eLearning PowerPoint Template
advertisement

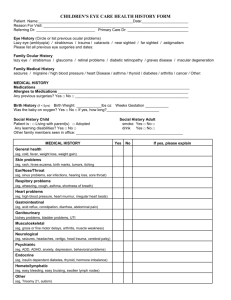
Pediatric Ophthalmology Julie M. Lange, MD Assistant Professor Division of Pediatric Ophthalmology Julie.Lange@osumc.edu Primary Learning Objective Recognize important preventable and treatable causes of blindness or vision loss in infants and children Secondary Learning Objectives define strabismus define amblyopia identify causes of amblyopia define esotropia and exotropia define suppression understand the basis for treatment of amblyopia, strabismus and refractive error in childhood Secondary Learning Objectives (continued) interpret tests of ocular alignment including corneal light reflex and cover-uncover testing recognize pseudostrabismus interpret abnormalities of the red reflex describe retinopathy of prematurity recognize ophthalmologic features of child abuse list common causes of leukocoria identify abnormal ocular motility disturbances presenting in childhood Red Reflex testing This is a basic test easily done by any practitioner. A direct ophthalmoscope is used to assess the red reflex in each eye. The examiner is looking for any opacities, irregularities or asymmetries in the red reflex. ANY abnormality needs to be referred to an ophthalmologist. Examples of abnormal red reflexes Retinoblastoma Cataract Congenital polar cataract dislocated lens Anisometropia: unequal refractions Vision Screening Terminology “Blinks to Light” “Fix and Follow” Children’s Figures HOTV chart Snellen chart Vision Screening Terminology Blinks to Light This term is used mostly to describe vision in newborn eye exams. An infant is expected to blink to light at birth, but does not usually show consistent fixation behavior until 2-3 months of age. Fix and Follow • By 4 months of age, most infants will fixate on an object and be able to follow it. • When checking fixation, have the patient fixate on an object with 1 eye at a time. It is best to use an object, rather than a light, to test vision because even a person with low vision can sometimes see lights well. Vision Screening Terminology Children’s Figures A chart consisting of pictures such as a hand and a car which are familiar to most children. Because the objects have very different shapes and are easily differentiated, this chart is not ideal. HOTV Chart A chart consisting of only 4 letters (H, O, T, V). It is often used in conjunction with a hand-held chart which the child can point to in order to indicate the letter on the wall chart. This is useful in preverbal children and in those who do not yet know the alphabet. Vision Screening Terminology Snellen Chart Snellen refers to the traditional eye chart consisting of a variety of letters which is read aloud. This is the most accurate chart to use, but its use is obviously limited by the age and literacy of the child. Refractive Error Every child has a refractive error. If the refractive error is high, glasses are warranted. Children have the ability to accommodate much more than adults, therefore small amounts of symmetric hyperopia are not corrected. Also, small amounts of myopia are not usually corrected due to the fact that the majority of a child’s daily activities are near tasks. Glasses can be given as early a 6 months old and can prevent and/or treat amblyopia. Amblyopia= less than normal best-corrected vision in 1 or both eyes. Causes include: Large refractive error in both eyes Difference in refractive error between the 2 eyes is called anisometropia. The more blurred eye will actually lose vision because the child starts to prefer the better seeing eye and only continues to develop vision in that eye. Strabismus or misalignment of the eyes. The child will prefer 1 eye while the more frequently deviated eye will lose vision. This is done to avoid diplopia which is inevitably the result if the eyes are misaligned. Structural abnormality of the eye can prevent a clear image and therefore proper visual development (cataract, corneal opacity, vitreous opacity, etc.) Amblyopia Treatments The first step is to put the child in the proper glasses if a significant refractive error exists Patching of the better seeing eye several hours per day in order to force the use of the weaker eye Cycloplegic eye drops can be used to blur the better seeing eye temporarily In cases of a structural abnormality, it is sometimes possible to address the problem directly (cataract surgery, corneal transplant, etc.) These patients often need patching after their surgery as well. Amblyopia