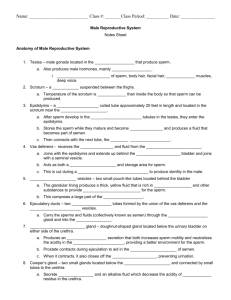
Male Reproductive System
advertisement

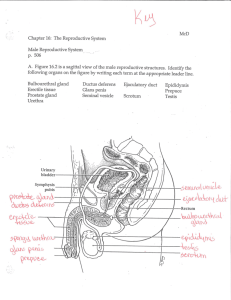
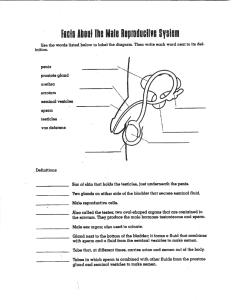
Male Reproductive System 1 Male Reproductive Organs scrotum and testes ducts accessory sex glands penis 2 Male Reproductive Organs prostate gland seminal vesicle penis epididymis ductus deferens testicle within scrotum 3 Scrotum (cont.) pendulous sac of loose skin and fascia supports testes divided internally by medial septum, supporting each testis left testes is usually suspended lower than the right so they are not compressed against each other 4 Scrotum (cont.) location (outside the body) and muscle fibers regulate temperature of the testes production and survival of sperm require temperature about 3o lower than normal body temperature contains Dartos muscle - contains smooth muscle fibers - causes wrinkling of scrotum 5 6 Cremaster Muscle continuation of internal oblique muscle stimulation by touch or cold results in contraction of muscle pulling testicles closer to the body presence of cremasteric reflex indicates integrity of the first lumbar nerve segment absence of reflex indicates damage 7 Testes primary sex organs; male gonads paired oval glands two inches long, one inch in diameter develop high in posterior fetal abdominal wall descend into scrotum during seventh month of fetal development suspended in scrotum by spermatic cord 8 9 Testes (cont.) Produce: - sperm - testosterone divided into compartments (about 250) called lobules formed by inward extensions of tunica albuginea - contain several highly coiled tubules called seminiferous tubules spermatozoa are formed in walls of tubules 10 Covering of Testes tunica vaginalis - pouch-like sac of peritoneum - formed during descent of the testes tunica albuginea - internal to tunica vaginalis - dense, white, fibrous tissue 11 Cryptorchidism occurs when testes fail to descend into scrotum results in sterility because of higher temperature in pelvic cavity - higher temperature destroys cells involved in development of sperm cells Treatment: - human growth hormone - surgery 12 Seminiferous Tubules Consists of: - spermatogenic cells - sustenacular cells - blood-testis barrier - basement membrane 13 Spermatogenic Cells line walls of seminiferous tubules towards lumen of tubules cells are progressively more mature Cells in various stages of development: - spermatogonia - primary spermatocytes - secondary spermatocytes - spermatids 14 Spermatogonia most immature cells lie next to basement membrane have 46 chromosomes (diploid) Primary Spermatocytes produce four spermatids have 46 chromosomes (diploid) 15 16 Secondary Spermatocytes cells formed by first nuclear division (reduction division) each cell has 23 chromosomes (haploid) Spermatids cells formed by second nuclear division (equatorial division) - mitotic each cell has 23 chromosomes (haploid) 17 Sustentacular Cells extend from outer basement membrane to the lumen support and nourish developing cells immature cells are embedded in luminal membranes secrete inhibin - protein hormone - directly affects anterior pituitary by inhibiting FSH secretion 18 Follicle-Stimulating Hormone FSH encourages spermatogenesis and stimulates sustentacular cells once adequate spermatogenesis level is achieved, inhibin is secreted - inhibits FSH secretion and decreases spermatogenesis if spermatogenesis occurs too slowly, lack of inhibin permits FSH secretion - increases rate of spermatogenesis 19 20 Blood-Testis Barrier developing sperm have surface antigens recognized as foreign by immune system prevents an immune response against sperm isolates cells from blood Basement Membrane surrounds each seminiferous tubule 21 Mature Sperm travel through seminiferous tubules to straight tubules through rete testis and from testes into epididymis 22 Epididymis half-moon-shaped organ encircling posterior of each testis site of sperm maturation contains highly coiled tube called the ductus epididymis used for storage of spermatozoa continuous with ductus deferens during ejaculation, muscle contractions move sperm and seminal fluid into ductus deferens 23 Ductus Deferens also called vas deferens or seminal duct 18 inch long tube carries spermatozoa from epididymis of each testis to an ejaculatory duct ascends along posterior border of epididymis 24 Ductus Deferens (cont.) enters pelvic cavity through inguinal canal loops over side and down posterior surface of urinary bladder terminal end is called ampulla stores sperm and moves sperm from epididymis to urethra seminal vesicle joins at distal end of ampulla 25 Vasectomy method of sterilization portion of each ductus deferens is removed sperm production continues but cannot be expelled from body 26 Ejaculatory Duct distal end of ampulla one inch long formed from union of duct from seminal vesicle and ductus deferens passes into prostate gland joins prostatic urethra eject sperm into prostatatic urethra just prior to ejaculation 27 Urethra tube extends from urinary bladder to tip of penis about 8 inches long Three parts: - prostatic urethra - membranous urethra - spongy urethra 28 Prostatic Urethra passes through prostate gland Membranous Urethra passes through urogenital diaphragm Spongy Urethra passes through corpus spongiosum of penis 29 Male Reproductive Glands seminal vesicles prostate gland bulbourethral glands 