oral presentation
advertisement
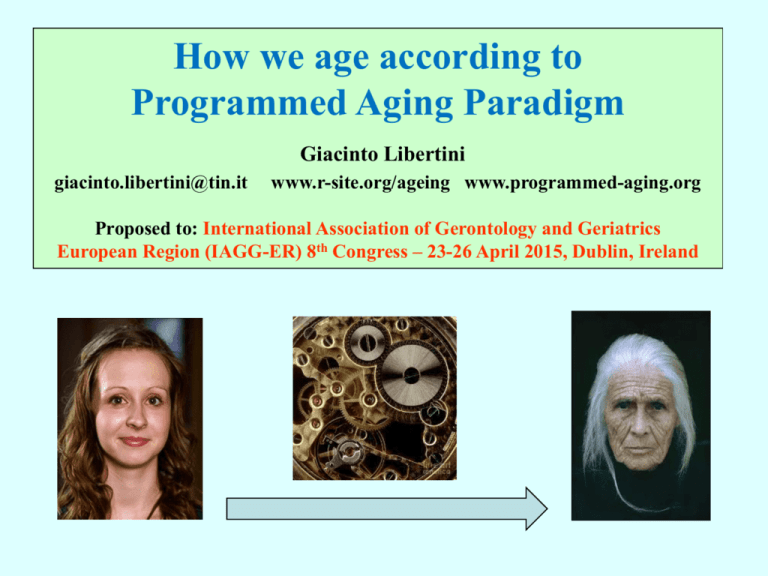
How we age according to Programmed Aging Paradigm Giacinto Libertini giacinto.libertini@tin.it www.r-site.org/ageing www.programmed-aging.org Proposed to: International Association of Gerontology and Geriatrics European Region (IAGG-ER) 8th Congress – 23-26 April 2015, Dublin, Ireland There are two antithetical general explanations for “aging” [1], here precisely defined as “age-related progressive fitness decline or mortality increase”. They are totally different and have very important opposed implications. Therefore, they deserve to be defined “paradigms”. The first, here defined as the “Old Paradigm”, explains aging as the effect of various factors insufficiently opposed by natural selection [2]: Aging is the main FAILURE of evolution! The second, here defined as the “New Paradigm”, explains aging as a physiologic phenomenon determined and favored by supraindividual selection in particular conditions [3]: Aging is an extraordinary ACHIEVEMENT of evolution! The two paradigms, by definition, are incompatible with each other. [1] Goldsmith T. The Evolution of Aging (3rd ed.). Azinet Press, USA 2013. [2] Kirkwood TBL & Austad SN. Why do we age? Nature 2000; 408:233-8. [3] Libertini G. Empirical evidence for various evolutionary hypotheses on species demonstrating increasing mortality with increasing chronological age in the wild. TheScientificWorld Journal 2008; 8:183-93. For the New Paradigm, aging is a particular type of “phenoptosis” The concept of “phenoptosis” [1, 2] includes a large category of well-known phenomena [3] characterized by the self-sacrifice of an individual (genetically caused / induced and regulated, & favored by natural selection, in terms of supra-individual selection). Etc. Autogeny Aphagy in adult insects Hormonally triggered senescence in plants Death after spawning Death of the male associated with mating / reproduction Aging (“slow phenoptosis” [4]) Endotokic matricide [1] Skulachev VP. Aging is a specific biological function rather than the result of a disorder in complex living systems: biochemical evidence in support of Weismann's hypothesis. Biochem (Mosc) 1997; 62(11):1191-5. [2] Libertini G. Classification of Phenoptotic Phenomena. Biochem (Mosc) 2012; 77(7):707-15. [3] Finch CE. Longevity, Senescence and the Genome, University of Chicago Press, London 1990. [4] Skulachev VP. Programmed Death Phenomena: From Organelle to Organism. Ann NY Acad Sci 2002; 959:214-37. Here, I do not want to discuss arguments and evidence for or against the two paradigms, but only focus on a key topic: how we age, i.e. a general description of aging process in our species (and in mammals in general) on the basis of mechanisms genetically determined and regulated. The New Paradigm predicts and requires the existence of specific mechanisms, genetically determined and regulated, which cause aging [1]. On the contrary, the Old Paradigm excludes the possibility that such mechanisms exist: their existence would therefore demonstrate that the paradigm is false [2]. Only clear and accepted evidence will be used in the following exposition. [1] Libertini G. Empirical evidence for various evolutionary hypotheses on species demonstrating increasing mortality with increasing chronological age in the wild, TheScientificWorld Journal 2008; 8:183-93. [2] Kirkwood TBL, Austad SN. Why do we age? Nature 2000; 408:233-8. First evidence: Programmed Cell Death (PCD) A cell may dies by necrosis because of accidental events (injury, mechanical stress, infection, ischemia, etc.), or by one of various types of PCD, e.g.: - The keratinization of epidermis or hair cells; - The detachment of cells from the lining of intestines or other body cavities; - Osteocytes phagocytized by osteoclasts; - The transformation of erythroblasts in erythrocytes and their subsequent removal by macrophages. - Apoptosis, an ordinate process of self-destruction with non-damaging