Male Obesity and Semen Analysis Parameters
advertisement

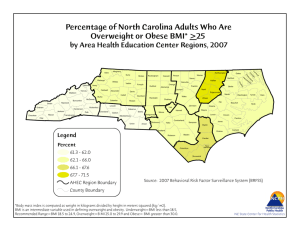
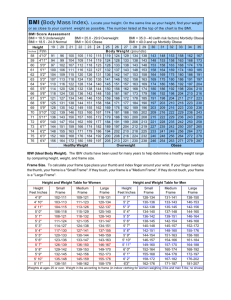
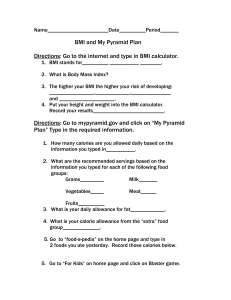
Male Obesity and Semen Analysis Parameters Joseph Petty, MD Samuel Prien, PhD Amantia Kennedy, MSIV Sami Jabara, MD Background: Obesity • Obesity is a growing problem. • The Behavioral Risk Factor Surveillance System, in conjunction with the CDC, conducted a national survey and found that in 2000, the prevalence of obesity (BMI >30 kg/m2) was 19.8%, a 61% increase since 1991. Background: Obesity • Obesity affects female and male fertility. • In a study comparing IVF success rates and female obesity, it was shown that a 0.1 unit increase in waist-hip ratio led to a 30% decrease in probability of conception per cycle 2. • In couples complaining of infertility, male factor plays a role in up to 40% of cases. Background: Semen Parameters • What parameters best predict fertility? • National Cooperative Reproductive Medicine Network: 765 infertile couples (no conception after 12 months), and 696 fertile couples • greatest discriminatory power was in the percentage of sperm with normal morphologic features. Hypothesis • Since there is an observed correlation between obesity and male factor infertility, our hypothesis is that an increased BMI is associated with higher rate of abnormal semen parameters, especially sperm morphology. Recent Studies • Danish study by Jensen et al. enrolled 1,558 young men (mean 19 years old) when they presented for their compulsory physical exam as part of their country’s military drafting system. • The authors showed decreased sperm counts and concentration (39 million/mL vs. 46million/mL) in those with an elevated BMI (>25kg/m2). They did not, however, observe a difference in morphology. • Hormonal differences Recent Studies • Kort et al. looked at semen analysis results in 520 men • grouped according to their BMI, and measured the average normal-motilesperm count (NMS = volume x concentration x %motility x %morphology) • Kort concluded that men with high BMI values (>25) present with few normalmotile sperm cells Recent Studies • Hammoud et al., showed a increased incidence of oligospermia and increased BMI and also showed decreased levels of progressively motile sperm • Considered each parameter separately. Sexual function • Agricultural study: The association between BMI and infertility was similar for older and younger men, disproving the theory that erectile dysfunction in older men is a significant factor. • Hammoud et al., though primarily concerned with hormones, looked at erectile dysfunction directly and showed that there was no correlation with increases in BMI • Nguyen et al., effect of BMI is essentially unchanged regardless of coital frequency, suggesting that decreased libido in overweight men is not a significant factor Hormonal Profile • Danish study, observed decreased FHS and inhibin B levels in the obese. • Pauli et al., observed with increases in BMI a decreased total T, decreased SHBG, increased estrogen and decreased FSH and inhibin B. • Inhibin B, cited for its usefulness as a novel marker for spermatogenesis and its role in pituitary gonadotropin regulation. • Pauli: no correlation of BMI or skinfold thickness with semen analysis parameters, though it was observed that men with proven paternity versus those without had lower BMI. Interventions: Gastric Bypass • One case series of 6 male patients after bariatric surgery showed secondary azoospermia with complete spermatogenic arrest. • none of the subjects had a semen analysis before the bariatric surgery, but all had fathered a pregnancy previously • malabsorption