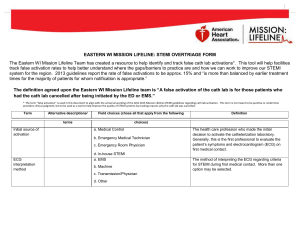
direct referral to the cath lab
advertisement

New York City Direct Referral to Catheterization Lab STEMI Notification & Transportation Protocol What is Mission: Lifeline? • Mission: Lifeline is the American Heart Association's systems-based approach to improving emergency cardiac care for all Americans. • M:L implements quality improvement strategies based on evidence-based guidelines and forms partnerships across the system of care: – community – emergency medical service – emergency department (referral and receiving centers) – inpatient care – post-discharge 3/14/2016 ©2012, American Heart Association 2 Ideal System of Care 3/14/2016 ©2012, American Heart Association 3 New York City Mission: Lifeline TIMELINE • New York City chosen as one of 20 sites nationwide to participate in pilot project with Duke Clinical Research Institute and the American Heart Association • Project Timeline: July 2012-December 2013 PROJECT OBJECTIVES • Establish regional standards for emergency cardiovascular care • Lower mortality by improving timely treatment for STEMI patients • Create sustainable system for treating cardiovascular emergencies including STEMI, cardiac arrest, stroke, aortic dissection 3/14/2016 ©2010, American Heart Association 4 Purpose of Protocol Direct notification to receiving hospital ED and direct delivery of certain STEMI patients to receiving hospital catheterization labs in order to expedite PCI treatment and continue to provide the highest level of care and transportation. 3/14/2016 ©2010, American Heart Association 5 Direct to Cath Lab Criteria INCLUSION CRITERIA • EXCLUSION CRITERIA Ongoing chest discomfort or upper • LBBB body discomfort felt to be ischemic in • Intubated origin • Respiratory failure or CHF requiring • Symptom duration of <12 hours • ST elevation of at least 2 mm in two or • Cardiac arrest more contiguous leads • DNR/DNI Absence of other issues believed to • On-going Hospice care • Obvious active severe bleeding • Head or other serious trauma (meets • require further evaluation and treatment (see exclusions) intubation trauma center criteria) 3/14/2016 ©2010, American Heart Association 6 Direct to Cath Lab Protocol EMS 1. EMS transmits ECG to OLMC MD FDNY OLMC 2. OLMC MD confirms ST elevation and verifies direct referral criteria with EMS 3. OLMC notifies and transmits ECG and patient demographic info to PCI center ED Receiving Hospital ED (Meet, greet, and escort EMS) 4. ED activates STEMI pager, including information that patient is Direct Referral to Cath Lab and ETA 5. Cath lab calls ED to confirm availability to proceed 3/14/2016 Cath Lab 6. Fellow, resident, or member of cath lab team greets EMS and patient at ED entrance and escorts ©2010, American Heart Association 7 them to cath lab Pre-Notification Protocol • FDNY will transmit the ECG and make a phone call (providing the necessary demographic information to allow for preregistration) for all patients with ischemic type chest discomfort and ST segment elevation >1mm. • For all cases with >2 mm ST segment elevation who meet the agreed upon criteria for “direct referral to the cath lab” FDNY will use specific language stating that the patient qualifies for “direct transport to the cath lab”. • Hospitals will then preactivate the cath lab and follow their procedures on how to expedite the patient to the cath lab. Note: If the field ECG cannot be transmitted from the field to the hospital, FDNY will still call a “direct referral to the cath lab” if the patient meets the criteria. (Note: the field EMS personnel will still communicate verbally with FDNY On-Line Medical Control MDs who will make the determination on the case). 3/14/2016 ©2010, American Heart Association 8 8 Notes • The hospital needs to escort EMS to the hospital’s Cath Lab on the EMS stretcher. EMS will not take any patient directly from the field to a PCI Center’s cath lab. • Hospital staff must meet EMS within five minutes of arrival and the total time spent awaiting an escort is not to exceed ten minutes. • If no staff is available within 10 minutes, the patient shall be delivered to ED staff. • With the availability of the transmitted field or hard copy ECG, time should not be wasted to obtain an ECG at the time of arrival. • If the cath lab is closed, the patient will then reside in the ED. • Hospital “arrival time” is the time the patient is brought to the ED by EMS. • If the field ECG cannot be transmitted, FDNY will still call a “direct referral to the cath lab” if the patient meets the criteria. 3/14/2016 ©2010, American Heart Association 9 Questions? Zainab Magdon-Ismail, Ed.M., MPH Vice President, Quality Improvement Initiatives American Heart Association 518-229-5483 (cell) Zainab.Magdon@heart.org Glenn Asaeda, MD Chief Medical Director Fire Department of New York asaedag@fdny.nyc.gov 3/14/2016 10