Breast Ultrasonography. An Introduction Part 2
advertisement

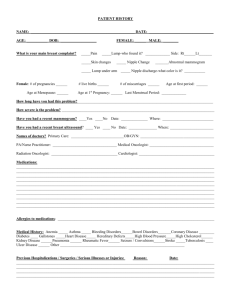
Ultrasound of The Breast Part 2 Holdorf PhD, MPA, RDMS (Ob/Gyn, Ab), RVT, LRT(AS) Instrumentation Breast Sonography is extremely operator-dependent. Therefore, it is essential to use appropriate equipment and be properly schooled in breast Sonography in order to achieve diagnostic accuracy. Sonographic images are created using the B-Mode (brightness) principle. This offers a gray scale image of the breast. The set-up of the ultrasound system (machine) should include selecting the most appropriate transducer and optimizing the depth, overall gain, TGC, output power, focus, and gray scale. Color and power Doppler techniques continue to play a useful role in breast imaging and also require fine adjustment. Transducers Transducer selection is critical in breast imaging. Frequency A 10.0 – 18.0 MHz frequency is optimal Need high frequency probe for superior axial and lateral resolution (detail) while maintaining penetration to chest wall. A broadband transducer (wide frequency range) is optimal. Trade-off; High frequency probes yield superior image detail while losing penetration ability. Low frequency probes penetrate deeper but lose image detail. Probe Design A linear Array transducer is optimal. Produces a rectangular image Allows direct contact scanning perpendicular to the chest wall. Accurate measurements can be recorded by avoiding beam divergence artifact (this is achieved with a rectangular image vs. a sector image). Interventional procedures (i.e., cyst aspiration, biopsy, and needle localization, etc.) can be accurately guided with a linear array probe. A curved Array transducer may be used to supplement the sonographic examination if a mass is too large to fit on a linear image. Using the lower frequency curved array probe provides a larger field of view at the expense of lost resolution. Depth Depth should be sufficient to visualize the breast tissue from skin to chest wall. Breast size will vary from one patient to the next. However, an imaging depth between 3 and 6 cm should be adequate. Imaging of the breast should include 1. skin 2. breast parenchyma 3. pectoral muscle 4. chest wall Gain Receiver gain is the amount of amplification applied to a returning echo. An echo’s brightness is controlled by gain. Gain is the most frequently adjusted control. It is optimized for each patient depending on several factors. These factors include breast size, thickness, and tissue density. There are typically three adjustments for gain on the ultrasound control panel: 1. Overall Gain 2. TGC 3. Auto Gain Optimization OVERALL GAIN Controls the level of brightness of all echoes appearing on the image. The Sonographer has the ability to increase or decrease the overall brightness by using this control. TGC (Time Gain Compensation) Allows for brightness to be controlled at varying depths throughout the image. The top control adjusts brightness in the near field of the image. The bottom controls adjust brightness in the far field. Output Power Output power is the amount of voltage applied to the transducer to create a sound wave. This control determines the patient’s exposure to ultrasound energy. Therefore, the sonogphaer should consider prudent use of output power. All state-of-the-art sonographic systems, however, function at a safe power setting while operating at 100% output power. Sonographers should remember the ALARA principle: Output power should be set “As low as reasonably achievable.” Focus Multi-focus or variable (Adjustable) electronic focusing will achieve optimal breast detail. The use of multiple focal zones will provide excellent resolution of full depth of the image. This may significantly reduce the frame rate. Multiple focal zones, however, are still recommended. Trade-off: Multiple focal zones will yield the best resolution throughout the entire image at the expense of a slow frame rate. Increased focal zones = decreased frame rate. Multiple focal zones Single focal zone (single focus) Gray Scale Echoes returning from breast tissue are assigned to a specific shade of gray based on their echo strength. This function of the ultrasound system is known as Gray Scale Mapping or Dynamic Range. The sonographer controls the selection of the gray scale map or dynamic range by using the breast or small part examination preset or protocol control. Fine adjustments to the dynamic range may also be made during scanning. Generally for Breast imaging, a broad gray scale map or dynamic range is used. This provides a wide range of gray shades to be displayed while demonstrating subtle tissue differences. A map with too few gray shades may not accurately demonstrate low-level echoes within a cyst or solid lesion. Artifacts Artifacts exist in breast sonography as they do imaging any other organ structure. Some artifacts have proven helpful and may aid in determining certain characteristics about tissue. Artifacts also hinder imaging capabilities. Helpful artifacts Acoustic enhancement – Generally associated with a cystic/benign lesion. Shadowing – generally associated with a solid/malignant lesion. Shadowing artifact with breast cancer Unwanted artifacts Reverberation – artifactual linear echoes parallel to a strong interface. Has a distinct “stepladder” or “venetian blind” appearance. Side or Grating lobe – Secondary sound sources off the main sound beam that place