Treatments Amblyopia treatments work best when implemented early. Around the age of 9 years old, a child’s bestcorrected vision is cemented. If not treated, amblyopia can cause blindness. If significant strabismus exists once equal vision is obtained, eye muscle surgery is warranted. Patching is the most common treatment for amblyopia Checking eye movements Oculomotor exam -Fixation with each eye individually -Range of movement of each eye -Steady? Look for nystagmus -Straight? Look for strabismus -Don’t forget to look at the pupils and eyelids Ocular motility disorders that may present in childhood Nystagmus Cranial Nerve 6 palsy Convergence Insufficiency Strabismus Esotropia Exotropia Hyper/Hypotropia Nystagmus Nystagmus is a term to describe fast, uncontrollable movements of the eyes. 1. Infantile: present at or soon after birth, can be associated with eye disease. Visual acuity in these patients is often nor correctable to 20/20. 2. Acquired: Secondary to medication Head injury Inner ear disorder Stroke B12 deficiency Multiple sclerosis Brain tumors Cranial Nerve 6 Palsy CN 6 controls the lateral rectus extraocular muscle In a CN6 palsy, there will be limitation to abduction in 1 or both eyes and a misalignment of the eyes in certain gazes This can be congenital or acquired It can be secondary to increased intracranial pressure or recent head trauma This warrants urgent referral to an ophthalmologist and/or ER Look for abnormal head positions This can indicate A null point for nystagmus An avoidance of diplopia in CN 6 palsy Eye preference in amblyopia Hypertropia in head tilts Strabismus Orthophoric: describes eyes that are aligned. Strabismus is a misalignment of the eyes. It can be constant or intermittent. Strabismus is not normal and should be taken seriously. Strabismus Esotropia (ET) eye drifts inward Exotropia (XT) eye drifts outward Corneal light reflex testing Assess alignment of eyes by having patient look at a penlight. The light reflex should fall within the pupil bilaterally. If the light reflex is asymmetric in 1 of the eyes, a misalignment may be present. The light reflex on the child’s left eye shows the eye is turned inward (esotropia) Orthophoric: eyes aligned Esotropia: L eye turned in Exotropia: L eye turned out Hypertropia: L eye drifted upward Alternate Cover Testing: 3 Steps to Detect Eye Deviation Step 1: The “Cover Test" Cover one eye while the patient fixates on an object (ie, toy, parent) During and after placement of the cover, the uncovered eye is observed for any movements that indicate the need to refocus. Alternate Cover Testing: 3 Steps to Detect Eye Deviation Step 2: The “Uncover Test" Cover one eye, but focus the examination on the covered eye once the cover is removed. If the justuncovered eye moves to regain focus, a strabismus is present. Alternate Cover Testing: 3 Steps to Detect Eye Deviation Step 3: The “Alternate Cover Test" Occlude each eye in an alternating manner. If the affected eye moves in an attempt to regain fixation, a strabismus is present. Cover Testing http://www.richmondeye.com/eyemotil.asp This is an interactive webpage where the user can cover and uncover the eyes on the screen to see fixation/refixation movements indicating strabismus. Pseudostrabismus A false appearance of strabismus. It is most commonly seen in infants and toddlers who have a wide nasal bridge or epicanthal folds. These facial features can partially cover the medial part of each eye giving the appearance that the eyes are crossed inward when actually upon testing, the eyes are orthophoric. Epicanthal folds causing pseudostrabismus Pseudoesotropia look at the light reflexes Pseudoesotropia When testing a child’s fixation. One should always be looking for eye preference. Children should be able to use either eye and not have a strong preference. If a preference is noted; this is a sign of amblyopia. When strabismus is present, preference is easier to assess. The examiner should make certain the child can fixate and maintain fixation with either eye. When strabismus is not present, the examiner must occlude each eye separately and test the fixation and ability to maintain fixation. Children who prefer one eye will strongly object to cover of that eye. Congenital Esotropia Congenital Esotropia Arises before 6 months of age Typical characteristics include: Large and constant alternating/cross fixation not significantly hyperopic, usually normal refractive error full abduction possible nystagmus, often the latent type Cross-fixation