4 is app. Equivalent to 60 mg of ferrous iron). Solubility – very soluble in boiling water, freely soluble in water, practically insoluble in ethanol (95%). Storage – store in tightly- closed containers. Standards – FeSO4 contains NLT 98% and not more than 105% of FeSO4 . 7H2O . Principle – It is a redox titration (ceriometric titration) in which Fe+2 get oxidized to Fe3+ and Ce4+ get reduced to Ce3+ . Oxidation reduction titrations involving ceric sulphate as an oxidizing agent are called as ceriometric titrations. Cerium sulphate is a powerful exidizing agent in acid solution. It is bright yellow in colour, both in solid state and in solution and since the corresponding cerium (IV) salt formed by reduction is colourless, strong solutions are self indicating. However, usually 0.1M solution are used and this conc. Is too dilute for observation of end point without addition of suitable indicator. Ferroin sulphate solution is added as an indicator. End point will be red to light blue. Chemical reaction – 2FeSO4 + 2Ce (SO4)2 , 2(NH4)2 SO4 Fe2 (SO4)3 + 2NHCe (SO4)2 + 6NH3 + 3H2SO4 Assay – Dissolve 2.5 g of sodium bicarbonate in a mixture of 150 ml of water and 10 ml H2SO4 . when efferevescence ceases , add 0.5g of sub. Being examined, accurately wt. shake gently to dissolve and titrate with 0.1 M ceric ammonium nitrate using 0.1 M of ferroin solution as indicator. Until the red colour disappears. Each ml of 0.1M ceric ammonium nitrate is equivalent to 0.02780 g of FeSO4 . 7H2o . Ferrous Sulphate Tablets Usual Strength – 200 mg (200 mg of dried Ferrous sulphate is app. Equivalent to 60 mg of ferrous ion). Storage – store in tightly-closed container. Labelling – The label state the quantity of the active ingredient both as the amount of dried ferrous sulphate and in terms of equivalent amount of ferrous iron in each tablet. Standards – Ferrous sulphate tablets contain NLT 80% and not more than 90% of the stated amount of dried ferrous sulphate, FeSO4. The tablets are coated. Assay – weigh and powder 20 tablets. weigh accurately a quantity of the powder equivalent to 0.5 g of dried FeSO4 and carry out assay as described above. Assay of Hydrogen Peroxide Principle The assay is based on oxidation reduction titration. Hydrogen peroxide is oxidizing agent but in acidic medium it acts as reducing agent and it can be titrated against KMNO4 solution. It is a good practice to use fairly high conc. Of acid and a reasonable low rate of addition in order to reduce the danger of forming manganese oxidewhich is an active catalyst for the decomposition of hydrogen peroxide. Potassium permanganate is a good example of self indicating reagent. One drop excess will impart a visible pink colouration even in presence of slightly coloured ions such as ferric ions. Solutions containing MnO4- are purple in colour, solution of salts, containing Mn++ ions are colourless hence a permanganate solution is decolorized when added to a solution of a reducing agent (H2O2) as long as latter is present in the solution. The moment there is an excess of KM n44 solution it becomes purple. Thus permanganate ion can serve as its own indicator, especially in acidic solution. The colour of cerium sulfate and iodine solution have also been employed in the detection of end points. Chemical reaction 2 KMnO4 + 3H2SO4 + 5H2O2 2 mnSO4 + K2SO4 + 8H2O + 5O2 Assay of Ciprofloxacin Hydrochloride Title C17 H18 FN3O3 , HCl , H2O Mol.wt. 385.82 Ciprofloxacin Hydrochloride is 1- cyclopropl -6- fluoro – 1 , 4 – dihycho – 4- ono -7- (1- piperazinyl)3- quinolone – carboxylic acid hydrochloride monohydrate. Category : Antibacterial Dose: The equivalent of 250 to 750 mg of ciprofloxacin hydrochloride, twice daily, (116 mg of ciprofloxacin) Description: Pale yellow, crystalline powder. Solubility: Soluble in water, slightly soluble in acetic acid and in methanol, very slightly soluble in ethanol, practically insoluble in acetone, in acetonitrile, in ethyl acetate, in hexane and in dichloromethane. Storage: Store in tightly-closed, light resistant containers. Standards: Ciprofloxacin Hydrochloride contains NLT 98% and not more than 102% of C17 H18 FN3 O3 , HCl, calculated with reference to the anhydrous substance. Assay: Carry out the assay described under ciprofloxacin using following solution in the mobile phase. Solution (1) is a 0.05% w/v solution of sub. Being examined. Solution (2) contains 0.05% w/v ciprofloxacin hydrochloride RS. Solution (3) contains 0.05% w/v each of ciprofloxacin ethylenediamine along RS and ciprofloxacin hydrochloride RS. Calculate the content of C7 H18 FN3O3, HCl in ciprofloxacin hydrochloride RS. Assay of ciprofloxacin: Title C17 H18 FN3O3 Mol.wt.331.35 Ciprofloxacin is 1-cyclopropyl-6-fluoro-1, 4-dihydro-4-ox 7-(1-piperazinyl)-3-quinoline carboxylic acid. Category : Antibacterial Dose: Orally, 250 to 750 mg twice daily, by intra venous infusion, 100 mg to 200 mg twice daily. Description: white to pale yellow, crystalline powder. Solubility: very slightly soluble in ethanol and dichloromethane, practically insoluble in water. It dissolves in dil. Acetic acid. Storage: Store in tightly-closed, light resistant containers. Principle: Assay is based upon high performance liquid chromatography (HPLC). HPLC is essentially a form of column chromatograph in which the stationary phase. Consist of small particle (3-50u) packings contained in a column with a small bore (2-3 mm), one end of which is attached to a source of pressurized liquid eluant (mobile phase). The three forms of HPLC most often used are ion exchange, partition and absorption. Assay: Carry out method for HPLC, using following solution. For solution take about 25 mg accurately weighed, of the sub. Being examined in a 50 ml volumetric flask, add 0.2 ml of solution containing 7% v/v of phosphoric acid dilute to volume with the mobile phase and mix to dissolve solution (2) is a similarly prepared solution of ciprofloxacin RS. Solution (3) is a 0.05% w/v solution of ciprofloxacin ethylenediamine analog RS in solution (2) Inject 10 uL solution (3) and record the chromatogram adjusting the sensitivity. Separately inject 10 uL of solution (1) and (2), record the chromatogram and measure the peak response of major peaks. Calculate the content of C17 H18 FN3 O3 from the declared content of C17 H18 FN3 O3 in ciprofloxacin RS. Assay of thiamine Hydrochloride Title C12 H17 Cl N4 OS, HCl Thiamine hydrochloride is 3-((4-amino-2-methy) pyrimidire 5- yl)methyl)-5-(2-hydroxyethyl)-4methy) thiazolium chloride hydrochloride. Category –B- group vitamin. Dose prophylactice, Orally, 2 to 5 mg once daily, therapeutic, orally or by subcutaneous or intramuscular injection, 25 to 100 mg daily. In multivitamin preparations, prophylactic, orally 1 to 2 mg daily. Therapeutic, orally 4.5 to 10 mg. Description : white or almost white, crystalline powder or small colourless crystals, odour, slight and characteristic. Solubility: freely soluble in water, slightly soluble in ethanol (95%), practically insoluble in chloroform and ether. Storage: store in tightly closed, light resistant, non-metallic container. Principle: The determination is based upon non aqueous titration. Sub. Which give poor end point due to being weak acids or basis in aq. Solution will frequently give more satisfactory end points when titrations are carried out in nonaqueous media. An additional advantage is that many sub. Which are insoluble in water are sufficiently soluble in organic solvents to permit their titrations