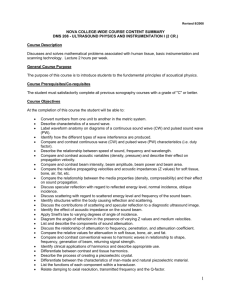
Biomedical Imaging I

Ultrasound
Sound waves
Sounds are mechanical disturbances that propagate through the medium
Frequencies <15Hz Infrasound
15Hz<Frequencies <20KHz Audible sound
Frequencies>20Khz Ultrasound
Medical Ultrasound frequency 2 -20MHz
Some experimental devices at 50MHz
Velocity and frequency
For sound waves the relationship between frequency/velocity and wavelength is c = f x
Speed of sound depends on the material sound travels
Velocity is inversely proportional to compressibility the less compressible a material is the greater the velocity
Average velocity in tissue 1540 m/sec (air 331m/sec, fat 1450 m/sec)
The difference in speed of sound at the boundaries determines the contrast in US
Wave Speed
c air
= 331 m/s c salt water
= 1500 m/s c
B
B = Bulk Modulus
= density
Bulk modulus measures stiffness of a medium and its resistance to being compressed
Speed of sound increases with stiffness of material k = adiabatic bulk modulus
= density
Wave speed cnt
Changes in speed DO NOT affect the frequency so only the wavelength is dependent on the material.
What is the wavelength of a 2MHz beam traveling into tissue?
What is the wavelength of a 5MHz beam traveling into tissue?
Wave speed cnt
Changes in speed DO NOT affect the frequency so only the wavelength is dependent on the material.
What is the wavelength of a 2MHz beam traveling into tissue? 0.77mm
What is the wavelength of a 10MHz beam traveling into tissue? 0.15mm
The wavelength determines the image resolution
Higher frequency -> higher resolution
Penetration is higher at smaller frequencies.
Penetration and resolution
Thick body parts (abdomen)
Low frequency ultrasound (3.5 - 5 Mhz)
Small body parts (thyroid, breat)
High frequency (7.5 - 10 Mhz)
Interference
Waves can constructively and destructively interfere
Constructive interference -> Increase in amplitude (waves in phase)
Destructive interference -> Null amplitude (waves out of phase)
Acoustic Impedance
Z=
x c [kg/m 2 /sec] SI unit ([Rayl] =1 [kg/m 2 /sec])
Independent of frequency
Air -> Low Z
Bone -> High Z
Large difference in acoustic impedence in the body generate large reflections that translate in large US signals
Example going from soft tissue to air filled lunghs ->BIG REFLECTION
Sound and pressure
Sound waves cause a change in local pressure in the media
Pressure (Pascal)=N/m 2
Atmospheric pressure 100KPa
US will deliver 1 Mpa
Intensity I (amount of energy per unit time and area) is proportional to P 2
This is the energy associated with the sound beam
Temporal and Spatial intensity when dealing with time or space
Sound and pressure
Relative sound intensity (dB) (Bels => B, 1B=10dB)
Relative intensity dB= 10 log( I/Io ) Io original intensity, and I measured intensity
Negative dB -> signal attenuation
-3dB -> signal attenuated of 50%
Attenuation
Loss by scatter or absorption
High frequency are attenuated more than low frequencies
Attenuation in homegeneous tissue is exponential
A 1Mhz attenuation in soft tissue is 1 dB/cm, 5 MHz -> 5dB/cm
Bone media attenuation increases as frequency squared.
Absorbed sound ->heat
Reflection
Echo -> reflection of the sound beam
The percentage of US reflected depends on angle of incidence and Z
Similar to light
R
Z
Z
2
2
Z
1
Z
1
2
T
4
Z
1
Z
2
Z
1
Z
2
2
Reflection Snell’s Law
i
t angle of incidence angle of transmittance
sin sin
i
v
1 v
2
Transducer
Made of piezoelectric material
Crystals or ceramics
Stretching and compressing it generate V
Lead-zirconate-titanate (PZT)
A high frequency voltage applied to PZT generate high freq pressure waves
Are generators and detectors
Q factor
Q factor is the frequency response of the piezoelectric crystal
Determines purity of sound and for how long it will persist
High Q transducers generate pure frequency spectrum (1 frequency)
Q=operating frequency/BW
BW bandwidth
High Q -> narrow BW
Low Q->broad BW
Transducer backing
Backing of transducer with impedance-matched, absorbing material reduces reflections from back
damping of resonance
Reduces efficiency
Increases Bandwidth (lowers Q)
Axial beam profile
Piston source: Oscillations of axial pressure in near-field
(e.g. z
0
= (1 mm) 2 /0.3mm = 3 mm)
Near Field
Fresnel Zone
Far Field
Fraunhofer zone
Caused by superposition of point wave sources across transducer (Huygens’ principle)
Side lobes = small beams of reduced intensity at an angle to the main beam sin(
)
1.22
/(2 r ) z
0
r
2
4
US usually uses
Fresnel Zone
Lateral beam profile
Determined by Fraunhofer diffraction in the far field.