in congenital ET Esotropia Esotropia arising after 6 months of age is usually classified as accomodative or non accomodative. Accomodative: patient has a high hyperopic prescription and the eyes are aligned in glasses Non-Accomodative: patient has low refractive error and glasses do not significantly change the alignment. Esotropia Esotropia is often associated with amblyopia and needs be treated right away. ESOTROPIA Esotropia much improved in glasses. Therefore, this is Accomodative Esotropia. Bifocals are sometimes used to add more plus lenses to the bottom of the existing prescription to help with more esotropia at near. Exotropia: temporal deviation of the eyes XT Less risk of amblyopia Often begins as intermittent with some control Can progress and become more constant EXOTROPIA Exotropia Exotropia is sometimes helped my myopic (nearsighted) glasses, but large deviations usually require strabismus surgery to correct. Suppression If strabismus arises in a child with binocular vision, the child experiences diplopia. Therefore, the child will usually suppress one eye as an adaptation to avoid diplopia. This often leads to Amblyopia. Strabismus surgery Basic concept is to weaken or strengthen an eye muscle Methods to weaken: recess (move the insertion of a muscle posteriorly) insert a spacer into the muscle therefore effectively making the muscle longer Botox disinsertion Methods to strengthen: resect, tuck, advance Methods to weaken muscle: Recess: move the insertion of a muscle posteriorly insert a spacer into the muscle therefore effectively making the muscle longer botox disinsertion Methods to strengthen: resect: excise part of the muscle, thereby making it shorter Tuck: essentially folding a segment of muscle on itself and securing it in place, thereby tightening it Advance: moving the insertion anteriorly A recession (weakening) of the medial rectus is the surgery most often performed for the correction of non-refractive esotropia. It is done by disinserting the muscle from the globe and then reattaching it to the globe posterior to its original insertion. 1. An incision is made through conjunctiva and tenons fascia. The desired eye muscle is then located with a muscle hook. 2. Here the medial rectus muscle is isolated with a muscle hook and then cleared of connective tissue. 3. The muscle is then secured with a double armed suture just anterior to its insertion onto the globe. 4. The muscle is then excised from the globe with the sutures preventing loss of the muscle. 5. Calipers are then used to measure and mark a predetermined distance from the original insertion of the muscle. The muscle is then reattached to the globe using the double-armed suture already in place to make partial-thickness scleral passes at the marks made by the calipers. Suture are then tied and cut. The conjunctiva is re-approximated and sometimes sutured. The same procedure is often performed on the other eye. Strabismus Surgery Video http://webeye.ophth.uiowa.edu/eyeforum/video/PediatricOp hth-Strabismus-vids/medial-rectus-recession.htm Retinopathy of Prematurity Retinopathy of prematurity (ROP) is a potentially blinding eye disorder that primarily affects premature infants weighing 1500 grams or less or with a gestation of less than 30 weeks. ROP • Retinal blood vessels begin to develop approximately 3 months after conception and usually complete their development before the birth of a full term infant. • If an infant is born very prematurely, eye development is often not complete and the growth of the retinal vessels may be disrupted. The vessels may stop growing or grow abnormally from the retina into vitreous. These abnormal vessels are very fragile and bleed easily. Retinopathy of Prematurity ROP These babies are at high risk of retinal detachment. ROP can cause blindness. ROP exams are done on all babies who fall within the risk guidelines. Because there are no external signs of this diagnosis, parents need to be reminded of the importance of these exams. ROP Progression of ROP can lead to a retinal detachment. The scar tissue associated with the fibrovascular ridge contracts, pulling the retina away from the wall of the eye. Eyes with retinal detachments due to ROP are very difficult to operate on and these babies often have poor visual outcomes. Depending upon the stage and zone of the ROP, treatment may be indicated in an attempt to prevent vision loss. The gold standard treatment is laser. It is used to photocoagulate the avascular retina to eliminate the