Cardiac Rehabilitation

Benefits of Cardiac Rehabilitation:
Impact on Mortality, Hospitalizations and Risk Factors
Reggie Higashi, MSS
Exercise Physiologist
Core Program Components
• Baseline clinical evaluation & patient assessment
• Risk factor management and goal setting
• Psychosocial management
• Physical activity counseling
• Exercise training
Balady, G. et al. Core components of cardiac rehabilitation/secondary prevention programs: A statement for healthcare professionals from the American Heart
Association and the American Association of Cardiovascular and Pulmonary
Rehabilitation. Circulation , 2000; 102:1069-1073.
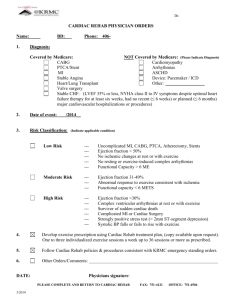
Approved Diagnoses
(Medicare)
• Myocardial infarction
– Within 1 year
• Stable angina
• Coronary artery bypass grafting
– Within 1 year
Ref: Section 35:25 of the "Medicare Procedure Manual"
Cardiac Rehabilitation Programs
Approved Diagnoses
(Non-Medicare)
• Myocardial infarction
• Stable angina
• CABG
• PTCA/Stent placement
• Heart failure
• PAD
• Recent ICD implant
• Arrhythmias
• Valve replacement/repair
• Heart transplant
Cardiac Rehab Programs
• Monitored outpatient program
– 3 days/week for up to 12 weeks
– Covered by Medicare (MI, angina, CABG)
• Modified monitored outpatient program
– 3 days/week for up to 4 months
– Not covered by insurance
• Extended outpatient program (after monitored or modified program)
– 3 days/week for up to 4 months
– Not covered by insurance
• Maintenance program (after extended program)
– 2 days/week
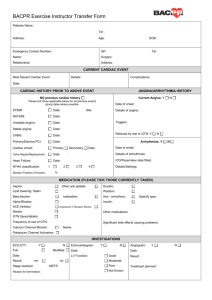
Monitored Outpatient Program
• One hour cardiac monitored exercise sessions
• 3 days/week, MWF for up to 12 weeks
• Various class times in morning and afternoon
• Guided warm-up, three 10-minute aerobic stations, guided cool-down
• Blood pressure monitored pre, during and post-exercise
• Monthly and final reports sent to referring
M.D.
• Medicare/Insurance covered diagnoses (MI,
CABG, Stable Angina)
Modified
Monitored Outpatient Program
• Telemetry monitored for first 2 weeks, then patient is placed on personal heart rate monitor for the remainder of program
• 3 days/week, MWF for up to 4 months enrollment limit
• Various class times in morning and afternoon
• Guided warm-up, three 10-minute aerobic stations, guided cool-down
• Blood pressure monitored pre, during and post-exercise
• Monthly and final reports sent to referring M.D.
• Costs: $325 for initial month (includes costs of personal heart rate monitor) then $40 per month for the remaining
3 months.
• (Self-Pay; Not covered by insurance)
Extended Outpatient Program
• One hour non cardiac-monitored exercise sessions
• 3 days/week, MWF for up to 4 months enrollment limit
• Various class times in morning and afternoon
• Guided warm-up, three 10-minute aerobic stations, guided cool-down
• Blood pressure monitored pre, during and post-exercise
• Cardiac monitoring 1x/month
• Monthly reports with telemetry cardiac monitoring sent to referring M.D.
• Self Pay: $40/month (Not covered by insurance)
– Must complete monitored or modified monitored program to enroll in this program.
Maintenance Program
• One hour non cardiac-monitored exercise sessions
• 2 days/week, Tu & Th, 8:00 a.m. - 9:00 a.m.
• Guided warm-up, four 10-minute aerobic stations, guided cool-down
• Blood pressure monitored 1x/month as as needed
• Heart Rate checks pre, during and post-exercise by patient
• Copy of monthly exercise logs given to patient.
• Self Pay: $30/month (not covered by insurance)
– Must complete extended out-patient program to enroll in this program.
Effect of Exercise-Based Cardiac Rehab on Cardiac Events in Patients with CAD
(MI, angina, CABG, PCI)
Exercise
Only
Non-fatal MI - 4%
Cardiac
Mortality
- 31% *
Comprehensive
Program
- 12%
- 26% *
Jolliffe et al. Meta-Analysis, 2001.