artifactual echoes within a cyst. Slice (section) Thickness – Unwanted echoes from the thickness of the sound beam in the elevation plane that place artifacts within a cyst. Nipple Shadowing – shadowing in the subareolar region may be eliminated by angling the transducer posterior to the nipple or by using the “rolled nipple” technique. Volume Averaging – decreases contrast resolution and spatial resolution (both axial and lateral). Places unwanted echoes in cysts. Doppler is helpful in distinguishing: Solid vs. Cystic – Positive flow within a lesion confirms a solid nature. Inflamed vs. non-inflamed tissue- Doppler signal will increase due to increased flow to an inflammation. Complicated Cyst vs. complex cyst – vs. intraductal papilloma – Doppler signal will be absent in the debris of a complicated cyst but may be evident within the solid component of a complex cyst or intraductal papilloma. PRESSURE: Minimal transducer pressure should be used with Doppler scanning techniques of the breast. The small vessels within the breast tissue are easily compressed. Doppler technique: In order to optimize Doppler imaging, the sonographer should establish a technique for low velocity flow states: This includes 1. Low velocity Scale 2. Low filter setting 3. Optimal Doppler Gain Setting 4. Increased PRF for high flow velocities. Solid or Cystic? Conventional color Doppler reveals solid mass Elastography Elastography is a diagnostic method that evaluates the elastic properties of tissue. Breast tissues and masses vibrate or compress differently based on their firmness. It is well known that breast fat is highly elastic and compresses significantly. It is also known that benign lesions tend to be soft (compressible) and malignant lesions tend to be hard (very firm and non-compressible. Therefore, elastography may have the potential to differentiate benign from malignant breast tumors (distinguish BIRADS 3 form BIRADS 4 lesions) and potentially reduce the number of biopsies. Skin The skin is composed of the epidermis and dermis layers The thickness is 0.5 to 2 mm It is slightly thicker in young females and thins with age. NIPPLE Consists of dense connective tissue and erectile muscle. It contains many sensory nerve endings. 15 to 20 collecting (lactiferous) duct openings may be seen (each of which arise from a breast lobe) AREOLA Circular area of dark pigmentation seen around the nipple. Consists of smooth muscle. Slightly thicker than surrounding skin. Contains Montgomery glands- sebaceous glands seen as small bumps in the areola. 1. Subcutaneous (Premammary Layer) 2. Superficial layer 3. Deep layer 4. Superficial fascia 5. Mammary Layer Subcutaneous (Premammary ) Layer Lies just beneath the skin extending to the mammary layer Consists primarily of fat It is not seen posterior to the nipple Amount of fat increases with age, pregnancy, and obesity Cooper’s ligaments appear as prominent structures within the subcutaneous layer. Standard Anatomic Reference Quadrant Method Each breast can be divided into quadrants (4): UO – Upper Outer UI – Upper Inner LO- Lower Outer LI – Lower Inner Glandular tissue is usually thicker in the Upper-Outer quadrant of both breasts Therefore, a larger percentage of cancers are found there. Clock method Regions of the breast are correlated with positions of a clock. This method allows a more precise location to be documented. Correlating clock locations from right to left side is important in evaluating the breast for symmetry. For example, the 10:00 position in the right breast correlates with the 2:00 position on the left. Development Anomalies Amastia- absence of one or both breasts Polymastia – accessory breast or more than two breasts. Athelia- absence of the nipple. Polythelia – accessory nipple (most common breast anomaly). Amazia- absence of the breast tissue with development of the nipple. Nipple flattening or Nipple inversion. Unilateral early ripening – asymmetric growth of the breasts. Polythelia is more common in men than in women. Intra-mammary Lymph Node Approximately 75% of lymphatic drainage is to the axilla. Therefore, the axillary lymph node chain becomes extremely important in predicting the spread of breast cancer. The axillary lymph node chain consists of 6 groups of nodes: 1. External mammary group-located along the lateral thoracic vessels. 2. Scapular group-run with the subscapular vessels. 3. Axillary group- run with the axillary vessels. 4. Central group – run with the axillary vessels 5. Subclavicular group – run with the subclavian vessels. 6.Interpectoral (Rotter’s) nodes – found between pectoralis major and minor muscles. Lymph nodes of the axillary region Mature female breast The mature female breast is sensitive to the menstrual cycle and responds to fluctuating hormone levels every month. Early in the proliferative phase of the menstrual cycle, changes in the epithelium occur. Later in the secretory phase, the ducts and veins increase in size, the stroma becomes edematous, and the epithelium produces secretions. These changes may account for premenstrual breast discomfort. At the onset of menses, the breast tissues decrease in size. Pregnancy During pregnancy, there is considerable change in the breast tissue. The TDLUs increase in size as the epithelium begins to swell. The acinar cells enlarge in response to a variety of hormones including estrogen and progesterone, and lactogen, prolactin, and chorionic gonadrotrophin from