The Penis
advertisement

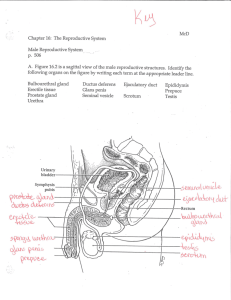
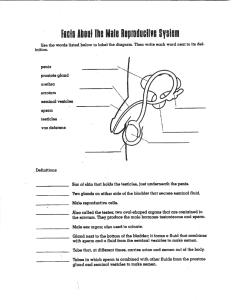
Male Sexual Anatomy, Physiology, and Response Male Sex Organs • • Sex organs serve a reproductive function Also serve other functions: • • • • Bringing pleasure to self Giving pleasure to others May serve to attract potential sexual partners Sharing of genital sexuality can play a bonding role in relationships External Structures • Penis, Scrotum The Penis • Penis: from Latin word for tail • organ through which sperm and urine pass Contains urethra for urine and semen transport Becomes erect to better penetrate the vagina and deposit sperm near the os No bone, little muscle The Penis • Myths about the penis abound • • Penis size not linked to body size or weight, muscular structure, race or ethnicity or sexual orientation. Determined by heredity. No relationship between penis size and ability to have sexual intercourse or satisfy a partner. The Penis • Three main sections: • • Root: attaches penis within the pelvic cavity Shaft: body of the penis (hangs free) • Contains 3 parallel columns of erectile tissue • • corpora cavernosa: 2 columns along the front surface corpus spongiosum: runs beneath corpora cavernosa, also forms the glans The Root of the Penis Extends into the body below the pubic bone Attached to internal pelvic muscles and can be felt in the perineum Figure 6.1 The internal structure of the penis. The Penis: Cross-Section of the Shaft The Penis • Glans penis: head of penis; most sensitive • • Corona: rim at base of the glans Frenulum: on underside of penis; triangle of sensitive skin; attaches glans to foreskin. The Penis • Foreskin: sleeve-like covering of the glans • • • Often surgically removed in infancy: circumcision Crura (pl.): formed by the corpora cavernosa; anchored by muscle to public bone Urethra: a tube that transports urine & semen • • Runs from bladder through penis. Opens at tip of glans. When penis erect, urinary duct is blocked Figure 6.2 The male reproductive organs. The Scrotum • Scrotum: a pouch of skin that holds the two testicles • • • • Scrotum skin more heavily pigmented Sparsely covered with hair Divided in the middle by a ridge of skin During sexual arousal or cold conditions, scrotum retracts to keep testicle temperature consistent (about 93°F) Cremaster muscle moves the scrotum closer to or farther from the body (protects) Internal Structures • Testes: • • • • • • Two major functions: sperm and hormone production Shaped like olives; 1.5” long and 1” diameter. Size and weight decrease as men age Not usually symmetrical in the way they hang Suspended by spermatic cord Within each testicle, there are about 1000 Seminiferous tubules: tiny compressed tubes 1-3 feet long • Production of sperm takes place in these tubes Internal Structures: CrossSection of a Testis Internal Structures • Epididymis & Vas Deferens • • • The ducts that carry sperm from testicles to urethra for ejaculation Sperm mature in epididymis, which joins with vas deferens Vas deferens joins the ejaculatory duct within prostate gland • Vas deferens can be felt within scrotal sac Internal Structures • Seminal vesicles • • Prostate gland • • • Secrete fluid that makes up 60% of semen Secretes fluid that makes up 30-35% of semen Can be stimulated in anal play Cowper’s (bulbourethral) glands • Secrete thick clear mucus prior to ejaculation Male Sexual Physiology • Reproductive processes of the male body include: • • production of hormones production and delivery of sperm Male Reproductive Hormones • Testosterone • • • • • Acts on seminiferous tubules to produce sperm Regulates sex drive Is responsible for development of secondary sex characteristics in puberty Influences growth of bones and muscle mass May affect personality Testosterone Production Testosterone is the most important male hormone Interstitial, or Leydig, cells in the testicles produce testosterone out of cholesterol Testosterone Fluctuations in a Day Spermatogenesis • Ongoing process from puberty onward • Sperm produced within seminiferous tubules of testicles (64-72 days) • • 20 days for sperm to travel through epididymis • • Several 100 million sperm produced daily During this time they become fertile & motile Upon ejaculation, sperm expelled through urethra by muscular contractions Spermatogenesis Seminiferous tubules produce and store sperm Sertoli cells (in the tubules) provide nutrition for the development of sperm This process begins with spermatogonium on the outer wall of the tubules; they move toward the center during development as primary spermatocytes, then divide to form secondary spermatocytes, and divide again into spermatids Spermatogenesis (Cont.) Spermatids form the compact head covered by an acrosome that contains enzymes to penetrate the egg The midpiece is formed and serves as the energy source The flagellum propels the mature sperm Sperm production takes 72 days, but is constant and each male produces about 300 million sperm a day Figure 6.5 Spermatogenesis is continually taking place with various levels of sperm development throughout the testis. Spermatogenesis Immature sperm travel from the tubules to the epididymis; organ that rests atop the testicle Old and faulty sperm are reabsorbed here They mature in 10-14 days in the epididymis Upon maturity they are transferred to the vas deferens for storage Male Sexual Response • Erection • • • Blood vessels expand and increase blood in penis Veins that normally carry blood out are compressed, leading to engorgement of penis Secretions from Cowper’s glands