GHChapterDraft - Hormone Restoration
advertisement

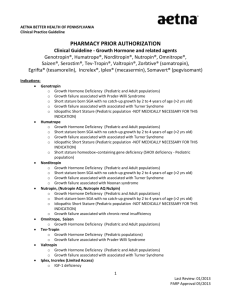
Rough Draft: Growth Hormone Deficiency 1. Introduction Borges last Growth Hormone secretion and the level of a major product of growth hormone in our blood, IGF-1, decline 14% per decade of life. This loss, like the loss of other vital hormones with age, is detrimental to our health and quality of life. By the age of 40 or 50, many people have relatively low IGF-1 levels--equal to people who have damaged pituitary glands and no GH production at all. Growth hormone stimulates cell division, cell growth, and protein production throughout the body, helping to maintain all tissues. Growth hormone deficiency shares many features with normal aging and therefore it's logical to assume that the loss of GH with age contributes to the declines seen with aging. Many studies have shown growth hormone is essential to the maintenance of our nervous system, immune system, bones, metabolism, and muscles. Higher, rather than lower IGF-1 levels within the reference ranges reduce abdominal fat, blood sugar, and blood pressure. Higher IGF-1 levels decrease the risk of a heart attack. GH replacement improves mood and sociability.Growth hormone levels cannot be directly measured because it's produced only during the night while we are in deep sleep. However, growth hormone secretion can be measured using the IGF-1 level in the blood. It is a reliable test: only liver disease or a rare genetic defect can cause a low IGF-1 level in the face of adequate growth hormone secretion. Some medical authorities are now trying to restrict adult GH replacement to those extreme cases where persons have obvious physical damage to their pituitary gland and &nbsp;cannot make any GH even when forced to do so with superphysiological stimuli like insulin or arginine stimulation tests. This policy is unscientific, as a “normal”; response to such tests does not guarantee that enough GH is actually being secreted on a daily basis. The best indicator of actual GH secretion under normal circumstances in any person is the IGF-1 level.Growth hormone restoration, like testosterone restoration, is controversial today only because athletes are using and abusing it for performance gains, and because most of the early studies of GH replacement in older adults used grossly excessive doses that produced elevated blood sugar, fluid retention, and aching joints. Dr. Lindner, prescribes GH only to those with symptoms and relatively low IGF-1 levels who thereby demonstrate evidence of growth hormone deficiency. He uses low, physiologic doses that have been shown to produce benefits without causing signs or symptoms of excess. Unfortunately, GH is not covered by insurance, is expensive (a moderate dose costs $200/mo), and requires nightly self-injections. There is evidence that GH deficiency as defined in terms of a low insulin-like growth factor-1 (IGF-1) level occurs in approximately 30% of patients with fibromyalgia and is probably the cause of some morbidity. It seems most likely that impaired GH secretion in fibromyalgia is related to a physiologic dysregulation of the hypothalamic-pituitary-adrenal axis (HPA) with a resulting increase in hypothalamic somatostatin tone. It is postulated that impaired GH secretion is secondary to chronic physical and psychological stressors. It appears that impaired GH secretion is more common than clinically significant GH deficiency with low IGF-1 levels. The severe GH deficiency that occurs in a subset of patients with fibromyalgia is of clinical relevance because it is a treatable disorder with demonstrated benefits to patients.1 Optimal level of other hormones can increase GH secreation and IGF-1 levels including progesterone during the luteal phase. 