the placenta. Late in the pregnancy, the lactiferous ducts increase in size. Cartoons of Shapes Sonography Breast Sonography Sonography has been shown to be highly valuable in the diagnosis and management of breast disease. The use of breast sonography as a screening tool for breast cancer, especially for younger patients, continues to gain popularity. Using sonography as a screening tool for all patients is highly debated. There are several approaches for using Breast Sonography or Breast Ultrasound (BUS) in the diagnosis of disease: Targeted Examination and Whole Breast Examination. Targeted Exam Sonography is used to evaluate a specific area of breast only. Usually performed as a follow-up to mammography. The entire breast and opposite breast are not evaluated. Whole Breast Exam Sonography is used to survey the entire breast for the presence of disease, often with attention to a specific area. Sonography also plays a crucial role in the management of breast disease. Real-time visualization of the needle’s path using 2D or 3D/4D technique allows sonography to guide interventional procedures. Indications for Breast Sonography Characterize masses as cystic or solid Follow-up to Mammography Evaluate palpable masses in young women (less than 30) avoiding mammography. Evaluate masses in pregnant and lactating women. Evaluate dense breast tissue Evaluate a mass seen in only one view on mammography Evaluate inflammation Evaluate the irradiated breast Evaluate the augmented breast Evaluate axillary lymph nodes Evaluate nipple discharge Evaluate patients when mammography is not possible Serial evaluation of a benign mass Evaluate the male breast Guide interventional procedures Patient History The sonographic examination begins with a through patient history. Sonographers should use a questioning technique to obtain as much personal history that the patient can provide. Patient history should include: Patient’s name Personal history of breast disease Personal history of cancer Family history of breast disease Medications: especially hormones Previous breast surgeries and findings Breast pain and location Findings from monthly breast self-examinations (BSE) Findings from clinical breast examination (CBE) The sonographer should also make a visual inspection of the breast for: Size, shape, contour, and symmetry Skin redness, edema, dimpling or retraction, protrusions, and thickening. Nipple retraction and discharge Surgical scars If palpable lump is noted, the sonographer should document: Location Size Shape (round, oval, lobulated, or irregular) Consistency of lump (soft, rubbery, firm, hard, gritty) Mobility (movable or fixed) Distanced from the nipple Date when it was first discovered and has it changed over time. If a previous Mammogram or BUS has been performed, the prior examination should be reviewed by the sonographer for comparison. It is essential that size, shape, and density/echogenicity of a mass are consistent from one exam to the next. Skin dimpling Positioning The patient is examined in a supine or supine-oblique position with the ipsilateral (same) arm raised above the head. A sponge or pillow may be used to support the patient’s back. This maneuver allows a more even distribution of the breast tissue over the chest wall with the nipple centered. The thickness of the breast is minimized and allows adequate penetration by the sound beam. This is also identical to the position used during open excisional biopsies. The right breast is best evaluated with the patient in the LPO (left posterior oblique) position. The left breast is best evaluated in the RPO (right posterior oblique) position. The medial aspect of the breast is effectively evaluated with the patient lying in the supine position. For larger breasted patients, lateral lesions may require a steep oblique or decubitus position. A sitting or upright position may be used as an alternative patient position to simulate the cranio-caudal (CC) mammographic view. Transducer Pressure Moderate transducer pressure should be applied during scanning. This will: Improve sound transmission Improve detail or resolution Decrease the tissue depth for better penetration May eliminate some artifacts Scan Planes Sagittal and transverse scan planes may be used in breast imaging. Sagittal and transverse scan planes correspond to conventional sagittal and transverse to the body. Radial and Anti-radial scan planes may also be used. Radial and Anti-radial scan planes correlate with the direction of the ductal system of the breast. Radial is longitudinal or parallel with the ducts and anti-radial is transverse or perpendicular to the ducts. Radial is the AIUM recommended scan plane for breast imaging. Important note: If a solid lesion is found, the sonographer should scan the lesion in the radial and anti-radial planes. This allows visualization of tumor or ductal extensions branching toward or toward the nipple. These extensions could be missed in the sagittal and transverse planes. Annotation Labeling your images can be very time consuming, yet very helpful for precise location of a lesion and followup studies. Most sonography departments use the standard clock method for identifying the location of lesions. This provides a more detailed description than the quadrant method. SA may denote the subareolar region, and AX may refer to the axillary region. In addition to the clock method, some Sonographers also use the 123 and ABC methods of providing more exact location. 