of nutrients Interventions • Hammoud et al., part of Utah Obesity Study • effect of the gastric bypass surgery on sex steroids and sexual function • Cohort of 64 severely obese men • Along with a significant decrease in BMI, they found decreased levels of estradiol, and increases in total and free testosterone along with a reported improvement in quality of sexual function. • Semen analysis parameters were not considered in this study Study Design • Retrospective chart review for all couples and individual patients presenting for an infertility consultation and evaluation at the Texas Tech Physicians Center for Fertility and Reproductive Surgery from September 2005 through January 2008. • Intake questionnaire: demographic, medical, surgical and fertility history. Questionnaire • Previous pregnancies fathered: current or previous partner • Psychiatric disorders included any degree of depression, bipolar disorder or any other psychiatric disorder requiring medical therapy. • Tobacco and alcohol users: whether they admitted to light, moderate, or heavy use, patient underreporting. • Chemical exposures: contact with pesticides, herbicides, and heavy metals. • Sexual dysfunction: mainly erectile dysfunction and decreased libido. • Genitourinary anomalies: hypospadias, varicocele, genitourinary surgery, testicular torsion or inguinal hernia or trauma • Other medical problems included mainly diabetes, hypertension, thyroid disease, autoimmune disease, and cancer. Study Design • Patients grouped according to their BMI as normal (2024 kg/m2, N = 24), overweight (25-30 kg/m2, N = 43), or obese (>30 kg/m2, N = 45), as standardized by the World Health Organization • Semen analysis parameters: morphology, volume, concentration, percent motility, and presence of absence of agglutination, in accordance with World Health Organization (WHO) guidelines • SPSS statistical software was used to run analysis of variance (ANOVA) and post-hoc Tukey HSD tests between the groups. A p-value <0.05 was considered statistically significant. Exclusion Criteria • questionnaire was missing or if they had an otherwise incomplete chart. • missing vital statistics (i.e. height and weight), • 235 total charts reviewed, – 60 no semen analysis or outside lab. – 63 patients had either missing vital statistics or a missing questionnaire – This left a total of 112 patients with valid data to be considered. Results The BMI groups were statistically similar as far as demographic characteristics and confounding variables Background Variables 70 60 Percent 50 40 Group 1 30 Group 2 20 Group 3 10 33 ) ) (1 lp ro b. ( n To xi ed ic a ge ry (1 4) M U G U G Su r al y om an SD (7 (8 ) ) 1) (6 Al c 3) (2 (8 To b ch Ps y v. Pr eg (3 8) ) 0 Pr e • Group 1 = normal BMI; Group 2 = overweight; Group 3 = obese Results • There was no statistically significant difference between the semen parameters of all three BMI groups. Variable Morph. (%) Vol (mL) Motility (%forward) Agg (% with) Conc. (mil./mL) norm value >30 >2 >50 none >20 BMI Groups (means) 1(N=24) 2(N=43) 3(N=45) P value 27.6 34.1 28.1 0.083 3.6 3.3 3.4 0.845 42.3 52.7 46 0.06 12 7 7 0.668 136.1 87.5 64.3 0.18 25 20 15 10 5 0 Results • slight trend towards a decreasing sperm 1 2 3 concentration with increases in BMI BMI Groups Trend in Concentration 160 million / mL 140 136.1 120 87.5 100 80 64.3 60 40 20 0 1 2 3 Conclusion • In this study, overweight and obese men did not have an increased rate of teratozoospermia, asthenospermia, or oligospermia. Discussion • • • • Inconsistencies Small sample size Kort and data interpretation Change the normal hormonal milieu, addressed by Jensen study. • Sertoli cell function, increased aromatase, role