in nonaqueous media. Various solvents are used in nonaqueous titrations such as glacial acetic acid, acetonitrile, dioxin, etc. The most common titrant used is perchloric acid. Although indicators may be used to establish individual end points potentiometric methods of end point detection are also used extensively, especially for highly coloured solution. Chemical Reaction Assay: Weigh accurately about 0.15g, dissolve in 5 ml of anhydrous formic acid, add 65 ml of anhydrous glacial acetic acid and 10 ml of mercuric acetate solution, with stirring and carry out method A for non-aq. Titration. Determine end point potentiometrically perform a blank determination and make any necessary correction. Each ml of 0.1 M perchloric acid is equivalent to 0.01689 g of C12 H17 ClN4OS, HCl. Assay of Trimethoprim Principle: Refere assay of Thiamine Hydrochloride principle. Chemical Reaction Assay of Insulin Insulin is the specific natural anti diabetic harmone obtained from the pancrease of either pig or ox. Category: Hypoglycaemic. Dose: By subcutaneous, intramuscular or intravenous injection, or intravenous infusion, in accordance with needs of patient. Description: white or almost white powder Solubility: practically insoluble in water, in chloroform, in ethanol (95%) and in ether. Storage: store in tightly-closed, light resistant container. At a temp. not exceeding -20O until released by manufacturer. It should be stored at a temp. of 2O to 8O and used for manufacture of preparation within a short period of time. Principle: Assay is based on HPLC. HPLC is also known as high pressure liquid chromatography is essentially a form of column chromatography in which the stationary phase consists of small practicle (3-50 u) paclcings contained in a column with a small bore (2-5 mm), one end of which is attached to a source of pressurized liquid eluant (mobile phase). The three forms of HPLC most often used are ion exchange partition and adsorption. Assay : Carry out method for HPLC. For solution (1) dissolve 40 mg of sub. Being examined in sufficient 0.025 M HCl to produce 50ml. solution (2) contains 0.08% w/v of bovine insulin RS in 0.025 M HCl. Solution (3) contains 0.08%, w/v of porcine insulin RS in 0.025 M HCl. Solution (4) contains 0.04% w/v each of human insulin RS and porcine insulin RS in 0.025 M HCl. Inject 50 uL of each of solution but using either solution (2) or solution (3), as appropriate, taking into consideration species from which insulin in the sub. Being examined. Take the chromatogram and find peaks. Inject solution (1)and either of solution (2) or (3) as appropriate, alternately six times and record chromatograms. The test is not valid unless relative standard deviation of area of principle peak is not more than 2%. Calculate the content of insulin from peak areas. QUALITY CONTROL FOR DOSAGE FORMS Dosage Forms Drugs are rarely administrated in their original pure state. They are administered in different dosage forms after converting them into a suitable formulation. every dosage form is a combination of the drug and different kinds of non-drug component called additives. Importance: Transformation of drug into different dosage forms is done for the following reasons: 1) to protect the drug sub. From oxidation, hydrolysis and reduction e.g. coated tablets and sealed ampoules. 2) To protect the drugs from the destructive effect of gastric juice (HCl) of the stomach after oral administration e.g. enteric coated tablets. 3) To provide a safe and convenient delivery of accurate dosage. 4) To conceal the bitter, salty or obnoxious taste or ordure of a drug sub. e.g. capsule coated tablets and flavored syrups, etc. 5) To provide optimum drug action through inhalation therapy e.g. inhalation aerosols and inhalants. 6) To provide for the insertion of the drug into one of the body cavities e.g. rectal or vaginal suppositories. 7) To provide the maximum drug action from topical administration site e.g. creams, ointments, ophthalmic preparations and ear, nose and throat preparations. 8) To provide sustained released action through controlled released mechanism e.g. sustained released tablets, capsules andsuspension. 9) To provide liquid dosage forms of the drug soluble in a suitable vehicle e.g. solutions. 10) To provide liquid preparation of the drug which are insoluble or unstable in different vehicles e.g. suspensions. 11) To provide the drugs with in body tissues e.g. injections. Classification of Dosage Forms Dosage forms may be classified on the basis of physical form of the final product which are as follows in flow sheet. 1) Solid dosage form. 2) Liquid dosage form. 3) Semi-solid dosage form. 1) Solid dosage form The solid dosage forms are available mostly in unit dosage forms such as tablets, capsules, pills, cachets and powders. When drugs are to be administered orally in dry state, tablets and capsules are the most convenient dosage form. They are effective and patients have no problem in handling, identification and administration. Some solids are packed and supplied in bulk. The bulk forms meant for internal use are supplied either as granules or fine powder. The bulk powders meant for external use are dusting powders, insufflations, snuffs and tooth powders. Dosage Forms solid dosage forms unit dosage form e.g tablets, capsules, pills, powders. Internal External e.g. dusting powders, insufflations. snuffs, ear powders liquid dosage forms Bulk Monophasic External,Liniments, lotions, gargles, sprays, mouth washes, eyen nasal drops, eye lotions Internal, syrup, Elixirs, Linctus, Drops Biphasic emulsion suspension semisolid dosage forms External, ointments, creams, pastes, jellies Internal, suppositories,pessaries 2) Liquid dosage forms Liquid dosage forms are meant for internal, parenteral or external use. They are available in monophasic or biphasic forms. A) Monophasic Liquid Dosage Forms: They are represented by true or colloidal solution. Water is used as solvent for majority of monophasic liquid dosage forms. A solution is homogeneous because the solute is in an ionic or molecular form of subdivision. Monophasic liquid dosage forms are available as: i) Liquid for internal use e.g. syrups, elixirs, linctus , drops. ii) Liquids for external use whish are of two types: a) Liquids to be applied to skin e.g. liniments and lotions, etc. b) Liquids meant for body cavities e.g. gargles, throat paints, mouth washes, eye, ear, nasal drops, spray and inhalations. B) Biphasic Liquid Dosage Forms: The liquids which consist of two phases are known as biphasic liquids one of which is dispersed as minute globules into the other. The liquid which is converted into minute globule is called dispersed phase and liquid in which globules are dispersed is called continuous phase in case of emulsion. While in case of suspensions the finely divided solids are dispersed in a liquid which acts as a continuous phase. 