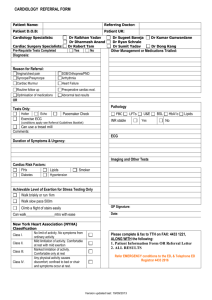
Risk Stratification Based on the ACC/AHA Guidelines
advertisement

Non-ST-Segment Elevation Acute Coronary Syndromes: Risk Stratification Based on the ACC/AHA UA / NSTEMI Guidelines ED Risk Stratification for Chest Pain For the past 20 years . . . In 2002: Does this patient need fibrinolytic therapy? Should this patient get antithrombin and anti-platelet agents? Can I safely send this patient home? R/O MI ED CCU Cath Lab Risk Stratification for Chest Pain Three levels of risk stratification are pertinent to the ED: Low, intermediate, or high risk that ischemic symptoms are a result of CAD Low, intermediate, or high risk of short-term death or nonfatal MI from ACS Dynamic, ongoing risk-oriented evaluation of low- or intermediate-risk patients for “conversion” to high-risk status that is linked to intensity of treatment Initial Risk Stratification Scheme Chest Pain History, Physical EKG STEMI UA/NSTEMI/ High Risk Mod Risk Low Risk Definite Non-Cardiac Risk Stratification Tools in the ED • History and Physical • Standard ECG and Non-standard ECG leads Cardiac Biomarkers • Troponin I or T, CK-MB, myoglobin Predictive Indices / Schemes Non-Invasive Imaging Studies Echocardiogram Exercise testing Technetium-99m-sestamibi: stress and rest Initial Evaluation Risk Stratification (1) I IIa IIb III Early risk stratification by symptoms, physical findings, ECG, cardiac markers 12-lead ECG within 10 min for ongoing pain, or ASAP if pain has resolved at presentation Cardiac markers, Troponins and CK-MB, for initial assessment Monitoring, repeat ECG and cardiac markers in 6-12 hours, if initial results normal Initial Evaluation Risk Stratification (2) I IIa IIb III If <6 hours after symptom onset, add early myoglobin or CK-MB to troponin C-reactive protein, other markers of inflammation Total CK, SGOT, HBDH, LDH Clinical Assessment (1) Rapid, focused evaluation Decisions based on this evaluation have substantial clinical and economic consequences Are the symptoms a manifestation of ACS? If so, what is the prognosis? Identify signs of life-threatening instability Triage to most appropriate area Typically an ED or chest pain unit Clinical Assessment (2) Risk status determined in the ED by: Assessment of anginal symptoms Careful physical examination Electrocardiogram Cardiac biomarkers CAD risk factors Illicit drug use Initial risk stratification assignment drives pace of subsequent evaluation and treatment Clinical Assessment (3) High-risk features apparent in the ED: Accelerated pattern of angina Ongoing rest pain > 20 min Signs of CHF Hemodynamic instability Arrhythmias - Atrial or ventricular Advanced age (> 75 years) Ischemic ECG changes Elevated cardiac markers Electrocardiogram Carries diagnostic and prognostic value Especially valuable if captured during pain ST-segment depression or transient ST-segment elevation are primary ECG markers of UA/NSTEMI 75% of patients with + CK-MB do not develop Q waves Differentiation between UA and NSTEMI relies upon positive biomarkers Inverted T-waves suggestive of ischemia, particularly with good chest pain story Six-Month Mortality by Baseline ECG Findings GUSTO-IIb Results 10% ST % Mortality 8% ST 6% 4% NS ST-Ts 2% 0% 0 30 60 90 120 Days from Randomization Savonitto, JAMA 1999 150 180 Biomarkers: CK/CKMB Until recently the principal serum marker used in evaluation of ACS despite known limitations: Low levels in healthy persons limits specificity MB band may be elevated in skeletal muscle damage Different MB isoforms exist in myocardium (MB2) and in plasma (MB1), and differentiating assay is not widely available Biomarkers: Troponins Very useful in diagnosis and prognosis of ACS Normally not detectable in blood of healthy persons; cTnI or cTnT can be positive with negative CK-MB = “minor myocardial damage” Predictive of MI and death when elevated, independent of CK-MB levels Elevated troponins validated as a predictor of enhanced treatment benefit from aggressive therapies (LMW heparins, GP IIb/IIIa inhibitors, early invasive strategy) Troponin as a Marker of Increased Risk in ACS 40% 34% Death