123 Method The 123 method describes the location of a lesion in comparison to its distance from the nipple. Location 1 is near the nipple. Location 2 is mid distance from the nipple. Location 3 is in the periphery of the breast. 123 Method ABC Method The ABC method describes the depth of a lesion. Location A is superficial Location B is at mid depth (likely within the mammary layer) Location C is near the chest wall. Stand-off Pad A stand-off pad creates distance between the face of the probe and the skin surface. Therefore, the fixed elevation plane focus is moved more superficially. This allows improved focusing and greater detail in the superficial layers of the breast. A stand-off pad improves imaging of: Superficial tumors of cysts Superficial vessels Superficial ducts Skin lesions Skin thickening Scanning surgical specimens Types of Stand-off Techniques include: Commercially produced gel pads Water bag Large “glob” of gel (used for imaging the nipple) Stand-off transducer attachments The ideal stand-off pad thickness for breast imaging is 1cm This places the elevation plane focus of a 10MHz transducer at approximately 0.5cm depth within the breast. Normal Sonographic Appearance The echogenicity of breast tissue will vary with the amount and location of fat and fibrous tissue due to patient age, functional state of the breasts, and body habitus. For example, young women will tend to have more dense fibroglandular tissue that appears HYPERECHOIC. Older women tend to have more fatty replacement that appears ISOECHOIC. The lactating patient will have greater density appearing HYPERECHOIC. The obese patient will have more fat appearing ISOECHOIC and the extremely thin patient will appear to have more dense tissue appearing HYPERECHOIC. The breast is composed of three major tissue types seen on sonography: Fat (superficial, intraparenchymal, and retromammary) Epithelium (TDLU and Acini) Stromal Tissue Loose stromal tissue (intralobular and periductal) Dense stromal tissue (interlobular and Cooper’s ligaments. Echogenicity Skin - HYPERECHOIC Thickness of 0.5 to 2mm. May see slight increase in echogenicity at the gel/skin interface (sound beam entrance) and the skin/superficial fat interface (exit). Fat – MEDIUM GRAY Found within the superficial layer, parenchymal layer, and retromammary layer. All structures are compared to the mid-level echogenicity of fat. Cooper’s Ligaments – HYPERECHOIC Considered part of the dense connective tissue. Best seen in the subcutaneous fat layer as a thin, wavy linear structure. May produce shadowing artifact- try changing the angle of the transducer. Sonographic Features of Benign Disease Shape and orientation Round Characteristic of tense cysts and small, solid, benign tumors Oval or Ellipsoid Typical of non-tense cysts and most benign tumors Horizontal orientation Also known as WIDER-THAN TALL, Length > AP, or Width > Depth Long axis of the tumor is parallel to chest wall Benign tumors tend to grow within or along the tissue plane (not crossing) Margins Smooth, well-defined, or circumscribed Indicates the tumor is displacing adjacent tissues rather than invading Macrolobulation Gentle, large lobulations Border Thickness Thin, echogenic pseudocapsule Caused by compression or rimming of adjacent tissues around the lesion (Opposite of Invasion) Echogenicity Anechoic Simple cyst Hyperechoic Indicates a fibroglandular pseudomass or lipoma Mildly hypoechoic, isoechoic, or mildly hyperechoic Solid, benign tumors Contradiction: some malignant tumors have same echogenicity Homogeneous Internal echoes are a consistent, single shade of gray Contradiction: some highly cellular malignant lesions may appear homogeneous Artifacts Acoustic Enhancement Caused by an increase in sound energy while passing through tissue Most are cysts Solid, benign tumors may also display enhancement. This is due to more uniform travel through the tumor than through the surrounding tissue Enhancement artifact offers good visualization of the posterior tumor wall. Contradiction: some highly cellular malignant tumors may have A.E. Edge Shadowing Attenuation of the sound beam at the lateral margins of a mass due to refraction. Doppler Cysts have no internal flow Benign, solid masses demonstrate no flow or are hypovascular (little Doppler signal) Fibrous Planes Benign lesions tend to grow within or along fibrous planes, compressing or displacing adjacent tissues Ducts Ducts generally measure less than 3mm and increase in size as they run toward the nipple Dilation or Duct Ectasia may occur due to a variety of normal conditions: Lactation, 3rd trimester of pregnancy, and perimenopausal changes Duct dilatation may also be due to mastitis and fibrocystic change or be seen with papillomas Contradiction: some duct dilatation may be associated with ductal carcinoma or papillary carcinoma. Margins Microlobulation Multiple small lobulations (usually 2mm) Ill-defined Obscured or indistinct margins that are poorly defined Usually indicates tumor invasion into surrounding tissues Angular Irregular, jagged margins Highly sensitive for malignancy Spiculated Straight lines which radiate from the center of a tumor Radial Extensions Duct extension – extension of tumor into a duct coursing toward the nipple Branch pattern – extension of tumor into a duct coursing away from the nipple (usually involves multiple ducts) Must be scanning in radial plane.