3) Semisolid dosage forms: semisolid dosage forms are mainly meant for external applications e.g. ointments, creams, pastes, jellies, etc. a) Ointments : They are semi-solid preparations meant for application to the skin or mucous membrane. They usually contains a medicament or medicaments dissolve, suspended or emulsified in the ointment base. The ointments are mainly used as protective or emollient for skin. The ointments which are meant for application to the eye are called ophthalmic ointments. An ideal ointment base should possess properties like: It should be inert, odourless and smooth. It should be physically and chemically stable. It should not produce irritation or sensitization and skin. b) Creams: These are viscous semi-solid emulsions which are meant for external use. The creams are of two types, a.q. and oily creams. In case of aq. creams, the emulsions are oil-in-water type and in case of oily creams, emulsions are water in oil type. A suitable preservative is generally added in aq. creams which have the tendency to bacterial and Ringal growth. Creams should be stored and supplie in well closed containers which prevent evaporation and contamination. c) Pastes: pastes are semi-solid preparations intended for external application to the skin. They differ from ointment as they contain a high proportion of finely powdered medicaments such as Zno, CaCO3, starch, etc. These sub. make the paste very thick and stiff. Pastes are less greasy than ointment. The stiffness property of paste makes them useful for protection. They are used mainly as antiseptic, protective or smoothing dressings which are often spread on lint before being applied. Pastes should be stored and supplied in containers maid of materials which do not allow absorption or diffusion of contents. d) Jellies: They are transparent or translucent, non-greasy, semi-solid preparations mainly used for external application to the skin. They are also used for lubricating catheters, surgical gloves and rectal thermometers. The sub. like gelatin, starch, tragacanth, sodium alginate and cellulose derivatives are used in preparation of jellies. Emulsion Emulsion are thermodynamically unstable, heterogeneous, biphasic system consisting two immiscible liquids, one of which is dispersed as minute globules into the other liquid. The liquid which is converted into minute globules is called as dispersed phase or internal phase and liquid in which globules are dispersed are called as continuous phase or external phase. Emulation is stabilized by emulsifying agents. Types of emulsion: There are two types of emulsion. i) ii) Oil in water (o/w) Water in oil (w/o) i) o/w: In oil in water type of emulsion oil is dispersed phase where as water is continuous phase where as water is continuous phase. The o/w type of emulsions are preferred for internal use. In o/w type of emulsion gumacacia, tragacanth, methyl cellulose, saponines and soap derived from monovalent bases like Na, k, NH3 are used as emulsifying agent. w/o: In water in oil type of emulsion water is dispersed phase where as oil is continuous phase. The w/o type of emulsions are mainly used externally as oinments or creams. Wool fat, bees wax, resins and soap derived from divalent cations like ca2+ , Mg2+, Zn2+ are used as emulsifying agent. ii) Identification Test Several test are available to identify the types of emulsion which are as follows: 1) Miscibility Test / Dilution Test: The emulsion is diluted with water in case if the emulsion remains stable after it’s dilution. Then it is o/w type of emulsion. In case w/o type emulsion breaks on it’s dilution with water but remains stable when diluted with oil. 2) Dry Test (colour test): Water phase or oily phase shows colouration when an emulsion is triturated with water or oil soluble colouring agent respectively. Scarlet red is only soluble in oil which is mixed with emulsion place a dn5p of emulsion on microscopic side, cover it with cover slip and examine it under microscope. If the dispersed globules appears red and background appears appears colourless it is o/w type of emulsion. The reserve condition occurs in w/o type of emulsion i.e. dispersed globules appear colourless in red background. 3) Conductivity test: water is a good conductor of electricity where as oil is bad conductor of electricity. the conductivity test can be performed by dipping pair of electrode connected through low voltage bulb in the emulsion. If bulb glows on passing the electric current then it is called o/w type emulsion because water is in continuous phase. In case the bulb does not glow the emulsion is of w/o type because oil is in continuous phase. 4) Fluorescence test: many fixed oil shows fluorescence when exposed to UV radiation. On microscopic observation of an emulsion under UV radiation the whole field fluorescence indicate presence of oil is in continuous phase (w/o) and droplet fluorescence indicate presence of oil is in dispersed phase (o/w). 5) Cobalt chloride test: anhydrous cobalt is blue and hydrated cobalt is red in colour. Treat filter paper with cobalt chloride solution and dry it. Dip dry treated paper is an emulsion. The change in colour of paper from blue to pink red indicates o/w type of emulsion and if paper remains same indicate w/o type of emulsion. Suspension Suspensions are heterogeneous biphasic liquid in which insoluble solid particles are uniformly distributed in liquid phase which are stabilized by suspending agents such as compound powder of tragacanth, mucilage sodium carboxy methyl cellulose and bentonite. Ideal properties of physically stable suspensions are as follows: i) Suspension should contain uniform distribution of mono sized, fine particles and the particle size of suspended solid should remain fairly constant through out it’s shelf life. ii) Particles should not settle rapidly at bottom of container. iii) The sediment should rapidly redispersible upon gental shaking of container and remain suspended long enough for a dose to be measured. iv) Suspension must be chemically stable. v) Viscosity of suspension should not make unpourable. Flocculated suspension 1) Suspended particles are in the form of loosely bound groups. Deflocculated suspension Particles are either individuals or in the form of aggrigates or exist as separate entities. 2) Suspensions are prepared by adding suitable flocculating agent. No flocculation is develop. 3) Rate of sedimentation of floccules is high ( since settles down as the folc which is collection of particles. The rate of sedimentation is low as the large particles sediment first followed with small particles. 4) The sediment is formed rapidly. The sediment is formed slowly. 5) The floccules sweep off any fine particles during setting and producing clear supernant liquid. The suspension liquid is turbide delayed settling of fine particles. 6) Sediment is easy to redisperse. Sediment is hard cake and difficult to disperse. 7) Sediment is loosly packed contain entrayed liquids and with higher sediment value. 8) These are physically stable suspension. 9) Through these are physically stable the appearance is pour due to separation and adherence of floccules to the site of container. The sediment is closely packed with low sediment volume. The physically stable suspension are prepared by addition to structure vehicle. The appearance is better. Quality Control Test For Emulsion Emulsion is necessary step in any formal development. Since it can be judge whether the developed product show the projected quality or not. Emulsion is biphasic product. Therefore the stability of it’s physical structure is of most important. The following evaluated test are carried out on the emulsion. 1) Globule size: Growth in globule size after the preparation of an emulsion is an indication of it’s physical instability. Hence, globule size and it’s distribution is generally a curtained in an emulsion per a certain. If a globule size is continuous to growth, it is indicative of poor formation of stability and phase separation occurs after certain time period. The globule size is measured by microscopic method or by electronic devices such as counter current. 