or MI 30% Troponin + Troponin - 30% 23% 22% 19% 20% 12% 11% 12% 10% 2% 4% 19% 6% 4% 1% 6% 0% 0% Hamm (1992) FRISC (1996) TRIM (1999) Pettijohn (1997) Hamm (1997) Hamm (1997) Polanczyk Galvanni (1998) (1997) Long Term Survival and Troponin-T Status GUSTO-IIa Results 1-Year Mortality Rates: Troponin-T Positive: 14% Troponin-T Negative: 5% 100% Survival 95% TnT - 90% p < 0.001 85% TnT + 80% 0 50 100 150 200 250 Days from Randomization 300 350 Biomarkers: Myoglobin Utility limited by release kinetics (early) and by lack of cardiac specificity Isolated elevation of myoglobin 4-8 hours after pain onset with a a non-diagnostic ECG must be supplemented by a more cardiac-specific marker Sufficiently sensitive that a negative myoglobin 4-8 hours after pain onset is useful in excluding myocardial necrosis Integration of Biomarkers with Clinical History Time since symptom onset should be a factor in marker selection and in repeat assay strategy Elevated serum levels of troponins persist for 7-14 days after initial release Delta values, as close as 2 hours apart, may be sufficiently sensitive to assist with serial evaluations Serial cardiac marker strategy not specified Serial Cardiac Markers Serial Testing in 309 Patients with Suspected MI Sensitivity Myoglobin CK-MB (mass) Troponin T 100% 75% 50% 25% 0% 3 4 5 6 Hours After Symptom Onset 8 12 Winter, Circulation, 1995 Biomarkers: Bedside Testing Consideration of bedside marker assay recommended when hospital lab turnaround time > 30-60 minutes Ready-for-use availability must be balanced against need for stringent QC and training of ED personnel, CLIA concerns, political hazards, etc Prognostic value limited because many assays are qualitative, not quantitative “Vein-to-Brain” Reporting Times for Cardiac Markers - St. Agnes Hospital Bedside Test (mean=15 mins) Laboratory Test (mean=128 mins) "Vein-to Brain" Reporting Times (mins) 180 160 140 120 100 80 60 40 20 0 Test Type Christenson R: Md Med 2001 Spring:Suppl:98-103 n = 939 SD = 46.74 Distribution of Reporting Times for Cardiac Markers - St. Agnes Hospital 284 mins = Latest Reporting Time 95th percentile (201.3 mins) 75th percentile (147 mins) 50th percentile (Median , 117 mins) Range of Lab Reporting Times 25th percentile 5th percentile (85 mins) (62.6 mins) 40 mins = Earliest Reporting Time Christenson R: Md Med 2001 Spring:Suppl:98-103 Noninvasive Studies Guidelines do not consider use of these tests in the ED setting, although: Many EDs now use rest sestamibi scanning in the risk stratification process Stress testing used after patients have “ruled out” Reality dictates that appropriate provocative testing often not likely after patient leaves ED ED is the “first, last, and best shot” at intervening in patients with risk concerns Predictive Indices - Risk Scores in the ED Combine clinical history, physical exam findings, ECG signs of ischemia, and cardiac marker results PURSUIT and TIMI Risk Scores Therapies such as LMW heparin and GP IIb/IIIa inhibitors have greater benefit in patients with higher risk scores Have not been tested prospectively in the ED Risk scores not specifically recommended by the ACC/AHA Guidelines Immediate Management I IIa IIb III Classify as non-cardiac, chronic stable angina, possible ACS, or definite ACS Evaluate for immediate reperfusion therapy if definite ACS and ST-segment present Pharmacological or exercise stress test, if possible ACS and serial biomarkers and ECGs are normal Admit pts with definite ACS, ongoing pain, biomarkers, new ST or deep T-wave inversion, abnormal hemodynamics, or (+) stress test The “Key” to Risk Stratification Link ongoing evaluation of risk to changes in intensity of therapy Develop risk stratification schemes that reflect capabilities of ED and needs/preferences of cardiologists Develop treatment pathways that provide for independent response of emergency physicians to recognition of higher risk levels The “Rallying Cry” for CRUSADE . . . A seamless transition of optimal care—diagnostic and therapeutic—from the ED to the Cardiology Service . . . . . . starts with a successful risk stratification strategy