disposal of cellular debris that makes it different from necrosis. The phenomenon was for the first time described and clearly differentiated from necrosis in the observation of normal hepatocytes [1]. A pivotal function of apoptosis in vertebrates is related to cell turnover in healthy adult organs, as well documented for many tissues and organs [2]. Beware: PCD is often used as synonymous of apoptosis, but this is a wrong simplification! [1] Kerr JFR et al. Apoptosis: a basic biological phenomenon with wide-ranging implications in tissue kinetics. Br. J. Cancer 1972; 26:239-57. [2] Libertini G. The Role of Telomere-Telomerase System in Age-Related Fitness Decline, a Tameable Process, in Telomeres: Function, Shortening and Lengthening, Nova Sc. Publ., New York, 2009. Second evidence: Cell Turnover The continuous death of cells by PCD is balanced by an equal proliferation of appropriate stem cells, which is regulated and limited by telomere-telomerase system. “Each day, approximately 50 to 70 billion cells perish in the average adult because of programmed cell death (PCD). Cell death in self-renewing tissues, such as the skin, gut, and bone marrow, is necessary to make room for the billions of new cells produced daily. So massive is the flux of cells through our bodies that, in a typical year, each of us will produce and, in parallel, eradicate, a mass of cells equal to almost our entire body weight” [1]. [1] Reed JC. Dysregulation of Apoptosis in Cancer. J Clin Oncol 1999; 17:2941-53. Duplication of stem cells CELL TURNOVER Cell death by PCD Cell turnover is a general pattern in vertebrates, but not for all animals (e.g., the adult stage of the worm Caenorhabditis elegans has a fixed number of cells). Cell Turnover (continued) The rhythm of cell turnover varies greatly depending on cell type and organ. In the intestinal epithelium “cells are replaced every three to six days”, while “Bone has a turnover time of about ten years in humans” [1]. VERY SLOW SLOW VERY QUICK [1] Alberts B. et al. Essential Cell Biology, 4° ed., Garland Science, 2013. QUICK Third evidence: “on/off” cell senescence and “gradual” cell senescence Cell replication, which is essential to allow cell turnover, is limited by known mechanisms. In 1961, Hayflick demonstrated that cells divide only a finite number of times [1]. Olovnikov hypothesised that, as DNA molecule shortens at each duplication, this could explain the finite number of duplications [2]. The end of DNA molecule (telomere) was shown, first in a protozoan species, to be a simple repeated sequence of nucleotides [3]. The discovery of telomerase which added other sequences of the nucleotides was a necessary explanation for cells, as those of germ line, capable of numberless divisions [4]. Telomerase was shown to be repressed by regulatory proteins [5]. In cells where telomerase is not active, an infinite number of duplications is impossible for the progressive telomere shortening. Before telomeres reach their minimum length, two phenomena are described ... [1] Hayflick L & Moorhead PS. The serial cultivation of human diploid cell strains. Exp Cell Res 1961; 25:585-621. [2] Olovnikov AM. A theory of marginotomy: The incomplete copying of template margin in enzyme synthesis of polynucleotides and biological significance of the problem. J Theor Biol 1973; 41:181-90. [3] Blackburn EH & Gall JG. A tandemly repeated sequence at the termini of the extrachromosomal ribosomal RNA genes in Tetrahymena. J Mol Biol 1978; 120:33-53. [4] Greider CW & Blackburn EH. Identification of a specific telomere terminal transferase activity in Tetrahymena extracts. Cell 1985; 51:405-13. [5] van Steensel B & de Lange T. Control of telomere length by the human telomeric protein TRF1. Nature 1997; 385:740-3. 