Given by Fourier Transform of the aperture function
Lateral resolution is defined by width of first lobe (angle of fist zero) in diffraction pattern
For slit (width a ):
I
I
0
sinc
Minima at: sin a
sin
n
a
For disc (radius r , piston source): sin
0.61
r
arcsin 0.61
r
Focused transducers
Reduce beam width
Concentrate beam intensity, increasing penetration and image quality
All diagnostic transducers are focused
Focal zone – Region where beam is focused
Focal length – distance from the transducer and center focal zone
Focusing of ultrasound
Increased spatial resolution at specific depth
Self-focusing radiator or acoustic lens
Array types
a) Linear Sequential
(switched) ~1 cm
10-15 cm, up to 512 elements b) Curvilinear similar to (a), wider field of view c) Linear Phased up to 128 elements, small footprint
cardiac imaging d) 1.5D Array
3-9 elements in elevation allow for focusing e) 2D Phased
Focusing, steering in both dimensions
Array resolution
Lateral resolution determined by width of main (w) lobe according to sin
w
Larger array dimension
increased resolution
Side lobes (“grating lobes”) reduce resolution and appear at sin
g n
g n
1, 2,3,...
a g w
Ultrasound Imaging
Imaging
Most ultrasound beam are brief pulses of 1 microsecond
Wait time for returning echo
Object must be large compared to wavelength
Signal is amplified when returned (echo is small signal)
A-mode (amplitude mode) I
Oldest, simplest type
Display of the envelope of pulse-echoes vs. time, depth d = ct /2
Pulse repetition rate ~ kHz
(limited by penetration depth, c
1.5 mm/
s
20 cm
270
s, plus additional wait time for reverberation and echoes)
A-mode (amplitude mode)
Or space! Also M mode!
depth
A-mode II
Frequencies: 2-5 MHz for abdominal, cardiac, brain; 5-15 MHz for ophthalmology, pediatrics, peripheral blood vessels
Applications: ophthalmology (eye length, tumors), localization of brain midline, liver cirrhosis, myocardium infarction
Logarithmic compression of echo amplitude
(dynamic range of 70-80 dB)
Logarithmic compression of signals
M mode or T-M mode
Time on horizontal axis and depth on vertical axis
Time dependent motion
Used to study rapid movement – cardiac valve motion
B-mode clinical example
Static image of section of tissue
Brighter means intensity of echo
Bmode (“brightness mode”)
Lateral scan across tissue surface
Grayscale representation of echo amplitude
Add sense of direction to information-> where did echo come from
Real-time B scanners
Frame rate R f
~30 Hz: t acq
2 c d
N R f
t
1 c
2 d N d : depth
N : no. of lines
Mechanical scan: Rocking or rotating transducer
+ no side lobes
- mechanical action, motion artifacts
Linear switched array
Linear switched
CW Doppler
Doppler shift in detected frequency f shift
c
f v : blood flow velocity c: speed of sound
: angle between direction of blood flow and US beam
Separate transmitter and receiver
Bandpass- filtering of Doppler signal:
Clutter (Doppler signal from slow-moving tissue, mainly vessel walls) @ f<1 kHz
LF (1/f) noise
Blood flow signal @f < 15 kHz
CW Doppler bears no depth information
Frequency
Counter
Spectrum
Analyzer
CW Doppler clinical images
CW ultrasonic flowmeter measurement (radial artery) v
[10cm/s] t
[0.2 s]
Spectrasonogram:
Time-variation of Doppler Spectrum f t
CW Doppler example
Duplex Imaging
Combines real-time B-scan with US Doppler flowmetry
B-Scan: linear or sector
Doppler: C.W. or pulsed ( f c
= 2-5 MHz)
Duplex Mode:
Interlaced B-scan and color encoded Doppler images
limits acquisition rate to 2 kHz (freezing of B-scan image possible)
Variation of depth window (delay) allows 2D mapping (4-18 pulses per volume)
Duplex imaging example (c.w.)
www.medical.philips.com