2,3 2. The Importance of Optimal GH/IGF-1 Levels The declining activity of the GH/IGF-I axis with age contributes to the negative changes in body composition, structure, function and metabolism. Treatment with rhGH restores plasma IGF-I levels, increases lean body mass and muscle strength while decreasing adipose tissue mass in healthy elderly subjects. Interestingly, it has been shown that the decline in IGF-1 with age is caused by a decline in GH secretion, as elderly people have the same increase in IGF-1 with a given high dose of GH as do younger adults. So older person retain their sensitivity to GH, they simply make much less if it. 4 GH-deficient adults have many negative changes in their bodies. Body fat percentage, LDL cholesterol, blood glucose and insulin levels are all increased. Bone density is significantly lower and blood pressure is higher. GH deficiency increases a number of cardiac risk factors; it increases abdominal fat, lowers cardiac ejection volume and the distensibility of the arteries. It raises total cholesterol and LDL cholesterol and the levels of inflammatory markers such as C-reactive protein. GH therapy lowers total and LDL cholesterol by 10 to 20% and lowers CRP. GHD patients have higher fibrinogen levels—a sign of increased tendency to form blood clots.5 5 years of gGH therapy in GH-deficienct adults reduced visceral fat, cholesterol, and actually reduced the thickness of the carotid artery intima—a direct measure of atherosclerosis.6 The degree of IMT in normal controls was found to be related more strongly to lower IGF-1 levels than to higher LDL cholesterol levels, and persons with low IGF-1 levels have lower HDL cholesterol, higher glucose, insulin, fibrinogen levels.7 In a large group of “healthy” persons, having levels of IGF-1 that were lower within the range was associated with higher blood pressure, impaired glucose tolerance, and diabetes.8 Lower IGF-1 levels within the “normal” range, and higher levels of IGF1BP3 that binds IGF-1 in the serum are independent predictors of later ischemic heart disease. The importance of free IGF-1 levels is similar in magnitude to well-known risk factors like cholesterol levels and blood pressure.9 In elderly persons, a lower IGF-1 is associated with a higher risk of death from ischemic heart disease.10 In elderly persons, those with IGF-1 levels above the median of 140mcg/dL had half the risk of heart failure as those with levels below 140mcg/dL.11 Adults with IGF-1 levels in the bottom quartile (72mcg/dL) had twice the risk of ischemic stroke as those with levels in the top quartile (125mcg/dL).12 GH replacement therefore appears necessary to prevent atherosclerosis, insulin resistance, and osteoporosis. 13 GH replacement has favourable cardiovascular and renal effects including increase of stroke volume and glomerular filtration rate with reduction of peripheral resistance.14 IGF-1 functions as putative regenerative agent in the adult brain. GH may act directly in the brain without the intervention of IGF-1. GH and IGF-1 are neuroprotective in various experimental models of brain injury. IGF-1 increases the formation of new nerve cells in the hippocampus, a region specialized in short term memory. GH 15 GH replacement for 6 months in deficient persons resulted in improved long-term and short-term memory function, and the effects were even visible using a functional MRI.16 The fall in IGF-I levels with aging correlates with cognitive decline and it has been suggested that IGF-I plays a role in the development of dementia. IGF-I is highly expressed within the brain and is essential for normal brain development. IGF-I has anti-apoptotic and neuroprotective effects and promotes projection neuron growth, dendritic arborization and synaptogenesis. Collectively, these data are consistent with a causal link between the age-related decline in GH and IGF-I levels and cognitive deficits in older persons.17 The replacement of GH in GH-deficient persons who already have some degree of central hypothyroidism (weak TSH production) can lower TSH secretion further leading to a decline in thyroid hormone levels. 18 Growth hormone administered to men with adult-onset growth-hormone deficiency at a dose adjusted to high-RR serum IGF-1 levels increases bone density and stimulates bone turnover, decreases body fat and increases lean mass, and is associated with a low incidence of “side effects”.19 The beneficial effect of GH replacement on bone mass persists for at least 18 months after replacement is discontinued.20 GH is essentially reversing the changes seen in older adults due to their loss of GH secretion. 