1) “on/off” cell senescence In a cell in “cycling” state, the telomere, whatever its length, oscillates between two phases: “capped” and “uncapped” (by a protein complex). The probability of the uncapped phase is inversely proportional to the relative reduction of telomere length. In the uncapped phase, the cell is vulnerable to the transition to noncycling state, i.e. to the activation of cell senescence program [1]. Figure 1 from [1] [1] Blackburn EH. Telomere states and cell fates. Nature 2000; 408:53-6. 1) “on/off” cell senescence (continued) Cell senescence, which can also be activated by other factors, is determined by a mechanism in which the p53 protein is involved. It is characterized by the block of the cell cycle and by a long series of changes in the expression of cellular genes. These changes also include alterations of cellular secretions that cause alterations of the extracellular matrix, inflammation, reduced secretion of important structural proteins such as elastin and collage, and impairments of the surrounding cells [1]. The alterations are stereotyped and predictable: cell senescence has been described as a “fundamental cellular program” [2]. [1] Fossel MB. Cells, Aging and Human Disease. Oxford University Press, New York 2004. [2] Ben-Porath I & Weinberg R. The signals and pathways activating cellular senescence. Int J Biochem Cell Biol 2005; 37:961–76. 2) “gradual” cell senescence The progressive shortening of telomeres has another effect. The telomere is covered (capped) by a protein complex that, as the telomere shortens, hides the subtelomeric DNA and causes transcriptional silencing. “As the telomere shortens, the hood slides further down the chromosome .... the result is an alteration of transcription from Figure 7 from [2] portions of the chromosome immediately adjacent to the telomeric complex, usually causing transcriptional silencing, although the control is doubtless more complex than merely telomere effect through propinquity … These silenced genes may in turn modulate other, more distant genes (or set of genes). There is some direct evidence for such modulation in the subtelomere ...” [1] [1] Fossel MB. Cells, Aging and Human Disease. Oxford University Press, New York 2004. [2] Libertini G. The Role of Telomere-Telomerase System in Age-Related Fitness Decline, a Tameable Process, in Telomeres: Function, Shortening and Lengthening, Nova Sc. Publ., New York 2009. “on/off” cell senescence and “gradual” cell senescence (continued) These alterations in gene expression progressively affect the functioning of cells and of the intercellular environment. With the activation of telomerase, cell senescence and all related alterations are completely canceled [1-5] cell senescence telomerase activation non-senescent cell senescent cell [1] Bodnar AG et al. Extension of life-span by introduction of telomerase into normal human cells. Science 1998; 279:349-52. [2] Counter CM et al. Dissociation among in vitro telomerase activity, telomere maintenance, and cellular immortalization. Proc Natl Acad Sci USA 1998; 95:14723-8. [3] Vaziri H. Extension of life span in normal human cells by telomerase activation: a revolution in cultural senescence. J Anti-Aging Med 1998; 1:125-30. [4] Vaziri H & Benchimol S. Reconstitution of telomerase activity in normal cells leads to elongation of telomeres and extended replicative life span. Curr Biol 1998; 8:279-82. [5] de Lange T & Jacks T. For better or worse? Telomerase inhibition and cancer. Cell 1999; 98:273-5. “on/off” cell senescence and “gradual” cell senescence (continued) “Telomerase gene transfection (“telomerization”) is an experimental determinant, switching somatic cells from mortal to immortal without disruption of the remainder of gene expression … This process of gene control is central to cell aging and experimental intervention. Resetting gene expression occurs in knockout mice, cloning, and other interventions, permitting us to make sense of how cell senescence causes aging in organisms.” [1] “Cells do not senesce because of wear and tear, but because they permit wear and tear to occur because of an altered gene expression. Telomerization effectively