2) Phase separation: the phase separation is result of creaming coagulation of globules. The rate and degree of phase separation in an emulsion can be easily determined by keeping a certain amount of emulsion in an graduated cylinder and measuring he volume of separated phase after definite time interval. This test can be accelerated by centrifugation at high speed of centrifugation. The poor emulsion would crack of completely while good formulated emulsion will survive due to tough interfacial time on the globules. 3) Flow property: Flow property of an emulsion is the manrfestation of globule size, type of emulgent, it’s conc. and phase volume ratio. Therefore, the study of flow property serve as an index of an emulsion stability. Any instrument suitable for the measurement of viscosity (brook field viscometer) can be used for the study of flow properties. 4) Effect of thermal traces: The emulsion are subjected to high (60OC) or low (0 – 40OC) temp. in alternating cycles. In emulsion which can bears this thermal traces are judge are good emulsion. This evaluation test are significant that no formulator can wait for a years to evaluated shelf life of his product and hence inorder to get some assurance of structure stability for longer period thermal traces are given to the product. Powders Defination: Pharmaceutical powders are solid dosage forms which consists of mixture of dry powder drugs intended for internal or external use. Dusting powders Powders for external use are termed as dusting powder. Dusting powders are not applied on broken skin and areas that are very moist, otherwise powder tends to cake. and abrade the skin. Powders for external use should be served through sieve no.85 because fine powders have more covering capacity more adsorptive properties and these are less irritant. Powders for external use can be dispersed in container with perforated closure or in an aresol container for spraying. The sterile dusting powder for application on openwound are called as surgical dusting powder. There are two types of dusting powders. i) Medicated dusting powder. ii) Surgical dusting powder. a) Medicated dusting powder: medicated dusting powder intended to be applied on interact skin have adsorption astringent and protective properties. These mainly composed of zinc oxide, boric acid, talke, kaolin, starch, etc. b) Surgical dusting powder: surgical dusting powder are used in treatment of wound, burns and on broken skin. These usually contain an tibacterical agent and there must be sterile. These should be packed in heat resistant paper, envelop or in small size glass or plastic bottles having nozzle attached. Additives Defination: Substances which are of little or no therapeutic value but which are added to the formulation in order to ease the production to maintain physiothermal stability to improve patient acceptability and functioning of the dosage form as a drug delivery system are called pharmaceutical addictives. They are also known as pharmaceutical aids, necessities, adjuncts, adjuvant or excipients. Some sub. are not only used as pharmaceutical additives but they also have some therapeutic value. Therefore, while selecting these, the formulator has to keep a balance betn the desire function and its therapeutic value. e.g. agar, castor oil are laxatives, alum, zinc oxide are astringents, chloroform is a general anaesthetic, lactose has nutritive value, lactic acid is ametabolic neutralizer. Ideal properties of Additives: 1) Physiologically inert. 2) Physic-chemically stable over a wide range of temp. pH and not reacting with other formulation ingredients. 3) Does not impart any undesired taste, odour or colour to the product. 4) Must be non-toxic, non-irritant, non-sensitizing. 5) Should be effective in low concentration. 6) Must be free from micro organism considered to be pathogenic or otherwise objectionable. 7) Must not interfere with bio-availability of drug. 8) Must be accepted by regulatory authorities. 9) Must be commercially available in form and purity that is commensurate with pharmaceutical standards at reasonable coast. Classification Pharmaceutical additives are classified on the basis of their functions as: 1) To produce a particular dosage form: a) Diluents or filters for solid dosage forms. b) Vehicles or solvents for liquid dosage forms. c) Semisolid bases for ointment creams. d) Propellants for sprays. 2) To attain and maintain physical stability of formulation a) Co-solvents, agents for solutions. b) Suspending or emulsifying agents for disperse system. c) Binders, disintegrating agents for solid dosage forms. 3) To attain and maintain chemical stability of formulation. a) Antioxidants b) Buffers. 4) Preservatives to control-microbial contamination. 5) To ease manufacturing of product. a) Lubricants, anti-adherents, glidants for solid dosage forms like tablets, capsules. b) Antifoaming agents for liquids and semisolids. 6) Organoleptic additives a) Colouring agents. b) Flavouring agents and perfumes. c) Sweeting agents. Standards of Tablets The following standards should be maintain during tablet manufacturing: 1) Shape of tablets: In the pharmacopoeia the shape of tablet is defined as circular with flat or convex faces. 2) Appearance: when a broken section of an uncoated tablet is examined under a lens, either a relatively uniform texture or a stratified structure is seen. 3) Content of active ingredient in tablets: the amount of active ingredient in tablet is determined by doing assay as stated in monograph. The result lies within the range for content of active ingredient in monograph. 4) Uniformity of content: it is desirable that every individual tablet in a batch should be uniform in weight but a small variation in the weight of individual tablet is liable to occur. 5) Uniformity of content: tablets must comply with the requirements for uniformity of content specified in individual monograph. Percentage of medicament is calculated by doing assay for a particular drug as per I.P. 6) Disintegration test for tablet: disintegration of a tablet means to break the tablet into smaller particles after swallowing. The time required to disintegrate the tablet is called disintegration time. The rate of disintegration depends upon type of tablet. 7) Dissolution test for tablets: the test is done for measuring the amount of time required for a given percentage of the drug sub. in a tablet to go into solution under specified condition in vivo. 8) Medical strength: the pharmacopoeia has not fixed any standard for mechanical strength or hardness of tablets. 