3. The Diagnosis of Growth Hormone Deficiency A normal IGF-1 level does not rule out GH deficiency as the low end of laboratories’ “normal” range includes persons with IGF-1 levels similar to those with obvious GH deficiency (demonstrated by known pituitary damage and inadequate response to GH stimulation testing. As many as half the adults with severe GHD have IGF-1 values within the laboratory’s “normal” range. Whereas Labcorp’s IGF-1 ranges for a 51-55yo male or female are 87-238ng/ml, many GH-deficient persons have IGF-1 levels as high as 110ng/ml. Standard GH diagnosis guidelines are illegitimitely restrictive. They restrict the diagnosis to those persons who have known pituitary damage, a low-IGF-1, and fail a GH stimulation test. Such guidelines fail to diagnose any lesser degree of GH deficiency, and particularly the dysfunctional GH secretion that causes suboptimal IGF-1 levels in many persons in the absence of pituitary disease. At present the gold standard is the insulin stress test (IST)which is unpleasant and potentially dangerous, particularly in patients with hypopituitarism. Insulin is injected to lower the person’s blood sugar to dangerous levels (must fall to <36mg/dL), and the brain secretes GH in addition to ACTH to try and raise the blood sugar level. Its use is not necessary. 91% of persons with an IGF-1 level below the laboratory’s reference range will also fail the IST. A combination of low IGF-1 and low overnight urinary GH secretion can reliably diagnose GH deficiency. (review paper about need for multiple hormonal deficiencies)21 The IGF-1 level is recommended as the best way to monitor GH treatment, and it’s considered the best indicator of GH secretion, yet guidelines fail to use it as an indicator of actual GH secretion on a daily basis. So why the failure to rely on the IGF-1 to diagnose GH deficiency? One must not make the diagnosis of GH deficiency before replacing other hormones that are low. Thyroid, testosterone, DHEA, and estradiol optimization all increase IGF-1 levels and presumably GH secretion. What is an adequate IGF-1 level? What is an optimal IGF-1 level? How have laboratories determined their reference ranges? Why do the ranges include such low level that many persons with severe GH deficiency are with the RR? Have they simply inlcuded all test done at their laboratory by a doctors order? As with other hormones, one must try to find realistic reference range by searching the literature. See the chart below from a study of 404 volunteers from the staff and relatives of a university medical deparement. All persons were excluded from the study by these criteria: “Exclusion criteria were: 1) personal history of cardiovascular diseases or pituitary diseases as reported in interviews with individual subjects; 2) previous or current treatments with drugs known to interfere with glucose or lipid metabolism or to influence BP; 3) previous treatment with corticosteroids for longer than 2 weeks; 4) previous or current treatment with estrogens or testosterone for longer than 12 weeks; and 5) smoking of more than 15 cigarettes/day and lcohol abuse (more than three glasses of wine/day). Subjects with type 1 diabetes mellitus have been also excluded. Smoking was stratified into the following: 1) non-smokers, 2) ex-smokers, and 3) mild smokers (up to 15 cigarettes/day). Subjects with chronic severe liver and renal dysfunction were also excluded.”22 In addition, all subjects found to be obese or with diabetes were excluded from the determination of the RR. Serum IGF1 levels by IRMA after ethanol extraction using Diagnostic System Laboratories Inc. (Webster, TX, USA). Using the mean and 1 standard deviation, we can compare the study subjects to the kit manufacturers ±2S.D range: Age, yrs Kit Male ng/L Kit Female <20 LabCorp M/F RR Averaged* 144-497 180–625 151–530 21-30 31-40 41-50 116-343 112-296 98-259.5 118–475 102–400 100–306 118–450 100–390 96–288 Male subject 2 S.D range 247-439 mean 343.0±48.0 SD 170- 405 Mean 287.8±58.4 SD Female subject 2 S.D range 213.1-373.5 Mean 293.3±40.1 SD 191.5-377.5 Mean 284.5±46.5 SD 139.4-309.8 148-290.4 51-60 84-231.5 Mean 224.6±42.6 SD Mean 219.2±35.6 SD 95–270 90–250 61-70 72-206 90.6-227.4 89-198.6 88–250 82–200 Mean159.0±34.2 Mean 143.8±27.4 SD >70 62-183 78–200 68–188 *Labcorp lists RRs in 5 year increments, for any decade the two 5 yr. RRs for that decade were averaged. LabCorp uses a different kit and technology in performing their IGF-1 tests. They have taken their reference ranges directly from the kit manufacturer, Nichols Institute Diagnostics. The lower limits found by Nichols correlate well with the lower limits of the Diagnostic System Laboratories Inc. kit, but DSL has higher upper limits, 30% higher in the 21-40 and, 13% higher 41-60 age group. The study subjects were only as young as 18yr, which explains