30 31 Seminal Vesicles paired, convoluted, pouch-like structures posterior to and at base of urinary bladder secrete an alkaline, viscous fluid - contains fructose, prostaglandins, and fibrinogen - helps to neutralize acid of female tract - provides nourishment for sperm - 60% of the volume of semen 32 Fructose used for ATP production Prostaglandins contribute to sperm motility and viability may also stimulate muscular contraction within female reproductive tract Fibrinogen aids in semen coagulation 33 Prostate Gland single, donut-shaped, walnut size inferior to urinary bladder surrounds superior portion of urethra secretes milky, slightly acidic fluid - contains citric acid, acid phosphate, clotting emzymes, and fibrinolysin - aids in sperm motility and viability - 25% of the volume of semen 34 Bulbourethral Gland also known as Cowper’s glands paired, size of peas lie beneath prostate gland on either side of membranous urethra ducts open into spongy urethra secrete alkaline, mucus-containing fluid - neutralizes acid ; lubricates end of penis - 10% of the volume of semen 35 Penis cylindrical organ transports urine and semen through urethra to the outside of body Consists of: - body - glans penis - root 36 Body of the Penis composed of three cylindrical masses of spongy erectile tissue enclosed in fascia and skin permeated by blood sinuses sexual stimulation causes dilation of arteries supplying penis blood accumulates in erectile tissue, and penis swells and elongates, producing an erection 37 Erectile Tissue corpora cavernosa penis - two dorsolateral masses corpus spongiosum penis - smaller midventral mass - contains spongy urethra 38 Glans Penis distal end of corpus spongiosum slightly enlarged forms tip of penis Anatomy: - corona - external urethral orifice - prepuce or foreskin 39 Corona margin of glans penis External Urethral Orifice slitlike opening of urethra Prepuce or Foreskin covers the glans penis often removed in circumcision 40 Circumcision removal of part or all of the prepuce many physicians believe it decreases risk of urinary tract infections, possible protection from penile cancer, and lowers risk of sexually transmitted diseases 41 Root of Penis attached portion Consists of: - bulb of penis expanded portion of the base of the corpus spongiosum penis - crura separated and tapered portions of the corpora cavernosa penis 42 Semen Mixture of: - sperm secretions of the seminal vesicles, prostate gland, and bulbourethral glands 43 Characteristics of Semen volume - 2.3 - 2.5 ml per ejaculation color - milky appearance because of prostate secretion sperm count - 50 - 150 million sperm per ml 44 Characteristics of Semen (cont.) motility of sperm - at least 60% active, good forward motility in order to be viable pH is slightly alkaline (7.20 - 7.60) specific gravity - denser than water (1.0280) morphology - at least 80% normally shaped in order to be viable 45 Characteristics of Semen (cont.) antibiotics - seminalplasmin - has ability to destroy certain bacteria nutrients - fructose - provides energy source necessary for sperm motility buffers - phosphate and bicarbonate - maintain relatively constant pH of semen 46 Characteristics of Semen (cont.) enzymes - hyaluronidase, proteinases - digest material covering ovum clotting enzymes - coagulate semen fibrinolysin - liquifies coagulated semen 47 Hormonal Control of Male Reproductive System Controlled by: - GnRH (gonadotropin releasing hormone) - FSH (follicle-stimulating hormone) - LH (luteinizing hormone) - inhibin - testosterone 48 Gonadotropin Releasing Hormone secreted by hypothalamus carried by anterior pituitary gland - stimulates the release of gonadotropins, follicle-stimulating hormone, and luteinizing hormone 49 Follicle-Stimulating Hormone stimulates sustentacular cells in seminiferous tubules - secrete chemicals that stimulate spermatogenesis - secrete inhibin which has a negative feedback effect on anterior pituitary gland, inhibiting secretion of FSH 50 Luteinizing Hormone stimulates interstitial endocrinocytes located in spaces within seminiferous tubules stimulates testosterone secretion 51 Androgens male sex hormones testosterone is principal androgen - synthesized from cholesterol in the testes - in some target cells testosterone is not active and must be reduced and converted into dihydrotestosterone (DHT) 52 Androgen Functions male pattern of development before birth sexual characteristics sexual functions metabolism 53 Male Pattern of Development Before Birth development of reproductive system ducts descent of testes development of external genitals (by DHT) converts some androgens into estrogens which aid in brain development 54 55 56 Sexual Characteristics development and enlargement of male sex organs development of male secondary sex characteristics 57 Male Secondary Sex Characteristics muscular and skeletal growth wide shoulders, narrow hips pubic, axillary, facial, and chest hair growth thickening of skin increased sebaceous gland secretion enlargement of larynx and deepening of voice 58 Sexual Functions male sexual behavior spermatogenesis sex drive 59 Metabolism androgens are anabolic hormones which stimulate protein synthesis - leading to heavier muscle and bone mass in males cause cessation of bone growth by stimulating closure of epiphyseal plate increase rate of metabolism and production of red blood cells 60