9) Friability test: friability test is performed to evaluate the ability of the tablet to withstand wear and tear in packing, handling and transporting. The apparatus used to perform this test is known as Friabilator. Disintegration test for tablet: Disintegration of a tablet means to break the tablet into smaller particles after swallowing. The time required to disintegrate the tablet is called disintegration time. The rate of disintegration depends upon the type of tablet. The tablet which are dissolved by slow solution in mouth or chewed are to be dissolved in water before administration, do not need a disintegration test. The disintegration test required in tablets which are swallowed. The rate of disintegration differs from tablet to tablet because the nature of drug. In some cases the disintegration time is as short as one minute and in other cases it may be as long as 30 mts. In general, pharmacopoeia prescribed a limited of 15 mts. For most of the tablet unless otherwise indicated in monograph. The disintegration test apparatus as per I.P. specification is used for performing test as shown in figure (1). The apparatus consists of instrumental arrangement as shown in figure. A rigid basket rack assembly supporting six cylindrical glass tubes. These tubes are held vertically by two superimposed transparent plastic plates with six holes having same diameter as tubes. These holes are at an equal distance from the center of plate and are equally spaced from one another woven wire gauze made from stainless steel is attached to underside of lower plate. The upper and lower plates are held in position by vertical metal rods at periphery and metal rod in the center of upper plate for attachment to a mechanical device. The assembly should be raised and lowered betn 28 to 32 times per minute in liquid at 37OC. The tablets are kept immersed in liquid within tubes by means of cylindrical guide discs. The assembly is suspended in liquid medium in a 1000 ml beaker. The beaker may be filled in such a way that the wire mesh at highest point is at least 25 mm below the surface of liquid and its lowest point is at least 25 mm above bottom of beaker. A separate method is used for each type of tablet, the detail of which is given below: 1) Method used for uncoated tablets: place one tablet in each of six tubes of the basket, add a disk to each tube and operate apparatus using water maintained at 37O+- 2OC as the immersion liquid. At end of 15 mts or after time specified in individual monograph. Lift basket from liquid and observe tablets. the tablet pass the test if all size tablet have disintegrated. 2) Method used for coated tablets: Place one tablet in each of the six tubes of basket and tablet has a soluble external coating. Immerse the basket in water at R.T. for 5 min. then add a disc to each tube, suspend the assembly in water maintained at 37O +- 2O and operate apparatus for 60 min. or as indicated in monograph. The tablet pass the test if all six have disintegrated. In any one of the case tablet has not disintegrate, repeat the test on further six tablets replacing water with 0.1 N HCl. The tablets then pass the test if all six tablets have disintegrated in acidic medium. 3) Method used for enteric-coated tablets: place one tablet in each of six tubes of basket. Immerse the basket in water for 5 min. at R.T. in case tablet has a soluble external coating. Operate apparatus without using disk for two hours. The basket is immersed in 0.1 N HCl maintained at 37OC +- 2OC. If no tablet shows signs of disintegration or cracks, then add a disc to each tube and operate apparatus using mixed phosphate buffer having pH 6.8 as immersion liquid at 37O +- 2OC. After 60 min., remove the assembly from liquid and observe the tablets. the tablets pass the test if all six tablets have disintegrated. Capsules Capsules are a solid dosage form in which a drug sub. is enclosed in a water soluble shell or an envelop. A capsule shell is made from gelatin. The capsules are available both as hard and soft capsule. Difference between hard and soft gelatin capsule Hard gelatin capsules 1) The hard gelatin capsule shell consists of two parts viz. body and cap. 2) They are cylindrical in shape. 3) The contents of a hard gelatin capsule usually consists of the medicament or mixture of medicaments in form of powder, beads or granules. 4) These are prepared from gelatin, titanium dioxide, colouring agents and plasticizer. 5) Capsules are sealed after they are filled to ensure that the medicaments may not come out of capsule due to rough handling. Soft gelatin capsules The softgelatin capsule shell becomes a single unit after sealing two halves of capsule. They are available in round, oval and tube like shapes. The contents of soft gelatin capsule usually consists of liquids or solids dissolved or dispersed in suitable excipients to give a paste like consistency. These are prepared from gelatin plasticizer (Glycerin or sorbitol) and a preservative. Filling and sealing of soft gelatin capsules are done in a combined operation on machines. Evaluation of Capsules The following tests should be carried out for evaluation of the capsules. 1) Uniformity of weight: The 20 intact hard gelatin capsules are weighed individually and average wt. per capsule is determined. The capsule passes the test, if each of individual wt. is within 90-110% of average weight. If capsule does not come in this range, then the weight of content of each individual capsule is determined and compared it with average weight of contents. A similar method is followed for soft gelatin capsules. After finding the individual gross wt. of the capsules, the shells are carefully opened by cutting and contens are removed by washing with suitable solvent. After shells have dried, they are weighted and content wt. of indivisual capsule is calculated. 2) Content of active ingredients in capsule: It is applicable to all capsules which are used for oral administration. The assay is done as per the monograph of that drug in the pharmacopoeia. Generally, 20 capsules or such other number as is indicated in the monograph are used in the assay. The result lies within the range of content of the active ingredients stated in the monograph. The requirement of this tablet apply when the stated limits are between 90 and 110 % . 3) Disintegration test for capsules: The apparatus used for disintegration test for capsules is same as that used for disintegration test for the tablets. Place one capsule in each of 6 tubes of the basket and suspend the assembly in water maintained at 37O +- 2O C. Do not use the discs for hard capsules except when the hard capsules float on top of the water, the disc may be added. When testing soft capsules, discs may be used. Operate the apparatus for 30 min. in case of hard capsule and 60 min. in case of soft capsules. The capsule passes the test if no residue remains in form of fragments of the shell. If one or two capsules fail to disintegrate, repeat the test on 12 additional capsules so as NLT 16 of total number of 18 capsules tested get disintegrated. 4) Dissolution test for capsules: The apparatus used for the dissolution test for capsules is same as that used for dissolution test for tablet. Place 1000 ml of H2O free from dissolved air having a temp. of 36.5O to 37.5OC into the vessel. Place the specified number of capsules in dry basket. Assemble the apparatus. Start the motor and adjust its speed to 100 rpm or such other speed as given in monograph. Withdraw the required volume of solution from the vessel after forty five min. or after the period specified in monograph. Filter and determine the amount of active ingredient present by the method given in monograph. Repeat complete operation four times. The sample passes the test if amount of active ingredients in solution is NLT 70 % of stated amount given in the monograph. Test of Alkalinity For Glass The alkalinity tests for glass are as follows: 1) Apomorphine: The hydrochloride of this alkaloid is official and if stabilized by use of water for injections free from dissolved air, sodium metabisulphite and nitrogen filling can be sterilized by autoclave. The sterilized solution may be stored indefinitely if protected from light. However, apomorphine itself is very rapidly oxidized to a green 2) 3) 