51 randomized, controlled trials (n = 4,000)
2 –6 months of supervised rehab, then unsupervised
Mean follow-up of 2 – 4 years
Utilization of Cardiac Rehab by
Patients After MI
• Ades et al , 1992 reviewed utilization of cardiac rehab by patients within 1 hour of rehab center
• Age Dependence of Utilization
– < 62 yrs: 46% utilization
– > 62 yrs: 21% utilization
– Most powerful predictor of utilization was recommendation of primary care physician to participate
Potential Explanation for Reduced
Mortality Without Impact on Non-fatal MI
• Ischemic preconditioning
– Animals having repeated episodes of temporary coronary occlusion have smaller MI when occlusion is permanent
• Electrical stability and reduced ventricular fibrillation
Exercise Training in Patients with Angina
• Improved myocardial oxygen supply at a given level demand
– Increase in rate pressure product at onset of angina (reduction in exercise heart rate)
– Decrease in nuclear scan perfusion defects (as early as 8 weeks)
– Less ST segment depression
• Proposed mechanisms
– Improved endothelial function (angio studies)
– Increased coronary collaterals
– Regression and reduction in progression of CAD
(1 yr studies)
Exercise Training After Coronary
Revascularization (CABG/PCI)
• No large studies
• ETICA Trial (Exercise Training Intervention after
Coronary Angioplasty Trial, 2001
• 118 patients underwent 6 months of exercise training or control. Follow-up of 33 + 7 months
• Improved exercise capacity (26% increase in v02)
• Fewer cardiac events (12 vs 32%)
• Fewer hospital admissions (19 vs. 46%)
• No impact on restenosis
Exercise Training for Patients
With CHF
• > 20 studies document improvements in
– Exercise capacity
• 20% improvement in v02 after 4 weeks
• 18 – 34% increase in time on treadmill after 12 wks
– Quality of life
• Hospitalization and mortality
– Belardinelli et al (Circ, 1999): Small trial that demonstrated improved exercise capacity, decreased hospitalization and improved 1 yr survival
– HF-ACTION – NIH Study
• Compares “usual care” with addition of formal exercise training
• Endpoints of mortality and hospitalization
Exercise Training for Patients with PAD and Claudication
• Improvements in distance to onset of pain
(increased by 179% [225 m]) and distance to maximal tolerated pain (increased by
122% [397 m])
• Improvements with exercise exceed those with meds (I.e., Trental, Pletal)
• Most significant improvements when:
– Walking as training
– Walking to maximal pain
– Training period for 6 months
Meta-Analysis of 21 exercise programs
Gardner and Poehlman, JAMA, 1995
Proposed Mechanisms for Improved
Outcomes with Exercise Therapy
• Favorable impact on risk factors
– Lipids
– Blood pressure
– Body weight
– Insulin sensitivity
• Enhanced parasympathetic tone
• Improved endothelial function
• Lower catecholamine levels with exercise may reduce platelet aggregation
Impact on Risk Factors:
Cholesterol Reduction
• LDL decrease of 5% (8 – 12% decrease with combined exercise and diet therapy)
• HDL increase of 4.6%
• Triglyceride decrease of 3.7%
Meta-Analysis (2001) of 52 trials, n = 4700, > 12 weeks of training
Impact on Risk Factors:
Diabetes Mellitus
• Decrease in hemoglobin A1C by 0.5 to 1.0
– Mechanisms proposed: Increased insulin sensitivity and decreased hepatic glucose production
– Data from 9 trials, 337 patients with diabetes mellitus, type 2
• Role of physical activity and weight loss * in preventing type 2 diabetes mellitus in patients at risk
– Diabetes Prevention Program (NEJM, 2002)
– 58% reduction in onset of diabetes over 2.8 years
(vs 31% reduction with metformin 850 mg BID)
* Average weight loss of 4.4 kg
Increase activity by 8 met hr/week = 6 mile walk per week
Impact on Risk Factors:
Blood Pressure Reduction
Systolic
Overall Normotensive Hypertensive
- 3.4
Diastolic - 2.4
-2.6
- 1.8
- 7.4
- 5.8
44 Trials, n = 2,674
Impact on Risk Factors:
Smoking
• Useful as adjunct to behavioral programs
• Results of 12 week exercise program in
281 women
– 19% abstain after program (vs 10%)
– 12% abstain at 1 year (vs 5%)
Impact on Risk Factors:
Weight Reduction
Exercise
Diet
2 – 3 kg
5 – 5 ½ kg
Diet and Exercise 8 ½ kg
Favorable Effects of Exercise Training
• Endothelial Function
• Fibrinolytic System
• Platelet Function
Exercise Therapy and
Platelet Function
• An increase in platelet aggregation can occur after exercise in sedentary individuals
(possibly related to increased catecholamines)
• After 12 week exercise training program, platelet aggregation decreased by 52% in a study of middle age, hypertensive male subjects
Exercise Therapy and
Fibrinolytic System
Plasma Fibrinogen
Tissue Plasminogen
Activator
Plasminogen activator inhibitor - 1
- 13%
+ 39%
- 58%
Summary:
Benefits of Exercise-Based Cardiac Programs
• 30% decrease in mortality in patients with
CAD (Decrease in mortality also reported in CHF)
• Decrease in hospitalizations after coronary revascularization and with CHF
• Improved exercise tolerance in patients with claudication and PAD
• Favorable impact on risk factors
Exercise Recommendation
(AHA/CDC/ACSM)
• 30 minutes or more of moderate intensity of physical activity on most (preferably all) days of the week
• Moderate intensity
– Absolute intensity = 4 – 6 mets *
– Relative intensity = 40 – 60% of v02 max
•4 mets may be “vigorous” for an 80 yr old and
• “light” for a 20 yr old