of leptin • Aggerholm study: altered hormones not correlated with semen abnormalities in overweight men (25.1-30.0 kg/m2), slightly decreased sperm concentration in overweight but not in obese Future Studies • What affects morphology specifically? – – – – Hormones Result of secondary disease, i.e.. Diabetes Genetic mutations Weight loss surgery and other interventions • Overall, there is no doubt that increases in BMI have a detrimental effect on male fertility, but a satisfactory explanation of the mechanism for this phenomenon has yet to be given. References • • • • • • • • 1. Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA 2001;286:1195–200. 2. Zaadstra BM, Seidell JC, Van Noord PA, te Velde ER, Habbema JD, Vrieswijk B, Karbaat J. Fat and female fecundity: prospective study of effect of body fat distribution on conception rates. Br Med J 1993;306:484–7. 3. Thonneau P, Marchand S, Tallec A, Ferial ML, Ducot B, Lansac J, Lopes P, Tabaste JM, Spira A. Incidence and main causes of infertility in a resident population (1,850,000) of three French regions (1988-1989). Hum Reprod 1991;6(6):811-6. 4. Guzick DS, Overstreet JW, Factor-Litvak P, Brazil CK, Nakajima ST, Coutifaris C, Carson SA, Cisneros P, Steinkampf MP, Hill JA, Xu D, Vogel DL; National Cooperative Reproductive Medicine Network. Sperm morphology, motility, and concentration in fertile and infertile men. N Engl J Med 2001;345(19):1388-93. 5. Jensen TK, Andersson AM, Jørgensen N, Andersen AG, Carlsen E, Petersen JH, Skakkebaek NE. Body mass index in relation to semen quality and reproductive hormones among 1,558 Danish men. Fertil Steril 2004;82(4):863-70. 6. Kort HI, Massey JB, Elsner CW, Mitchell-Leef D, Shapiro DB, Witt MA, Roudebush WE. Impact of body mass index values on sperm quantity and quality. J Androl 2006;27(3):450-2. 7. Hammoud AO, Wilde N, Gibson M, Anna Parks, Carrell DT, Meikle AW. Male obesity and alteration in sperm parameters. Fert Ster 2008;90(6):2222-2225 altered serum sex hormone profile? Fertil Steril. 2008 Sep;90(3):619-26. Ref. cont. • • • • • • • • • 8. Sallmén M, Sandler DP, Hoppin JA, Blair A, Baird DD. Reduced fertility among overweight and obese men. Epidemiology 2006 Sep;17(5):520-3. 9. Nguyen RH, Wilcox AJ, Skjaerven R, Baird DD.Men's body mass index and infertility. Hum Reprod. 2007 Sep;22(9):2488-93. 10. Pauli EM, Legro RS, Demers LM, Kunselman AR, Dodson WC, Lee PA. Diminished paternity and gonadal function with increasing obesity in men. Fertil Steril. 2008 Aug;90(2):346-51. 11. Di Frega AS, Dale B, Di Matteo L, Wilding M. Secondary male factor infertility after Roux-en-Y gastric bypass for morbid obesity: case report. Hum Reprod 2005;20:997–8. 12. Hammoud A, Gibson M, Hunt SC, Adams TD, Carrell DT, Kolotkin RL, Meikle AW. Effect of Roux-en-Y Gastric Bypass Surgery on the Sex Steroids and Quality of Life in Obese Men. J Clin Endocrinol Metab. 2009 Jan 27. [Pub Med Epub ahead of print] 13. World Health Organization, Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation, WHO Consultation on Obesity, Geneva, Switzerland, 1999. 14. World Health Organization. Laboratory Manual for the Examination of Human Semen and Sperm-Cervical Mucus Interaction. Cambridge University Press, 1999. 15. Winters SJ, Wang C, Abdelrahaman E, Hadeed V, Dyky MA, Brufsky A. Inhibin-B levels in healthy young adult men and prepubertal boys: is obesity the cause for the contemporary decline in sperm count because of fewer Sertoli cells? J Androl 2006;27(4):560-4. 16. Aggerholm AS, Thulstrup AM, Toft G, Ramlau-Hansen CH, Bonde JP. Is overweight a risk factor for reduced semen quality and altered serum sex hormone profile? Fertil Steril. 2008 Sep;90(3):619-26. THANK YOU