hypoxia which drives the abnormal vessel growth. Laser spots are applied confluently to the avascular retina between the ridge and the ora serrata. Over the last 5-6 years, physicians have begun injecting anti-VEGF molecules into the eyes of babies with severe ROP. Their retinal vascular abnormalities often significantly improve after the injection. This is an offlabel use of intravitreal bevacizumab. This drug is most commonly used for exudative macular degeneration. However, there are still many questions surrounding bevacizumab It has many potential side-effects and our understanding of the short- and long-term effects of VEGF inhibition in newborns is extremely limited. The implications of VEGF blockade in an infant in whom physiologic VEGF is required for normal organogenesis are not known. Leukocoria Leukocoria, literally "white pupil”, occurs when the pupil is pale yellow or white rather than the usual black Common Causes of Leukocoria cataract retinal detachment retinopathy of prematurity retinal malformation intraocular infection (endophthalmitis) retinal vascular abnormality intraocular tumor (retinoblastoma). Retinoblastoma Most common primary intraocular malignancy of childhood 1/15,000 live births 3% of all childhood cancers RB Retinoblastoma is a rare type of eye cancer that arises from the retina and develops in early childhood. In most children with retinoblastoma, the disease affects only one eye. However, 1 out of 3 children with retinoblastoma develops cancer in both eyes. The most common first sign is leukocoria. This white reflex is often noted in photographs. Other signs of retinoblastoma include strabismus, eye pain, and eye inflammation If diagnosed early, retinoblastoma is often curable. However, if not treated promptly, it can spread beyond the eye to other parts of the body and be life-threatening RB When retinoblastoma is associated with a gene mutation that occurs in all of the body's cells, it is known as germinal retinoblastoma. People with this form of retinoblastoma have an increased risk of developing other life-threatening cancers such as pinealoma, osteosarcoma, and melanoma. Endophytic RB grows from retina into vitreous causing vitreous seeds Exophytic RB grows outward from retina resulting in a mass beneath the retina Presentation of Retinoblastoma 60% leukocoria 20% strabismus Chronic uveitis Child Abuse Suspicion should be aroused when apparently traumatic physical exam findings do not match with the history given by the caretaker (like multiple fractures on the face and head after a single short fall). Also, if the history does not match the developmental age of the child (like a 1 month old rolling off a bed or a 8 month old climbing out of a crib or high chair). Any physician who suspects abuse may have occurred is required by law in every U.S. state to report it to the proper authorities. Ocular Signs of Child Abuse hyphema Characteristic petal-shaped cataract from trauma Subconjunctival hemorrhage Shaken Baby Syndrome (Abusive Head Trauma) • Shaken baby syndrome (SBS) is a triad of medical symptoms: 1. subdural hematoma 2. retinal hemorrhage 3. brain swelling • • These findings lead doctors to infer child abuse caused by intentional shaking. In a majority of cases there is no visible sign of external trauma. Shaken Baby Syndrome (Abusive Head Trauma) • SBS is often fatal and can cause severe brain damage, resulting in lifelong disability. • Estimated death rates (mortality) among infants with SBS range from 15% to 38%. Up to half of deaths related to child abuse are reportedly due to shaken baby syndrome. • Nonfatal consequences of SBS include varying degrees of visual impairment (including blindness), motor impairment (e.g. cerebral palsy) and cognitive impairments. Extensive retinal hemorrhages found in multiple layers of the retina and in all 4 quadrants. A large schisis cavity (hemorrhagic cyst) is seen overlying the • A child with abnormal eye findings should have a dilated eye examination. • It is safe to dilate a baby’s eyes at any age. Thank you for completing this module Questions? Contact me at: Julie.Lange@osumc.edu Survey We would appreciate your feedback on this module. Click on the button below to complete a brief survey. Your responses and comments will be shared with the module’s author, the LSI EdTech team, and LSI curriculum leaders. We will use your feedback to improve future versions of the module. The survey is both optional and anonymous and should take less than 5 minutes to complete. Survey