appear at tip The Ejaculatory Pathway Ejaculation – physiological process where seminal fluid is powerfully expelled from the penis Pathway organs: Vas deferens Seminal vesicles Prostate gland Cowper’s glands Ejaculation Begins in the spinal cord once a threshold is reached, and proceeds until the conclusion Ejaculation (Cont.) Once the threshold is reached: Epididymis, seminal vesicles, and prostate empty their fluids into the urethral bulb A sphincter closes off the bladder 5-15 contractions at the base of the penis squeeze the urethral bulb Ejaculate is expelled Orgasm Return to flaccid state Ejaculation & Orgasm • Emission stage • • • • Expulsion stage • • • Sperm sent into vas deferens Rhythmic contractions begin Feeling of ejaculatory inevitability Rapid contractions Semen spurts from urethral opening Orgasm • • Intensely pleasurable physical sensations that usually accompany ejaculation Followed by refractory period Ejaculate/Semen 2-5 milliliters of fluid 50-150 million sperm per milliliter Few sperm reach the ovum Sperm work together in order to fertilize the egg Semen coagulates upon ejaculation; this helps it remain in the vagina and travel into the uterus 5-20 minutes later it thins out The Breasts and Anus • Male anatomical structures that do not serve a reproductive function but may be involved in sexual activities include: • • • • • Breasts Urethra Buttocks Rectum Anus The Male Maturation Cycle Male puberty Andropause Male Puberty Around 10 years of age, the hypothalamus starts to release gonadotropin releasing hormone (GnRH) which signals the pituitary to release FSH and LH At the testes, LH stimulates testosterone production; the two combine and FSH stimulate sperm production (around 12 years) Negative feedback loop Figure 6.6 The cycle of male hormones. Male Puberty (Cont.) Many organs and glands increase in size: testicles, penis, epididymis, prostate, seminal vesicles, Cowper’s glands Growth spurt initiated by testosterone levels Testosterone and DHT develop the secondary sex characteristics: larger muscles and bones, pubic hair, thick and tough skin, deep voice, facial and chest hair, increased sex drive Andropause Testosterone levels decrease about 1% per year after 40 years of age In the 70s and 80s, andropause occurs Andropause symptoms: decreased spermatogenesis, thinner ejaculate, less ejaculatory force, libido decreases, fatigue, mood disturbances, decreased strength Controversy over hormone treatments Male Reproductive and Sexual Health Diseases of the male reproductive organs Other conditions that affect the male reproductive organs Cancer of the male reproductive organs Diseases of the Male Reproductive Organs Cryptorchidism – testes do not descend into the scrotum; surgery necessary to correct Male Reproductive and Sexual Health Diseases of the male reproductive organs Other conditions that affect the male reproductive organs Cancer of the male reproductive organs Diseases of the Male Reproductive Organs Cryptorchidism – testes do not descend into the scrotum; surgery necessary to correct Figure 6.7 Although the testicles of a fetus begin high in the abdomen, they must descend into the scrotum during fetal development. If they do not, the male may become infertile. Diseases of the Male Reproductive Organs Testicular torsion – testis is twisted on its spermatic cord; many causes (sex, exercise, sleep); symptoms are pain and swelling; immediate surgery is required to maintain the testicle Figure 6.8 Testicular torsion can occur after exercise, sexual intercourse, and even while sleeping. Diseases of the Male Reproductive Organs Priapism – persistent, painful erection not related to sexual excitement; blood is trapped in erectile tissue; common causes are drug use and unknown; treatment is cessation of drug use and, possibly, surgery Peyronie’s disease – painful curvature of the penis making penetration impossible; cause is unknown; may disappear within 2 years, or require drugs or surgery Other Conditions that Affect the Male Reproductive Organs Anabolic-androgenic steroid use – synthetic testosterone can increase muscle mass and endurance; there are also numerous physical, psychological, and emotional side effects, including erectile problems Other Conditions that Affect the Male Reproductive Organs (Cont.) Inguinal hernia – intestine goes through an abdominal opening into the scrotum, creating a bulge; can be due to heavy lifting and straining; surgery may be required Hydrocele – fluid accrues & forms a scrotal mass Cancer of the Male Reproductive Organs Testicular Penile Prostate Testicular Cancer Most common cancer in men 15-44 years Few early symptoms, early detection important; testicular self-exam Symptoms: painless mass or hardness in the testes; pain or increase in size of the testes, lower back pain, gynecomastia, shortness of breath, urethral obstruction High cure rate: radiation, chemotherapy, removal of testicle Penile Cancer Lesions on the penis may be benign or malignant and are usually treatable; may also be a STI Penile cancer is not common Prostate Cancer Prostate glands enlarge with age and this is typically unproblematic, other than interfering with urination Prostate cancer is one of the most common in American men, typically in men over 50 years Risk factors: age, high fat diet, race, genetics Symptoms: pain in the lower back, pelvis, or upper thigh, and urinary abnormalities Detected through rectal exam and blood test Prostate Cancer (Cont.) Treatments: “watchful waiting”, radical prostatectomy, radiation, cryosurgery, drugs that attack cancerous cells