replaces the score, allowing the gene to express their previous pattern. … cells do not senesce because they are damaged, but permit damage because they senesce. Homeostatic processes suffice indefinitely in germ cell lines; they suffice in somatic cells if senescence is abrogated.” [1] [1] Fossel MB. Cells, Aging and Human Disease. Oxford University Press, New York 2004. With the passage of time (and with very different rhythms, varying for cell types and organs), in a tissue: - the percentage of cells in senescent state increases; - the percentage of cells with functions more or less affected by telomere shortening and the consequent interference in the subtelomeric region increases. Figure 8-2 (partial) from [1]: “a modicum of cells display varying degrees of senescent change” [1] Fossel MB. Cells, Aging and Human Disease. Oxford University Press, New York 2004. This leads, for each tissue and organ, to the “atrophic syndrome”, which is characterized by [1]: a) reduced mean cell duplication capacity and slackened cell turnover; b) reduced number of cells (atrophy); c) substitution of missing specific cells with nonspecific cells; d) hypertrophy of the remaining specific cells; e) altered functions of cells with shortened telomeres or definitively in noncycling state; f) alterations of the surrounding milieu and of the cells depending from the functionality of the senescent or missing cells; g) vulnerability to cancer because of dysfunctional telomere-induced instability [2]. [1] Libertini G. The Role of Telomere-Telomerase System in Age-Related Fitness Decline, a Tameable Process, in Telomeres: Function, Shortening and Lengthening, Nova Sc. Publ., New York 2009. [2] DePinho RA . The age of cancer. Nature 2000; 408:248-54. AGED SKIN Human epidermis turnover is determined by stem cells located in the dermalepidermal junction, a corrugated surface. In old subjects, dermal-epidermal junction is flattened, an indirect sign of the reduction of epidermis stem cells, and the rate of epidermal renewal is reduced [1]. In derma, as a likely consequence of the exhaustion of specific stem cells, a general reduction of all its components (melanocytes, Langerhans cells, dermal fibroblasts, capillaries, blood vessels within the reticular dermis, mast cells, eccrine glands, hair. etc.) is reported and nails grow more slowly [1]. “The study of aging skin is one that presents a paradigm for aging of other organs.” [1] [1] Griffiths CEM. Aging of the Skin. In: Tallis, RC et al. (eds), Brocklehurst’s Textbook of Geriatric Medicine and Gerontology, 5th edition. Churchill Livingstone, New York 1998. D-E junction AGED MUSCLE “In detailed studies it has been shown that the progressive reduction that occurs in muscle volume with aging can be detected from age 25 years and that up to 10 percent of muscle volume is lost by age 50 years. Thereafter the rate of muscle volume atrophy increases, so that by 80 years almost half the muscle has wasted. ... Both reduction in fiber number and fiber size are implicated in the loss of muscle volume.” [1] Figure 78-4 from [2]: Age-related decline in maximum voluntary isometric force (MVF, open symbols) and in cross-sectional area (CSA, black symbols) in various muscles. [1] Cumming WJK. Aging and neuromuscolar disease. In: Tallis, RC et al. (eds), Brocklehurst’s Textbook etc., 1998. [2] Bruce S. Muscle strength. In: Tallis, RC et al. (eds), Brocklehurst’s Textbook etc., 1998. AGED BONE “Involutional bone loss ... starts between the ages of 35 and 40 in both sexes, but in women there is an acceleration of bone loss in the decade after menopause. Overall, women lose 35 to 50 percent of trabecular and 25 to 30 percent of cortical bone mass with advancing age, whereas men lose 15 to 45 percent of trabecular and 5 to 15 percent of cortical bone. ... Bone loss starts between the ages of 35 and 40 years in both sexes, possibly related to impaired new bone formation, due to declining osteoblast