4) 5) compound and therefore, if a solution of HCl is sterilized in a container yielding more than a trace of alkali the solution will turn green. Atropine: The pH range must favourable for maximum stability of atropine is app. 3 to 4. Above 4.5 the composition is catalyzed by hydroxyl ions. Consequently, storage is high alkali glass which will speed up its destruction and 90 % loss has be reported in an 0.1 % aq. solution for which lime-soda glass was used as container. Morphine: Solution of morphine sulphate develop colour on heating and during storage. This is retarded by acid and accelerated by alkaline pH. Consequently morphine solution must be packed in low-alkali glass. The use of metabisulphide in official injections avoids the use of very low and painful pH which would otherwise be necessary. Polypeptides Insulin: This complex polypeptide is most stable betn pH 2 and 4. It rapidly decomposes when eaction is above 7. Therefore, protection from alkali is necessary. Posterior pituitary Hormones: for maximum stability they must be adjusted to within pH ranges 3 to 4.5 and 3 to 4. It shows that at pH 3 – 4 it lost 10 to 20 % of oxytocic activity during sterilization at 115OC for 30 min. but if pH was 5 about 50 % was destroyed. Although the official injections are no longer sterilized by heating method, alteration of pH in either direction accelerate decomposition on storage and therefore low alkali containers are necessary. Synthetic Base: Adrenaline: This sub. decomposes very easily and it must be protected from alkali because even a slight decrease in its acidity causes a significant loss of potency during sterilization. Vitamins: The stability of many vitamins (e.g. thiamine, ascorbic acid and cyanocobalamine) is greatly reduced in alkaline. Solution and use of containers of low alkalinity is an important means of preserving their activity. Q.C. or Limit of alkalinity for Glass: Because non of the glasses used for pharmaceutical containers is completely free from extractable alkali a test for its absence is impracticable and limit tests must be used. In most pharmacopoeias the quantity of alkali yielded to a specified amount. Ideally, a container should be tested under conditions similar to those it will meet in use but as this would often make the tests inconveniently long extraction is accelerated by a high temp. Two main type of tests are used: 1) Crushed-Glass test: The container is crushed and sieved to produce uniform particles of which a definite weight is taken. Control of particle size and wt. of powder ensures that a constant surface area is exposed to solution. Because all of the glass is examined and extraction is enhanced by rough surfaces of particles, this is a severe test and if a glass passes, it is unlikely that container made from it will give trouble in use. Nevertheless the technique is tedious and is not applicable in surface-treated containers because crushing would expose the alkaline glass below surface. The test may used for determining the nature of the glass or for distinguishing betn two types of glass, such a neutral or surface treated. 2) Whole-container Test: The containers are simply filed with test solution and exposed to test conditions. Because the surface layer of a container is smooth and less reactive than glass beneath, glass ware may pass the whole container test more easily. There car be no serious objection to this, since injection solution are in contact with surface and not deeper layers. But account must be taken of possible diffusion of alkali from latter (e.g. as a result of weathering) during the container’s lifetime. E.g. Container Volume (ml) Inner wetted surface (cm2) 1 5.9 Ampoule 10 29.0 Bottle 1000 511.0 The millittre of test solution a 1 ml ampoule receives the alkali from 1.5 cm2 of surface, in 10 ml ampoule and 1 lit bottle each ml gets the alkali from 2.9 and 0.5 cm2 respectively, i.e. the alkali conc. In small containers will be much greater-about 12 times larger in 1 ml ampoule than in litre bottle. These conditions exist when the containers are in use, the contents of small containers being exposed to more alkali than the contents of large containers, it must be taken into account when setting the limit of extractable alkaline sub. from diff. sized containers. Microbial Limit Test The following tests are designed for the estimation of the number of viable aerobic microorganisms present and for detecting the presence of designated microbial species in pharmaceutical substances. The term growth is used to designate the presence and presumed proliferation of viable micro organisms. Preliminary Testing: The methods given here in are invalid unless it is demonstrated that the specimens to which they are applied do not inhibit the multiplication under the test conditions of microorganisms that can be present. Therefore, prior to doing the tests, inoculate diluted specimens of sub. being examined with separate viable cultures of Escherichia coil, salmonella species, pseudomonas aeruginosa and staphylococcus aureus. This is done by adding 1 ml of NLT 10-3 dilutions of a 24-hr broth culture of micro-organisms to first dilution (in buffer of pH 7.2, fluid soyabean-casein, digest medium or fluid lactose medium) of test material and following test procedure. If organism fails to grow in the relevant medium the procedure should be modified by a) Increasing volume of diluent with quantity of test material remaining the same or b) Incorporating a sufficient quantity of a suitable inactivating agent in diluents or c) Combining the aforementioned modifications so as to permit growth of organisms in media. If inhibitory sub. are present in sample, 0.5 % of soya lecithin and 4 % of polysorbate 20 may be added to culture medium. Alternatively, repeat test as described above, using fluid casein digest-soya lecithin-polysortate 20 medium to demonstrate neutralization of preservatives or other antimicrobial agent in test material. Where inhibitory sub. are contained in product and latter is soluble, the membrane filtration method i.e. total aerobic microbial count may be used. If inspite of incorporation of suitable inactivating agents and a sustaintial increase in volume of diluent it is still not possible to recover viable cultures described above and where the article is not suitable for applying membrane filtration method it can be assumed that the failure to isolate inoculated organism may be due to bactericidal activity of product. This may indicate that article is not likely to be contaminated with given species of micro-organism. However, monitoring should be continued to establish the spectrum of inhibition and bactericidal activity of article. Sterilization: An article would be deemed sterile only when there is complete obsence of viable microorganisms from it. The process of making article sterile is called sterilization. Dry Heat Sterilization: This process of sterilization may be used for heat-stable non-aqueous products and powders. A preparation to be sterilized by dry heat is distributed in final containers which are either finally sealed or temporarily closed to exclude microorganisms, is then heated so as to ensure that entire contents of each container are maintained at 160OC for two hours, unless otherwise stated in individual monograph or at any other equally effective combination of temp. and time. Containers which have been temporarily closed during sterilization procedure, are then finally sealed using