the lower upper limits for the <20 yr. range. Notice that throughout, the screened study subjects had much higher – 2SD cut off ranges than the kit manufacturer. In the important middle-aged group of 41-60yrs, the screened male subjects had lower IGF-1 limits of 139.4, compared to only 97.5ng/ml for the kit range. The lower limit in the study group for 21-40yr males was 170, compared to an average of 110 for the kit. One must wonder who the kit manufacturer had studied, and what screening technique was used. But it gets much more interesting. In another study using this same assay, reference ranges, and same control subjects as above, the IGF-1 levels and GHR+arginine stimulation test results were compared with those of patients with suspected GH deficiency. Colao et al. found that in the patients, an IGF-I SDS (standard deviation score) of -1.00 or less was diagnostic of GHD in 99.5% who had two or more pituitary deficits. A IGF-I SDS of -1.50 or less had 100% specificity independently from the number of pituitary deficits. 23 Meaning that every person with suspected growth hormone deficiency based on signs and symptoms who had an IGF-1 that was 1.5 standard deviations below the mean level of the controls, and stimulation-testing verified severe growth hormone deficiency. The -1.5 SD cutoff is quite a bit higher than the -2.0 SD cutoff reported by all laboratories. Using -1.5 SD as the cutoff for diagnosing GH in a person with signs and symptoms and no other deficits in pituitary hormones, we get the lower limit cut-offs seen below. However, in my practice, most of these patients do have other pituitary deficits. Many how hypothyroidism with low-normal free T4 and free T3 levels and a normal TSH. Many others have inadquate cortisol levels or effects by testing or by symptoms and response to therapy. Most males have LH deficiency as they age causing inadequate free testosterone levels. So we can produce the following chart for the diagnosis of GH deficiency without the use of stimulation testing. Age yrs <20 21-40 41-60 >60 IGF-1 – 1.5 S.D. Males, No deficits 271 200.2 160.7 107.7 IGF-1 – 1.5 SD Females No deficits 233.2 214.8 165.8 102.7 IGF-1 – 1.0 S.D. Males, ≥2 deficits 295 229.4 182 124.8 IGF-1 – 1.0 SD Females ≥2 deficits 253.2 238 183.6 116.4 4. Is GH Restoration Safe? GH does increase cell proliferation and prevent programmed cell death (apoptosis). These are the mechanisms by which it maintains tissue integrity. It is feared that these effects could increase the risk of cancers occurring or surviving in a person. Acromegaly is a condition caused by grossly excessive GH production by a tumor of the GH producing cells in the pituitary. The GH secretion is several times the normal amount. Some studies have shown higher incidences of some cancers in people with this disorder. 24 GH replacement in GH-deficient adults at the physiological dose of 0.2mg/day produced the usual improvements in bone and muscle mass, reduced levels of total and LDL (bad) cholesterol. On the negative side, the GH therapy raised insulin levels (from 9 to 17mIU/L) and insulin resistance. 25 GH does have blood-sugar raising effects. It is one of the hormones that the body secretes to maintain blood sugar. Blood sugar levels did not change. A longer term study found an increase in fasting glucose from 79 to 87mg/dL after 1 and 5 years. Insulin resistance (HOMA-IR) increased from 2.1 to 2.5 after one year, but decreased to 2.3 by 5 years. The authors suggest that the long-term reduction in body fat percentage may overcome the negative influence of GH on glucose metabolism.26 This early increase in insulin resistance, followed by a return to baseline has been seen in a 5 yr. study.27 Indeed, studies of person with long-term GH deficiency show that they have more insulin resistance and higher fasting blood sugars.28 in the long-run, GH sufficiency prevents insulin resistance by maintaining muscle mass and minimizing body fat. 5. The Treatment of GH Deficiency Occasionally a study on GH replacement is done in which “side effects” are seen and GH replacement is presented as risky. In one such study, excessive doses of GH were given to older adults using a nonphysiological 3 times/week schedule. These pharmaceutically-minded physicians do not understand that hormones are not drugs and therefore cannot cause “side effects”. They are natural to the body and have effects. Only excessive