function.” [1] [1] Francis RM. Metabolic Bone Disease. In: Tallis et al. (eds.), Brocklehurst’s textbook etc., 1998. AGED LUNG Lung volumes (FEV1, FVC) decline with age [1]. “The most important age-related change in the large airways is a reduction in the number of glandular epithelial cells ... the area of the alveoli falls and the alveoli and alveoli ducts enlarge. Function residual capacity, residual volume, and compliance increase. ...” [2] young lung senile enphysema in an old lung [1] Enright PL et al. Spirometry Reference Values for Women and Men 65 to 85 Years of Age. Cardiovascular Health Study. Am Rev Respir Dis 1993; 147:125-33. [2] Connolly MJ. Age-Related Changes in the Respiratory System. In: Tallis et al. (eds.), Brocklehurst’s textbook etc., 1998. AGED HEART An old and deep-rooted belief is that the heart is an organ incapable of regeneration and without cell turnover. But, in a normal heart, every day about 3 million myocytes die by apoptosis and are replaced by cardiac stem cells: “the entire cell population of the heart is replaced approximatively every 4.5 years … The human heart replaces completely its myocyte population about 18 time during the course of life, independently from cardiac diseases.” [1]. The senile heart has a decreasing number of myocytes owing to the progressive decline in the ability to duplication of cardiac stem cells [1]. But the heart chambers, for lack of contractile capacity, are dilated and, so, the senile heart, although atrophic as number of cells, is morphologically hypertrophic [2]. [1] Anversa P et al. Life and Death of Cardiac Stem Cells. A Paradigm Shift in Cardiac Biology. Circulation 2006; 113:1451-63. [2] Aronow WS. Effects of Aging on the Heart. In: Tallis et al. (eds.), Brocklehurst’s textbook etc., 1998. AGED SKELETAL MUSCLE Myocytes of skeletal muscle are cells with turnover as heart myocytes! Stem cells from muscles of old rodents divide in culture less than cells from muscles of young rodents [1]. A transplanted muscle suffers ischaemia and complete degeneration and then there is a complete regeneration by action of host myocyte stem cells that is poorer in transplants from older animals [2]. In Duchenne muscular dystrophy, there is a chronic destruction of myocytes that are continually replaced by the action of stem cells until these are exhausted [3]. [1] Schultz E, Lipton BH. Skeletal muscle satellite cells: changes in proliferation potential as a function of age. Mech Age Dev 1982; 20:377-83. [2] Carlson BM, Faulkner JA. Muscle transplantation between young and old rats: age of host determines recovery. Am J Physiol 1989; 256:C1262-6. [3] Adams V et al. Apoptosis in skeletal muscle. Front Biosci 2001; 6:D1-11. AGED ENDOTHELIUM The correct functionality of endothelial cells is essential to avoid atherogenesis and its complications, such as cardiac infarctions, cerebral ischemia and other diseases derived from compromised blood circulation [1]. Their turnover is assured by endothelial progenitor cells, derived from bone marrow, whose number has been shown to be inversely related to age, reduced by cardiovascular risk factors (cigarette smoking, diabetes, hypertension, hypercholesteremia, etc.), and increased by drugs, such as statins, which protect organ integrity [1]. Moreover, with negative relation, the number of endothelial progenitor cells is a predictor of cardiovascular risk equal to or more significant than Framingham risk score [1, 2]. In the senile state, diseases deriving from a compromised endothelial function increase exponentially in correlation with the age, even if other cardiovascular risk factors are absent [3]. These factors anticipate and amplify the risk [3], while drugs with organ protection qualities, as statins [4], ACE-inhibitors and sartans [5] counter their effects. [1] Hill JM et al. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med 2003; 348:593-600. [2] Werner N et al. Circulating endothelial progenitor cells and cardiovascular outcomes. N Engl J Med 2005; 353:999-1007. [3] Tallis RC et al. (eds.). Brocklehurst’s Textbook of Geriatric Medicine and Gerontology, 5th ed., Churchill Livingstone, New York 1998. [4] Davidson MH. Overview of prevention and treatment of atherosclerosis with lipid-altering therapy for pharmacy directors. Am J Manag Care 2007; 13:S260-9. [5] Weir M.R. Effects of renin-angiotensin system inhibition on end-organ protection: can we do better? Clin Ther 2007; 29:1803-24. AGED INTESTINAL VILLI In each intestinal crypt, there are four to six stem cells that with their intensive duplication activity renew continuously the epithelium of the small intestine [1]. In healthy old individuals, in comparison with young individuals the transit time for cells from crypts to villous tips decreases and villi become broader, shorter and with less cellularity [2]. These changes, surely due to a declining mitotic activity of crypt stem cells, as hypothesised from a long time [2], reduce intestinal functionality and, likely, overall fitness. [1] Barker N et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature 2007; 449:1003-7. [2] Webster SGP. The gastrointestinal system – c. The pancreas and the small bowel. In: Brocklehurst, JC (ed) Textbook of Geriatric Medicine and Gerontology (2nd ed.), Churchill Livingstone, New York 1978. AGED LIVER Liver volume declines with age [1], both in absolute values and in proportion to body weight [2], and this reduction has been estimated to be about 37 percent between ages 24 and 91 [1]. Liver blood flow also declines with age, by about 53 percent between ages 24 and 91 [1]. However, while liver size declines with age, hepatocytes increase in size, unlike in the liver atrophy that accompanies starvation [3]. Cirrhosis is the final stage of chronic destruction of hepatocytes caused by hepatitis, alcoholism or other factors. When hepatocyte stem cells exhaust their duplication capacities, the liver is transformed by a general atrophic process, often complicated by carcinomas caused by dysfunctional telomere-induced instability [4, 5]. [1] Marchesini G et al. Galactose Elimination Capacity and Liver Volume in Aging Man. Hepatology 1988; 8:1079-83. [2] Wynne HA et al. The Effect of Age upon Liver Volume and Apparent Liver Blood Flow in Healthy Man. Hepatology 1989; 9:297-301. [3] James OFW. The Liver. In: Tallis et al. (eds.), Brocklehurst’s textbook etc., 1998. [4] DePinho RA. The age of cancer. Nature 2000; 408:248-54. [5] Artandi SE. Telomere shortening and cell fates in mouse models of neoplasia. Trends Mol Med 2002; 8:44-7. AGED BLOOD "... Gradual involution of red marrow continues but is especially marked after the age of 70 years when iliac crest marrow cellularity is reduced to about 30 percent of that found in young adults.” [1] In vitro neutrophil functions (e. g: endothelial adherence, migration and phagocytosis capacity, granule secretory behavior, etc.) are insignificantly affected by age but in vivo significantly fewer neutrophils arrive at the skin abrasion sites studied in older people [2]. The proliferative capacity of T lymphocytes to nonspecific mitogens is greatly reduced with aging [3]. It has been suggested that age-related functional decline in adult tissue hematopoietic stem cells limits longevity in mammals [4]. [1] Gilleece MH, Dexter TM. Aging and the Blood. Tallis et al. (eds.), Brocklehurst’s textbook etc., 1998. [2] MacGregor RR, Shalit M. Neutrophil Function in Healthy Elderly Subjects. J Gerontol 1990; 45:M55-60. [3] Gravenstein S, Fillit H, Ershler WB. Clinical Immunology of Aging. Tallis et al. (eds.), Brocklehurst’s textbook etc., 1998. [4] Geiger H. and Van Zant G. The aging of lympho-hematopoietic stem cells. Nat. Immunol. 