technique so as to exclude microorganism. Dry heat sterilization is usually carried out in a sterilizing oven designed specifically for this purpose. The oven may be heated by gas or electricity and is normally provided with a fan or blower to circulate heated air to assure adequate heat distribution throughout the chamber and with suitable temp. recording devices. The sterilizer should be loaded in such a manner as to permit free circulation of heated air throughout chamber. The effectiveness of any dry heat sterilization schedule may be determined under actual working conditions by means of thermocouples or other suitable devices present in representative locations within the load and after proper schedule has been determined. The chamber should be loaded in substantially the same manner for all subsequent cycles in which particular material is to be treated. Suitable biological indicators may be employed to demonstrate effectiveness of the sterilization cycle. Applications The hot air sterilizer is used for sterilizing all kinds of glassware such as test tubes, pipettes, pitridishes and flasks. In addition, it may be used to treat other laboratory materials, instruments and equipment which are not burned or injured by high temp. of the sterilizer. Mechanism: Irreparable degradations of essential cell constituents such as enzymes and other proteins by oxidation are most probable mechanism of dry heat sterilization. General Requirements for Parenteral Dosage Forms: The formulation of parenteral products involve careful consideration of following requirements. 1) Stability: The stability of parenteral preparation is very important. The physical as well as chemical stability of parenteral preparation must be maintained during storage. 2) Sterility: The parenteral preparations should be free from all types of micro-organisms. An aseptic conditions are required to be maintained during the preparation of parenteral products and it’s administration. The parenteral product must pass the test for sterility. 3) Free from pyrogens: The parenteral preparations should be free from toxin and pyrogens. It is necessary that parenteral products must pass the test for pyrogen, because contaminated parenteral product cause a rise in body temp. after its administration. 4) Free from foreign particles: The parenteral products should be free from foreign particles such as dust and fibers. To ensure this the parenteral product must pass clarity test. 5) Isotonicity: The parenteral preparations should be isotonic with blood plasma and body fluids. It is very important, in order to avoid any complications on administration of parenteral products. 6) Specific gravity: The parenteral products meant for intra-spinal injections should have same specific gravity as that of spinal fluid into which same are to be injected. 7) Chemical purity: The parenteral products should be free from chemical impurities or it should be within certain limit as specified in monograph of that preparation n pharmacopoeia. Test for Pyrogens: Unless otherwise stated in individual monograph when the volume to be injected in a single dose is 10 ml or more. Injections comply with test for pyrogens unless the test for bacterial endotoxins is prescribed. Test for pyrogens involves measurement of rise in body temp. of rabbits following the i.v. injection in marginal rein of ear of sterile solution of the sub. being examined. It is designed for products that can be tolerated by test rabbit in a does not exceeding 10 ml per kg injected intravenously with in a period of not more than 10 min. Before the main test a ‘’ preliminary test (sham Test) is performed by injecting pyrogen free saline solution to acclimatized the animal with testing. Any animal showing a temp. variation of 0.6O C or more must not use in main test. The rectal temp. is recorded as prescribed with the help of theromoreted or thermocouple. The main test is performed using three rabbits which are acclimatized through sham test. If sum of the responses of group of three rabbits does not exceed 1.4OC and if response of any individual rabbit is less than 0.6OC, the preparation being examined passes the test. If the response of any rabbit is 0.6OC or more, or if sum of responses of three rabbits exceeds 1.4OC, continue test using five other rabbits. If not more than three of eight rabbits show individual response of 0.6OC or more and if sum of responses of group of eight rabbits does not exceed 3.7OC, the preparation being examined passes the test. At present an in vitro test for pyrogen is developed which is known as LAL-Test (Limulus Amoebocyle Lysate Test) and much more sensitive than rabbit test. This lysate is used in BACTERIAL ENDO TOXINS TEST as prescribed by I.P. The bacterial endotoxins test (BET) measure the conc. Of bacterial endotoxins that may be present in or on the sample of article to which test is applied using a lysate derived from hemolymph cell or amoebocytes from horse shoe crab, Limulus polephemus. The addition of a solution containing endo-toxin to a solution of lysate produces turbidity, ppt. or gelation of mixture. The rate of reaction depends on conc. Of endotoxin, pH and temp. Powders Pharmaceutical powders are solid dosage forms which consists of mixture of dry powder drugs intended for internal or external use. Merits: 1) 2) 3) 4) They can be made easily because no complicated machinery is required. They disintegrate quickly in stomach. The drug can be easily dispensed in cachets. Large doses of drug can be swallowed by using cachets, because once they get soften by immersion in water, even large sized cachets can be swallowed readily. Demerits: 1) 2) 3) 4) They must be softened before swallowing. They are easily damaged. They can not protect the enclosed drug from light and moisture. They are not compressed in cachets. Quality Control Good Manufacturing Practice: Definition: Good manufacturing practice (GMP) is that part of quality assurance which ensure that products are consistently produced and controlled to quality standards appropriate to their intended use and as required by the marketing authorization (as per WHO). GMP is that part of quality assurance which insures that products are consistently produced and controlled to quality standards appropriate for their intended use and legal requirements. GMP is thus concerned with both production and quality control matters ( as per MCC S.A.) Comments: i) ii) iii) iv) v) GMP is part of Q.A. GMP’s main function is to produce quality products consistently. GMP must meet legal requirements of country. For meeting the expected requirements, GMP must deal with both production and Q.C. related issues. The main function of GMP is to diminish the risk of mixups and contamination. Components of GMP: The total activity of GMP can be summarized in following points: a) All manufacturing processes should be clearly defined:- all manufacturing process should be systematically reviewed in light of experience and shown to be capable of consistently manufacturing pharmaceutical products of required quality that comply with their specifications. b) Critical steps of manufacturing process and any significant changes made to the process validated. c) All necessary facilities are provided including: i) Appropriately qualified and trained personnel in sufficient no. ii) Adequate permises and space. iii) Suitable equipment and services. iv) Correct materials, containers and label. v) Adequate personnel, laboratories and