doses can cause excessive effects! Persons may not tolerate growth hormone if they have insufficient cortisol or thyroid levels. A reduction in cortisol effects produces fatigue, aches, anxiety, and irritability. A GH-induced reduction in thyroid effects produces fatigue. Some studies of GH therapy in hypopituitary patient do not show many of the expected benefits29f or the reason that such patients have multiple hormone deficiencies that are either not treated, or are treated inadequately or wrongly. They often receive no DHEA , even though their levels are undetectable. They are given levothyroxine in grossly insufficient doses, they are given prednisone instead of cortisol. Sex hormones are not replaced, are under-replaced, are are ill-replaced. Growth hormone replacement is beneficial in cases of heart failure. 30 IGF-1 levels stabilize at 3 weeks after a GH dosage change.31 7000IU of Vit D3 weekly can raise IGF-1 by 30ng/ml in GH-deficient persons.32 1 Bennett RM. Adult growth hormone deficiency in patients with fibromyalgia. Curr Rheumatol Rep. 2002 Aug;4(4):306-12. 2 Caufriez A, Leproult R, L'hermite-Balériaux M, Moreno-Reyes R, Copinschi G. A potential role for endogenous progesterone in modulation of growth hormone, prolactin and thyrotropin secretion during normal menstrual cycle. Clin Endocrinol (Oxf). 2009 Oct;71(4):535-42. 3 Caufriez A, Golstein J, Tadjerouni A, Bosson D, Cantraine F, Robyn C, Copinschi G. Modulation of immunoreactive somatomedin-C levels by sex steroids. Acta Endocrinol (Copenh). 1986 Jun;112(2):284-9. 4 Arvat E, Ceda G, Ramunni J, Lanfranco F, Aimaretti G, Gianotti L, Broglio F, Ghigo E. The IGF-I response to very low rhGH doses is preserved in human ageing. Clin Endocrinol (Oxf). 1998 Dec;49(6):757-63. 5 Colao A, Di Somma C, Filippella M, Rota F, Pivonello R, Orio F, Vitale G, Lombardi G. Insulin -like growth factor-1 deficiency determines increased intima-media thickness at common carotid arteries in adult patients with growth hormone deficiency. Clin Endocrinol (Oxf). 2004 Sep;61(3):360-6. 6 Cenci MC, Conceição FL, Soares DV, Spina LD, Brasil RR, Lobo PM, Michmacher E, Vaisman M. Impact of 5 years of growth hormone replacement therapy on cardiovascular risk factors in growth hormone-deficient adults. Metabolism. 2008 Jan;57(1):121-9. 7 Colao A, Di Somma C, Filippella M, Rota F, Pivonello R, Orio F, Vitale G, Lombardi G. Insulin-like growth factor-1 deficiency determines increased intima-media thickness at common carotid arteries in adult patients with growth hormone deficiency. Clin Endocrinol (Oxf). 2004 Sep;61(3):360-6. 8 Colao A, Di Somma C, Cascella T, Pivonello R, Vitale G, Grasso LF, Lombardi G, Savastano S. Relationships between serum IGF1 levels, blood pressure, and glucose tolerance: an observational, exploratory study in 404 subjects. Eur J Endocrinol. 2008 Oct;159(4):389-97. 9 Juul A, Scheike T, Davidsen M, Gyllenborg J, Jørgensen T. Low serum insulin-like growth factor I is associated with increased risk of ischemic heart disease: a population-based case-control study. Circulation. 2002 Aug 20;106(8):939-44. 10 Laughlin GA, Barrett-Connor E, Criqui MH, Kritz-Silverstein D. The prospective association of serum insulin-like growth factor I (IGF-I) and IGF-binding protein-1 levels with all cause and cardiovascular disease mortality in older adults: the Rancho Bernardo Study. J Clin Endocri nol Metab. 2004 Jan;89(1):114-20. 11 Vasan RS, Sullivan LM, D'Agostino RB, Roubenoff R, Harris T, Sawyer DB, Levy D, Wilson PW. Serum insulin-like growth factor I and risk for heart failure in elderly individuals without a previous myocardial infarction: the Framingham Heart Study. Ann Intern Med. 2003 Oct 21;139(8):642-8. 12 Johnsen SP, Hundborg HH, Sørensen HT, Orskov H, Tjønneland A, Overvad K, Jørgensen JO. J Clin Endocrinol Metab. 2005 Nov;90(11):5937-41. 13 Bohdanowicz-Pawlak A, Szymczak J, Bladowska J, Bednarek-Tupikowska G, Bidzinska B, Milewicz A. Risk factors of cardiovascular disease in GH-deficient adults with hypopituitarism: a preliminary report. Med Sci Monit. 2006 Feb;12(2):CR75-80. 14 Caidahl K, Eden S, Bengtsson BA. Cardiovascular and renal effects of growth hormone. Clin Endocrinol (Oxf). 1994 Mar;40(3):393-400. 15 Aberg ND, Brywe KG, Isgaard J. Aspects of growth hormone and insulin-like growth factor-I related to neuroprotection, regeneration, and functional plasticity in the adult bra in. ScientificWorldJournal. 