2002; 3:329-33. AGED KIDNEY “Age-induced renal changes are manifested macroscopically by a reduction in weight of the kidney and a loss of parenchymal mass. … The decrease in weight of the kidneys corresponds to a general decrease in the size and weight of all organs. Microscopically, the most impressive changes are reductions in the number and size of nephrons. Loss of parenchymal mass leads to a widening of the interstitial spaces between the tubules. There is also an increase in the interstitial connective tissue with age. The total number of identifiable glomeruli falls with age, roughly in accord with the changes in renal weight.” [1] Microalbuminuria, a simple marker of nephropathy, is “predictive, independently of traditional risk factors, of all-cause and cardiovascular mortality and CVD events within groups of patients with diabetes or hypertension, and in the general population ... It may ... signify systemic endothelial dysfunction that predisposes to future cardiovascular events” [2], and this implicates that drugs effective in “organ protection” defend renal functionality too. [1] Jassal V et al. Aging of the Urinary Tract. Tallis et al. (eds.), Brocklehurst’s textbook etc., 1998. [2] Weir MR. Microalbuminuria and cardiovascular disease. Clin J Am Soc Nephrol 2007; 2:581-90. Cell types without turnover AGED RETINAL NERVOUS CELLS Photoreceptor cells (cones and rods) are highly differentiated nervous cells with no turnover, but metabolically depending on other cells with turnover, retina pigmented cells (RPC), which are highly differentiated gliocytes. Without the macrophagic activity of RPC, photoreceptor cells cannot survive [1]. The age-related decline or RPC turnover causes the death of photoreceptor cells, which is more clinically evident in macula function (age-related macular degeneration or ARMD). ARMD affects 5%, 10% and 20% of subjects 60, 70 and 80 years old, respectively [1], and it is likely that a large proportion of older individuals suffer from ARMD. [1] Berger JW et al. Age-related macular degeneration, Mosby, USA 1999. AGED NEURONS OF THE CENTRAL NERVOUS SYSTEM The neurons depend on particular types of gliocytes (microglia cells). Microglia cells degrade β-amyloid protein [1, 2] and this function is known to be altered in Alzheimer Disease (AD) [3] with the consequent noxious accumulation of the protein. The hypothesis that AD is caused by the declining turnover of microglia cells has been proposed [4-7]. [1] Qiu WQ et al. Insulin-degrading enzyme regulates extracellular levels of amyloid beta-protein by degradation. J Biol Chem 1998; 273:32730-8. [2] Vekrellis K et al. Neurons regulate extracellular levels of amyloid beta-protein via proteolysis by insulindegrading enzyme. J Neurosci 2000; 20:1657-65. [3] Bertram L et al. Evidence for genetic linkage of Alzheimer's disease to chromosome 10q. Science 2000; 290:2302-3. [4] Fossel MB. Reversing Human Aging. William Morrow and Company, New York 1996. [5] Fossel MB. Cells, Aging and Human Disease. Oxford University Press, New York 2004. [6] Libertini G. Prospects of a Longer Life Span beyond the Beneficial Effects of a Healthy Lifestyle, Ch. 4 in Handbook on Longevity: Genetics, Diet & Disease, Nova Sc. Publ., New York 2009. [7] Flanary B. Telomeres: Function, Shortening, and Lengthening, in Telomeres: Function, Shortening and Lengthening, Nova Science Publishers Inc., New York 2009. AGED EYE CRYSTALLINE LENS The crystalline lens has no cell in its core, but its functionality depends on lens epithelial cells that show turnover [1]. “Many investigators have emphasized post-translational alterations of long-lived crystalline proteins as the basis for senescent ocular cataracts. It is apparent in Werner syndrome that the cataracts result from alterations in the lens epithelial cells” [2], which is consistent with age-related reduction in growth potential for lens epithelial cells reported for normal human subjects [1]. Smoke and diabetes are risk factors for cataract [3]. Statins lower the risk of cataract [4]. This has been attributed to “putative antioxidant properties” [4], but could be the consequence of effects on lens epithelial cells analogous to those on endothelial cells [5]. [1] Tassin J et al. Human lens cells have an in vitro proliferative capacity inversely proportional to the donor age. Exp. Cell Res. 1979; 123:388-92. [2] Martin GM & Oshima J. Lessons from human progeroid syndromes. Nature 2000; 408:263-6. [3] Delcourt C et al. Risk factors for cortical, nuclear, and posterior subcapsular cataracts: the POLA study. Pathologies Oculaires Liées à l'Age. Am J Epidemiol 2000; 151:497-504. [4] Klein BE et al. Statin use and incident nuclear cataract. JAMA 2006; 295:2752-8. [5] Hill JM et al. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N. Engl. J. Med 2003; 348:593-600. Programmed cell death, cell senescence (“on/off” and “gradual”), cell duplication limits (variable according to cell types and influenced by various physiological and pathological events), cell turnover and its limitations (variable depending on the cell types) are all phenomena genetically determined and regulated. Some features of these phenomena have no justification in terms of physiological factors other than aging. In particular, the supporters of Old Paradigm try to justify the limits in cell replication as a general defense against cancer [1,2]. But: - Species with negligible senescence (i.e., with individuals showing no age-related decay) have no age-related reduction of telomerase activity and no increase in mortality due to cancer [3]. - In the human species, studied under natural conditions, fitness decline (i.e., aging) reaches significant levels without a detectable incidence of cancer mortality. It is untenable that a defense against cancer kills large part of the population before cancer as cause of death becomes detectable [4]. [1] Campisi J. The biology of replicative senescence. Eur J Cancer 1997; 33(5):703–9. [2] Wright WE & Shay JW. Telomere biology in aging and cancer. J Am Geriatr Soc 2005; 53(9 S):S292–4. [3] Libertini G. Empirical evidence for various evolutionary hypotheses on species demonstrating increasing mortality with increasing chronological age in the wild. The Scientific World Journal 2008; 8:182-93. [4] Libertini G. Evidence for Aging Theories from the Study of a Hunter–Gatherer People (Ache of Paraguay). Biochem (Mosc) 2013; 78(9):1023-32. Conclusion The mechanisms, genetically determined and regulated, here summarized, clearly cause the age-related progressive deterioration of all functions, namely aging. They are predicted by the New Paradigm and indeed are essential for its validity. On the contrary, they are not expected by the Old Paradigm and are in complete contrast with it. The explanation of aging through the New Paradigm allows: - A rational and consistent interpretation of all the manifestations of aging; - The prospect of being able to change and obtain a full control of aging through scientific procedures which are technically feasible [1,2]. [1] Libertini G. Prospects of a Longer Life Span beyond the Beneficial Effects of a Healthy Lifestyle, Ch. 4 in Handbook on Longevity: Genetics, Diet & Disease, Nova Science Publishers Inc., New York 2009. [2] Libertini G. The Role of Telomere-Telomerase System in Age-Related Fitness Decline, a Tameable Process, in Telomeres: Function, Shortening and Lengthening, Nova Sc. Publ., New York 2009. Conclusion (continued) The exposition and discussion of this last prospect, already briefly expounded elsewhere [1], is however outside and beyond the limits of time and of topic of this oral presentation. I do only dare to say: The possibility of an unlimited lifespan: - until now was excluded by prejudices, - today is a choice, - tomorrow will be restrained by the ability to endure an unlimited life. [1] Libertini G. Prospects of a Longer Life Span beyond the Beneficial Effects of a Healthy Lifestyle, Ch. 4 in Handbook on Longevity: Genetics, Diet & Disease, Nova Science Publishers Inc., New York 2009. This presentation is on my personal pages too: www.r-site.org/ageing. (e-mail: giacinto.libertini@tin.it) Thanks for your attention