equipment in IPQC under the responsibility of production management. d) Instruction and procedures are written in clear and unambiguous language, specifically applicable to facilities provided. e) Operators are trained to carry out procedures correctly. f) Records are made during mtg. to show that all steps required by defined procedures and instructions have infact been taken and at quantity and quality of product are as expected and significant deviations are fully recorded and investigated. g) The proper storage and distribution of product minimizes any risk of their quality. Documentation in quality control laboratory: Quality Control Q.C. is the part of GMP concerned with sampling, specification and testing and with the organization, documentation and release procedure which ensure that necessary and relevant tests are actually carried out and that material are not released for use, nor products released for sale or supply, until their quality has been satisfactory. Q.C. is not confined to laboratory operations but must be involved in all decisions concerning quality of product (as per WHO). Q.C. is that part of GMP which is concerned with organization, documentation and release procedures which ensure that necessary and relevant tests are actually carried out that material are not released for use, nor products released for sale or supply, until their quality has been judged to be satisfactory. The documentation required for different Q.C. are as: 1) For other activities of Q.C.a) Responsibilities of Q.C. department. b) Job description of Q.C. head. 2) Sampling of finished bulk and packed finished products. a) SOP/R on sampling of – R.M. , P.M., I.P., Q.C. material, finished bulk products, finished packed product. 3) Testing a) SOP/R on calibration and validation for all analytical instrument. b) List of all major analytical instruments. c) Lists of chemicals / reagents / media used. d) Lists of glass wares. e) Lists of books related to chemical and other analysis. f) List of technical staffin Q.C. lab. g) Lists of specification for R.M/P.M./F.G. h) SOP/R on reference / related samples. i) SOP/R on assestment of finished product. j) Standard test procedures. k) Records of analysis. l) SOP/R on ref. and working std. m) SOP/R on handling of reagents / media, etc. n) SOP/R on management of animal house. o) SOP/R on sampling and testing of IPQC materials. p) SOP/R on testing and release of sterile products. Stability Studies Pathways of drug degradation: 1) Introduction: a) Chemical degradation of active ingredient can cause substantial loss of active ingredient from dosage form. b) Chemical degradation can produce a toxic product that has undesirable side effects. 2) Rates and orders of radiation: a) Degradation rate is the velocity with which the reaction occurs. This rate is expressed as dc/dt (rete of change of conc. with time). b) The order of a reaction is the way in which conc. Of drug or reactant in a chemical reaction affects rate. The rate of reaction, dc / dt is proportional to conc. Of n th power. Where, n is the order of reaction. dc / dt Cn the above equation shows that the conc. of drug degrade with time. 3) Factors affecting reaction rates: Factors other than conc. can affect reaction rate and stability of drug. These factors are: a) Temp. An increase in temp. causes an increase in reaction rate. Hence, drugs degradated faster. b) Presence of solvent: Many dosage form require the incorporation of a water miscible soluents to stabilize drug. The change in solvent indirectly affect reaction rate. c) Change in pH: The magnitude of rate of a hydrolytic reaction catalyzed by H+ and OH- can vary considerably with pH. d) Presence of additives: Buffers salt must be added to many drug solution to maintain formulation to optimum pH. These salts can affect rate of degradation. 4) Methods of pharmaceutical degration: The decomposition of active ingredients in a dosage form occurs through several path ways. a) Hydrolysis: It is the most common type of degradation because many medicinal compounds are ester, amides or lactams. i) H+ and OH- are the most common catalysts of hydrolytic degradation in solution. ii) Esters usually undergo hydrolytic reactions that cause instability. Because esters are rapidly degraded in aq. solution. Formulators are reluctant to incorporate drugs that have ester function groups into liquid dosage forms. b) Oxidation: It is usually medicated through reaction with atmospheric oxygen under ambient conditions. i) Medical compounds in solvent and in lead space of their packages. Thje compounds should be packed in an inert atmosphere to exclude air from their containers. ii) Most oxidation reaction involve a free radical mechanism and chain reaction. Antioxidant in formulation react with free radicals by providing electrons and easily available hydrogen atoms. In this way they present the propagation of chain reaction. c) Photolysis: it is the degradation of drug molecules by normal sunlight at room light. i) Molecules may absorb the proper wavelength of light and acquire sufficient energy to undergo reaction. Usually, photolytic degradation occurs on exposure of light of were lengths less than 400 nm. ii) An amber glass bottle or an opaque container acts as a barrier to this light, thereby preventing or retarding photolysis. Shelf Life: The shelf life of an drug preparation is the amount of time that the product can be stored before it becomes unfit for use, through either chemical decomposition or physical deterioration. Determination of shelf life: 1) Storage temp: It affects shelf life. It is generally understood to be ambient temp. unless special storage conditions are specified. 2) In general, a preparation is considered fit for use if it varies from the nominal conc. or dose by no more than 10 % , provided that the decomposition products are not more toxic or harmful than original material. 3) Shelf life testing aids in determining the standard shelf life of a formulation. a) Samples are stored at app. 3 – 5 OC and at R-T (20-25OC). the samples are then analyzed at various intervals to determine rate of decomposition. Shelf life is calculated from this rate. b) Because storage time at these temp. can result in an extended testing time, accelerating testing is conducted as well, with a range of higher temp. the rate constant obtained from these samples are used to predict shelf life at ambsent are refrigeration temp. Temp.- accelerated stability testing is not useful if temp. changes are accompanied by changes in reaction mechanism or by physical changes in system. c) Stability at R.T. can be predicted from accelerating testing data by Aorehenius equation. 𝐾𝑇2 𝐸𝑎 (𝑇2 − 𝑇1 ) log ( )= 𝐾𝑇1 2.303 𝑅 (𝑇2 𝑋𝑇1 ) Where, KT2 and KT1 are rate constant at absolute temp. t2 and T1 respectively. R = molar gas constant. Ea = Energy of activation. d) Alternatively, an expression of conc. can be platted as linear function of time. Rate constants (k) for degradation at several temp. are obtained. The log of rate constant (log K) is plotted against reciprocal of absolute temp. (1/T). to obtain, the rate constant for degradation at R.T. k, hous-1 X 10 3 yT X 10 3 e) The length of time that the drug will maintained it’s required potency can also be predicted by calculation of 90 % . this method applies to chemical reactions with activation energies of 10 – 30 kcal/mole, the magnitude of activation energy for many pharmaceutical degradations that occur in solution.