2006 Jan 18;6:53-80. 16 Arwert LI, Veltman DJ, Deijen JB, van Dam PS, Drent ML. Effects of growth hormone substitution therapy on cognitive functioning in growth hormone deficient patients: a functional MRI study. Neuroendocrinology. 2006;83(1):12-9. 17 Ceda GP, Dall'Aglio E, Maggio M, Lauretani F, Bandinelli S, Falzoi C, Grimaldi W, Ceresini G, Corradi F, Ferrucci L, Valenti G, Hoffman AR. Clinical implications of the reduced activity of the GH-IGF-I axis in older men. J Endocrinol Invest. 2005;28(11 Suppl Proceedings):96-100. 18 Agha A; Walker D; Perry L; Drake WM; Chew SL; Jenkins PJ; Grossman AB; Monson JP Unmasking of central hypothyroidism following growth hormone replacement in adult hypopituitary patients. Clin Endocrinol (Oxf). 2007 Jan;66(1):72-7. 19 Baum HB, Biller BM, Finkelstein JS, Cannistraro KB, Oppenhein DS, Schoenfeld DA, Michel TH, Wittink H, Klibanski A. Effects of physiologic growth hormone therapy on bone density and body composition in patients with adult-onset growth hormone deficiency. A randomized, placebocontrolled trial. Ann Intern Med 1996 Dec 1;125(11):932-4. 20 Biller BM, Sesmilo G, Baum HB, Hayden D, Schoenfeld D, Klibanski A. Withdrawal of long -term physiological growth hormone (GH) administration: differential effects on bone density and body composition in men with adult-onset GH deficiency. J Clin Endocrinol Metab. 2000 Mar;85(3):970-6. 21 Bates AS, Evans AJ, Jones P, Clayton RN. Assessment of GH status in adults with GH deficiency using serum growth hormone, serum insulin-like growth factor-I and urinary growth hormone excretion. Clin Endocrinol (Oxf). 1995 Apr;42(4):425-30. 22 Colao A, Di Somma C, Cascella T, Pivonello R, Vitale G, Grasso LF, Lombardi G, Savastano S. Relationships between serum IGF1 levels, blood pressure, and glucose tolerance: an observational, exploratory study in 404 subjects. Eur J Endocrinol. 2008 Oct;159(4):389-97. 23 Colao A, Di Somma C, Savastano S, Rota F, Savanelli MC, Aimaretti G, Lombardi G. A reappraisa l of diagnosing GH deficiency in adults: role of gender, age, waist circumference, and body mass index. J Clin Endocrinol Metab. 2009 Nov;94(11):4414-22. 24 Baris D, Gridley G, Ron E, Weiderpass E, Mellemkjaer L, Ekbom A, Olsen JH, Baron JA, Fraumeni JF Jr. Acromegaly and cancer risk: a cohort study in Sweden and Denmark. Cancer Causes Control. 2002 Jun;13(5):395-400. 25 Boguszewski CL, Meister LH, Zaninelli DC, Radominski RB. One year of GH replacement therapy with a fixed low-dose regimen improves body composition, bone mineral density and lipid profile of GH-deficient adults. Eur J Endocrinol. 2005 Jan;152(1):67-75. 26 Giavoli C, Porretti S, Ronchi CL, Cappiello V, Ferrante E, Orsi E, Arosio M, Beck-Peccoz P. Longterm monitoring of insulin sensitivity in growth hormone-deficient adults on substitutive recombinant human growth hormone therapy. Metabolism. 2004 Jun;53(6):740 -3. 27 Cenci MC, Conceição FL, Soares DV, Spina LD, Brasil RR, Lobo PM, Michmacher E, Vaisman M. Impact of 5 years of growth hormone replacement therapy on cardiovascular risk factors in growth hormone-deficient adults. Metabolism. 2008 Jan;57(1):121-9. 28 Bohdanowicz-Pawlak A, Szymczak J, Bladowska J, Bednarek-Tupikowska G, Bidzinska B, Milewicz A. Risk factors of cardiovascular disease in GH-deficient adults with hypopituitarism: a preliminary report. Med Sci Monit. 2006 Feb;12(2):CR75-80. 29 Spielhagen C, Schwahn C, Möller K, Friedrich N, Kohlmann T, Moock J, Kołtowska-Häggström M, Nauck M, Buchfelder M, Wallaschofski H. The benefit of long-term growth hormone (GH) replacement therapy in hypopituitary adults with GH deficiency: Results of the German KIMS database. Growth Horm IGF Res. 2010 Nov 18. [Epub ahead of print] 30 Bocchi EA, Massuda Z, Guilherme G, Carrara D, Bellotti G, Mecelin A, Rodriguez Sobrinho CR, Ramires JF. Growth hormone for optimization of refractory heart failure treatment. Arq Bras Cardiol 1999 Oct; 73(4):391-8. 31 Sigurjonsdottir HA, Andrew R, Stimson RH, Johannsson G, Walker BR. Lack of regulation of 11betahydroxysteroid dehydrogenase type 1 during short-term manipulation of GH in patients with hypopituitarism. Eur J Endocrinol. 2009 Sep;161(3):375-80. 32 Ameri P, Giusti A, Boschetti M, Bovio M, Teti C, Leoncini G, Ferone D, Murialdo G, Minuto F. Vitamin D increases circulating IGF1 in adults: potential implication for the treatment of GH deficiency. Eur J Endocrinol. 2013 Oct 21;169(6):767-72.